CHAPTER 45 Dental Diseases and Disorders
Introduction
Dental diseases are the most prevalent chronic diseases worldwide.1 Despite great improvements in the oral health of populations across the world, problems still persist, particularly among poor and disadvantaged groups in both developed and developing countries. Immigrants and refugees have particularly high rates of dental diseases and unmet dental needs and these groups should be regarded as ‘at risk’ with regard to oral health. The country of origin, time span of migration and years in transition reflect the accumulated treatment needs. Even people with good oral health under normal situations can experience dramatic decline when under stressful conditions.2 The high prevalence of dental disease and neglected oral hygiene can also be the result of low priority of oral health compared to the more immediate problems of resettlement.
Although rarely life threatening, dental diseases have a detrimental effect on the quality of life from childhood through old age. Dental diseases affect eating, speaking, nutrition, health, and self-esteem.3 The interrelationship between oral and general health is well established. Severe periodontal disease is associated with diabetes mellitus, cardiovascular disease, stroke, chronic respiratory disease, and preterm low birth weight babies.4 Dental diseases can also create excessive financial and social costs on the individual and society. The treatment of dental diseases is extremely expensive, the fourth most costly disease to treat in most industrialized nations.1 Dental diseases can also affect economic productivity and compromise a person’s ability to work at home, at school, or on the job.5
Oral Health Assessment
A complete assessment of the craniofacial tissues should include observation and palpation for signs of pathology or infection. Assessment should include the head and neck, the dentition and soft tissues of the oral cavity – the mucosa covering the hard and soft palate, lips, tongue, oropharynx, floor of the mouth, and gingiva. Many systemic diseases have oral manifestations that may be the initial signs of clinical disease. A thorough oral examination can detect signs of microbial infections, pathology, oral cancer, manifestations of HIV/AIDS, injury and trauma or torture, as well as nutritional deficiencies.6 For example, there is evidence that patients who experience signs and symptoms of more advanced oral cancer are more likely to seek initial contact with medical healthcare professionals while patients with asymptomatic early-stage disease are more likely to be detected by oral healthcare providers.7 The National Institute for Dental Craniofacial Research has a step-by-step guide for health professionals to perform an oral examination, that is available on their website.8
Dental Caries
One of the most common diseases of the oral cavity is dental caries, an infectious disease induced by diet, leading to the destruction of tooth structure. An estimated five billion people worldwide suffer from dental caries.1 In the United States, dental caries remains the most common chronic disease of children aged 5–17 years (five times more common than asthma)5 and can progress throughout life. It is no longer accepted that certain races are naturally resistant to dental caries. Differences in the prevalence among different populations can be attributed to behavior, diet, and access to dental care.9
The main factors in the etiology of dental caries are cariogenic bacteria, fermentable carbohydrates, a susceptible tooth, and time. A large, carious lesion may progress to the pulp and surrounding bone, resulting in a dental abscess with possible pain and fever. If the pulp of the tooth becomes necrotic, the pain may subside, but the infection is still present (Fig. 45.1). Complications can be the spread of infection causing facial cellulitis, osteomyelitis or, in severe cases, cerebral abscess, endocarditis, or other disorders. In both primary and permanent teeth, an abscess may appear as a fistula on the gingiva and there may be a discharge when the gingiva is pressed. Treatment would be the elimination of infection and restoration of the tooth to function. Immediate referral to a dentist is recommended. Antibiotics may be indicated along with saltwater rinsing to reduce the infection. Over-the-counter pain relievers may be recommended for pain and fever. Aspirin should not be applied directly over the tooth or mucosa as it will increase the irritation and can create mouth ulcers.
Refined sugars are the most important dietary factor in the development of dental caries.3 The relationship between dental caries and refined sugar consumption has been well documented. An increased prevalence of dental caries has been associated with countries with higher per capita sugar consumption.10 In some developing countries, as socioeconomic levels rise, so does the amount of sugar in the diet, with corresponding increases in dental caries. In Africa, dental caries is considered a good proxy measure for socioeconomic development.11 Differences have been noted in caries prevalence between high and low socioeconomic groups. The prevalence and severity of dental caries is generally higher among the privileged residing in urban centers, where sugar is considered a luxury. In contrast, the indigenous rural diet is low in refined sugar and lower levels of caries have been found.11
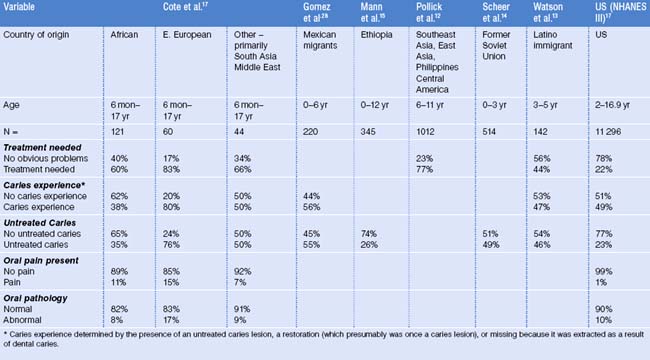
Oral health surveys in a number of countries have found that immigrant children have higher rates of treatment needs, untreated caries, oral pain, and oral pathology than US children.12–17 Table 45.1 summarizes oral health data collected from different populations of immigrant children and data collected from NHANES III of US children. Difference in the distribution of age makes it difficult to compare the data between the groups. Eastern European refugee children presented with particularly high treatment needs, untreated caries, pain, and pathology. African refugees, who originated from more rural areas, had the lowest caries experience and untreated caries. Significant differences were found when comparing the oral health status of refugee children to US children.17 The African refugee children had only half the dental caries experience of US children. However, when black African refugee children were compared to black US children, they had less of a history of dental caries but similar likelihood of having untreated dental caries, despite the fact that very few African refugee children had previous access to professional dental care.17
There are limited published data comparing the oral health status of immigrant adult populations. Adult refugees who had recently arrived in the United States primarily from Africa, the former Soviet Union, and Eastern Europe had an overall prevalence of unmet treatment needs of 87%. Forty-five percent had never been to the dentist and 13% required urgent care within 24 hours. Refugees from Eastern Europe and the former Soviet Union were over eight times more likely to present with a history of dental caries and more than 10 times as likely to have seen a dentist as those from Africa. However, the degree of urgency was greater among the Africans, with 22% who presented to the clinic in pain compared to 11% from Eastern Europe and the former Soviet Union.18 In a study conducted in New York City, Haitian adult immigrants were found to have low levels of dental caries.19
A dental assessment of asylum seekers and refugees receiving care at the Boston Center for Refugee Health and Human Rights documented that 73% of clients had untreated dental caries, with highest rates among Africans.20 The high rate can be attributed to living conditions prior to coming to the US, their extended time in transition, legal status in the US which makes them fearful to seek care and risk being deported, or lack of access to affordable dental care.
Differing levels of fluoride in the drinking water may also contribute to differences in caries experience between different refugee and immigrant populations. It has been well documented that fluoride at an optimal range of 0.7–1.2 parts per million (ppm) reduces dental caries; however, it does not eliminate risk of the disease.21 Several countries in Africa and the Eastern Mediterranean have excessively high levels of naturally occurring fluoride in the water supply.10 Excess fluoride exposure occurring during tooth formation may result in dental fluorosis.22 While clinically mild cases may appear as white spots and severe cases as discolored teeth or pitted enamel, dental fluorosis should not be misdiagnosed as dental caries.
In some parts of Africa, such as Tanzania, there is a high prevalence of dental fluorosis. One of the contributing factors is the use of fluoride-containing trona (magadi). Magadi is a crude mixture of various salts containing varying amounts of fluoride that is used to reduce cooking time. It is also added to food to add flavor, especially to vegetables and beans. A mixture of beans and bananas cooked with magadi is a traditional food used for weaning babies.22 There are no reports of this practice continuing in the US.
Early childhood caries
Early childhood caries (ECC) is a serious form of dental caries that affects the primary dentition of infants and toddlers. Decay of primary teeth can delay children’s growth, lead to malocclusion by adversely affecting the correct guidance of the permanent dentition, and cause poor speech articulation and low self-esteem.16 In many cultures, however, the primary dentition is believed to have no value and parents are not concerned if the child has decay as these teeth will be replaced. For some, the early loss of primary teeth symbolizes a life transition or a brotherhood or sisterhood with other children in that community.23
Although ECC affects children from all socioeconomic classes, it is most often found in children of new immigrants, or any US-born individual with lower socioeconomic status.24 An ongoing study in Boston has shown an overall prevalence of ECC of 8.7% compared to the national average of 4.5%.25 Differences were seen when the data were stratified by the parents’ region of origin (Table 45.2).25 ECC prevalence of 9% was seen in children whose parents were originally from North America, mainly the United States and Canada. The rate was much lower, at 6%, in children whose parents’ region of origin was the Caribbean, primarily from Haiti. The rate was higher, at 11%, in children whose parents’ region of origin was Africa, primarily from Nigeria and Cape Verde, and 12% in children whose parents’ regions of origin were other countries such as Honduras, Mexico, China, and Vietnam. Latino children have been reported to have very high levels of ECC. Thirty-three percent of Head Start Latinos in California presented with ECC compared to 13% of white children.26 At the California–Mexico border, the prevalence of ECC in Latino children was extremely high at 58% (Ramos-Gomez FJ, et al., unpublished).
Table 45.2 Distribution of Boston children’s early childhood caries (ECC) by parents’ region of origin25
| Parents’ region of origin | n | ECC |
|---|---|---|
| Asia | 51 | 13.7% |
| Middle East | 9 | 0.0% |
| Europe | 17 | 17.6% |
| Africa | 142 | 10.6% |
| North America | 301 | 9.0% |
| Central America | 29 | 10.3% |
| Caribbean | 238 | 5.9% |
| South America | 6 | 0.0% |
Similar to other forms of caries, risk factors for ECC are linked to dietary practices. Feeding practices of infants and also toddlers vary with culture and socioeconomic status and may also be influenced by family, specifically the mother’s female relatives. The influence of the extended family is important for some cultures where decisions on health and related issues may be made by older family members. One such situation is the recommendation in the US of discontinuing use of the baby bottle by 12 months of age. This practice is not popular among the Muslim Asians due to fear that the change might cause the infants to stop drinking milk and would not be acceptable in the community or to the older family members. A large milk intake is perceived as desirable since the provision of milk in the Indian subcontinent is associated with wealth.27 Latino babies have also been found to be bottle-fed for extended periods of time, often until age 2 or 3 years.
Children that are breast-fed at will or bottle-fed at night with milk or formula are at an increased risk of ECC. Studies have shown human milk and baby formula to be more cariogenic than cow’s milk.28 The practice of adding sugar or sugary flavorings to infant’s milk further increases the risk. The use of sugary drinks such as juice or soda in bed is also a risk factor. In some cultures, sugar is considered valuable as a source of energy and helpful in treating stomach aches and constipation. Sweetened drinks in bed have been found to be common practice among Latino and Asian populations and are probably a contributing factor to the high prevalence of ECC and untreated dental caries.26
Periodontal Disease
During the past 10 years, there has been an increased focus on the link between periodontal disease and systemic health. Research has shown that people with periodontitis are more likely to develop cardiovascular disease. One such study suggests the risk of fatal heart disease doubles for people with severe periodontal disease. Severe periodontal disease in pregnant women may be linked to a sevenfold increase in the risk of delivering preterm low birthweight babies.6 Diabetics are two to three times more likely to have periodontal disease which progresses rapidly and can worsen glycemic control.6
Most adults show some signs of gingivitis or periodontal disease. In the United States, there are disparities in the prevalence of periodontal disease, with rates highest among African-Americans (33%) compared to Mexican-Americans (25%) and Caucasians (20%).5 Immigrants are particularly at risk due to their interrupted lifestyles, lack of resources, and lack of access to professional dental care. Among newly arrived adult refugees in Boston, 88% had some degree of gingival inflammation, ranging from mild to severe. Nine percent presented with an acute periodontal infection requiring immediate referral to a dentist for treatment 18
In Africa, gingivitis is widespread and can be severe in children. Acute necrotizing ulcerative gingivitis (ANUG), which is now rarely seen in developed countries, is prevalent among children aged 3 years to puberty in sub-Saharan African countries.10 ANUG is a progressive, painful gingival infection with ulceration, swelling, and sloughing off of dead tissue that can spread throughout the mouth and throat. Stress, poor oral hygiene, and poor nutrition can induce the onset of ANUG. Symptoms are painful gingiva, bleeding in response to any pressure or irritation, a swollen, grayish film on the gingiva, crater-like ulcers, foul taste in the mouth, and bad breath. Medical professionals should screen refugee children, particularly from African countries, for ANUG and refer children presenting with these symptoms to a dentist. Treatment usually requires antibiotics, debridement, and, in severe cases, dental surgery (Fig. 45.2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree