20.1 Introduction
Diabetes mellitus (DM) is a metabolic disorder with a multifactorial etiology. It is characterized by chronic hyperglycemia and affects metabolism of carbohydrates, protein and fats. The pathophysiology of DM centers on impaired insulin secretion/or impaired insulin action. Subjects with DM present with varied symptoms such as polyuria, polydypsia and polyphagia with weight loss. Hyperglycemia may remain undetected as the disease may be asymptomatic causing vascular damage even before the detection of the disease. Long-term DM leads to a series of metabolic disturbances causing macro-vascular and microvascular pathology. Microvascular complications associated with DM include retinopathy, nephropathy and neuropathy. People with DM are at an increased risk of cardiovascular, cerebrovascular and peripheral vascular diseases.
20.2 Classification of diabetes
The recent classification encompasses both clinical stages and etiological types of DM and other categories of hyperglycemia. The terms insulin-dependent diabetes mellitus (IDDM) and noninsulin-dependent diabetes mellitus (NIDDM) are no longer used. The etiological classification is shown in Table 20.1.
Impaired glucose tolerance
The class impaired glucose tolerance (IGT) is a stage of impaired glucose regulation, since it can be observed in any hyperglycemic disorder, and is itself not DM.
Type 1 diabetes
Type 1 DM is characterized by reduced insulin levels (insulinopenia) due to β-cell destruction. Patients require insulin for survival. In the absence of exogenous insulin, they develop ketoacidosis, coma and death.
Type 2 diabetes
Type 2 DM is the most common form of DM and is characterized by impaired insulin action and insulin secretion. Both of these defects are present in clinical DM. Multiple and varied reasons for the development of these abnormalities have been identified.
Table 20.1 Etiological classification of disorders of glycemia
| Type 1 | Characterized by partial or total failure of insulin production by the β-cells of the pancreas. Causative factors remain poorly understood, but certain viruses, autoimmune disease and genetic factors may all contribute |
| Type 2 | Characterized by insulin resistance, where insulin is produced but in amounts that are insufficient or in an ineffective form. Strong genetic links with this form of diabetes and its development are closely linked with obesity |
| Other specific types | Genetic defects of β-cell function Genetic defects in insulin action Diseases of the exocrine pancreas Endocrinopathies Drug or chemical induced Infections Uncommon forms of immune-mediated diabetes Other genetic syndromes sometimes associated with diabetes |
| Gestational diabetes | A form of diabetes that develops during pregnancy. Most, but not all, cases resolve after delivery |
Type 2 DM also has a multifactorial etiology. The majority of patients are noninsulin dependent and mostly have adult-onset DM. In type 2 DM insulin resistance is common, with relative insulinopenia and occasionally requiring insulin in times of stress. Obesity and central obesity are commonly seen in type 2 diabetics. Ketoacidosis is uncommon and, if seen, is related to stress or other intercurrent illness. Patients are also prone to microvascular and macrovascular complications. Etiological factors include genetic factors, age, obesity and lack of physical activity.
Gestational diabetes
Gestational DM is carbohydrate intolerance resulting in hyperglycemia of variable severity with onset or first recognition during pregnancy. The definition applies irrespective of whether or not insulin is used for treatment or the condition persists after pregnancy. The glucose intolerance may precede pregnancy, but has been previously unrecognized.
The metabolic syndrome or syndrome X
A cluster of abnormalities, namely hyperglycemia, hypertension, central obesity, dyslipidemia and insulin resistance, occurs frequently. This clustering of risk factors for cardiovascular diseases is termed syndrome X, the insulin resistance syndrome or the metabolic syndrome. Epidemiological studies confirm that this syndrome occurs commonly in a wide variety of ethnic groups, including Europeans, African–Americans, Mexican Americans, Asian Indians and Chinese, Australian Aborigines, Polynesians and Micronesians. The management of people with hyperglycemia and other features of the metabolic syndrome should not only focus on blood glucose control, but also include strategies for reduction of the other cardiovascular disease risk factors.
20.3 Diagnosis of diabetes
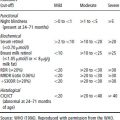
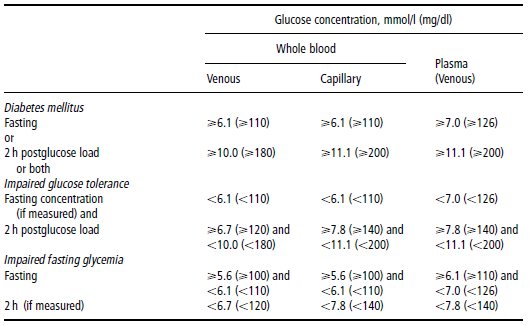
Standardization of the criteria for diagnosis and classification of DM proposed by the National Diabetes Data Group of the USA (NDDG) and the World Health Organization (WHO) expert committee brought in a certain degree of uniformity to the global studies on this metabolic disorder. An oral glucose tolerance test (OGTT) with a 75 g glucose load is used to distinguish between DM and non-DM. Table 20.2 shows the diagnostic criteria.
There is an underestimation of DM prevalence when the fasting plasma glucose (FPG) criterion is used. In the US National Health and Nutrition Examination Survey (NHANES) III population study, the prevalence of undiagnosed DM was 6.34% by the WHO criteria (2 h), but only 4.4% if diagnosis was based only on the FPG cut-off of 126 mg/dl (7.0 mmol/l) or above. The Diabetes Epidemiology: Collaborative Analysis of Diagnostic Criteria in Europe (DECODE) study group, which analyzed the data from 16 European countries, found that there was an underestimation of DM if the FPG criterion was used, with a concordance of only 28%. Sensitivity of the FPG for diagnosis of diabetes was also low in Asian populations.
Mode of diagnosis
- Symptoms of DM, such as thirst and polyuria, and a random plasma glucose ≥ 200 mg/dl (11.1 mmol/l)
- or FPG ≥ 126 mg/dl (7.0 mmol/l)
- or 2h plasma glucose ≥ 200 mg/dl (11.1 mmol/l) during an OGTT
- for population screening purposes, the fasting or 2 h value after 75 g oral glucose may be used.
Table 20.2 Values for diagnosis of diabetes mellitus and other categories of hyperglycemia
Source: WHO (1998). Reproduced with permission from the WHO.
Pregnant women who meet the WHO criteria for DM or IGT are classified as having gestational DM. Screening for gestational DM is unnecessary in women younger than 25 years of age who are at low risk. Glucose tolerance should be reclassified by a 75 g load OGTT, 6 weeks or more after delivery. The American Diabetes Association (ADA) recommends a screening by measuring plasma glucose concentration 1 h after a 50g oral glucose load between 24 and 28 weeks of gestation. If the glucose concentration is at least 7.8 mmol/l (140mg/dl), a full 3h OGTT should be performed. Any two of the four plasma glucose values obtained during the test meeting or exceeding the values shown below indicate a diagnosis of gestational DM:
| Time | mg/dl | mmol/L |
| fasting | 95 | 5.3 |
| 1h | 180 | 10.0 |
| 2h | 155 | 8.6 |
| 3h | 140 | 7.8 |
The glycosylated hemoglobin (HbA1c) measurement is an index of glycemic status over the past 2–3 months. It is recommended as a tool for monitoring glycemic control.
20.4 Risk factors for the development of diabetes
Type 2 DM is a multifactorial disease with equally strong genetic and environmental components contributing to its development. Some of these factors can be modified by lifestyle changes, other factors cannot.
Genetic factors
Evidence for a genetic component comes from the increased concordance of DM in monozygotic twins, a high prevalence in the offspring of diabetic parents and a high prevalence in certain ethnic groups. Associations of DM with many candidate genes have been identified in different populations, but none has been shown to be the major gene involved in the development of the disorder. Type 2 DM is a polygenic disorder, and no clear relationship is described with human leukocyte antigen (HLA) genes. Maturity-onset diabetes in the young (MODY) is a monogenic form of type 2 DM with an early age of onset, less than 25 years. It has an autosomal dominant inheritance and mutations have been described in at least five genes. Another genetic variant is maternally inherited deafness in diabetes mellitus (MIDDM), which has characteristics of both type 1 and type 2 DM. Sensory neural deafness is associated with an early onset of DM and this form is characterized by a strict maternal inheritance. Only a daughter can transfer the disease to her progeny, although both genders are affected equally.
Thrifty genotype and thrifty phenotype
The thrifty genotype hypothesis was put forward by Neel in 1962, and proposes that certain populations exposed to cycles of starvation and times of plenty have been benefited by a thrifty gene which has helped them to store a high proportion of energy intake as fat during times of plenty. It could be used during times of famine. This was proposed to be common among the hunter–gatherer populations. During the process of modernization, when these individuals with a thrifty genotype are confronted with a continuous supply of energy and reduced physical activity, the condition is favorable for development of DM and IGT. Hyperinsulinemia is considered to be a mechanism of preferential energy storage, which has become a disadvantage in modern populations. Such a phenomenon is observed in cases of Pacific islanders, Native Americans and Asian Indians.
In recent years a different hypothesis of a thrifty phenotype has gained significant importance. Barker’s hypothesis (see Chapter 18) states that fetal and childhood malnutrition, by programming metabolism, predisposes to chronic diseases in adulthood such as hypertension, coronary heart disease and type 2 DM. A thrifty phenotype has been proposed in which inadequate fetal nutrition programs lead to the development of insulin resistance in adulthood. It may well be that such a phenomenon is more relevant in the developing countries where malnutrition is a major health problem.
Environmental risk factors
Epidemiological studies from different parts of the world have shown that the major environmental risk factors for DM are:
- age
- obesity and central obesity
- insulin resistance
- dietary factors
- physical inactivity
- urbanization and modernization.
Age
Aging is an important risk factor for DM. In all of the epidemiological studies in different populations, the prevalence of DM shows an age-specific increase. In the European population, the age of onset of DM is generally in the region of 50–60 years, but it is significantly lower in the Native American and Asian Indian populations, who have a high prevalence of DM.
Obesity and central obesity
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree