Learning objectives
- •
The basic principles of bone densitometry.
- •
The densitometric diagnostic criteria of osteoporosis and osteopenia.
- •
Osteoporosis is asymptomatic until a fracture occurs.
The case study
Reason for seeking medical help
- •
DI, 68-year-old, is asymptomatic and enjoys good health. Given her age, she is referred for a DXA scan to screen her for osteoporosis.
Past medical and surgical history
- •
No relevant past medical history, no history of fractures, falls, or renal calculi.
- •
Natural menopause at age 47 years, no hormonal replacement therapy.
- •
Menarche at age 12 years, regular menstrual periods.
- •
Four children aged 39, 37, 32, and 30 years, all in good health.
Lifestyle
- •
Sedentary lifestyle.
- •
Plays golf at least three times a week.
- •
Good dietary daily calcium intake: about 1200 mg daily.
- •
No cigarette smoking, no alcohol intake, no excessive caffeine, no excessive sodium intake.
- •
Good appetite, well-balanced diet.
Medications
- •
Multivitamin tablet daily.
Family history
- •
Negative for osteoporosis.
Clinical examination
- •
Weight: 133 pounds, height: 64″, no height loss.
- •
No significant clinical findings.
Laboratory result(s)
- •
She recently had the following laboratory tests done as part of her annual clinical examination: comprehensive metabolic panel (CMP), complete blood count (CBC), serum vitamin D, and thyroid stimulating hormone (TSH): all within normal limits.
DXA and radiological result(s)
T-scores: lumbar vertebrae (L1-L4): −2.6, right femoral neck −2.2, right total hip −1.9.
Multiple choice questions
- 1.
The diagnosis of osteoporosis can be established by:
- A.
The presence of a fragility fracture.
- B.
Bone densitometry: dual X-ray absorptiometry.
- C.
Laboratory tests.
- D.
A or B.
- E.
A, B, or C.
Correct answer: D
Comment:
Osteoporosis is a silent disease until a fracture is sustained. Patients have no warning symptoms and are usually unaware of having osteoporosis until a fragility fracture occurs. This is often the first manifestation of osteoporosis and is diagnostic of osteoporosis.
A fragility fracture is defined as a fracture occurring after a fall from the standing position or from a height not exceeding body height. Fragility fractures also can be the result of trauma that ordinarily would not be expected to lead to a fracture and are referred to as low trauma, low impact, or low energy fractures. They also can occur spontaneously in the absence of any trauma and are known as atraumatic fractures. In the absence of underlying localized bone pathologies such as neoplastic deposits that may lead to fractures, fragility fractures are diagnostic of osteoporosis regardless of the bone densitometry results.
The diagnosis of osteoporosis also can be established by bone densitometry. During this procedure the bone scanned is exposed to two different X-ray wavelengths, hence the name Dual X-ray Absorptiometry (DXA) or Dual Energy X-ray Absorptiometry (DEXA). The International Society for Clinical Densitometry (ISCD) recommends that the term “DXA” be used. The two waves of X-rays are attenuated to different extents by soft and bone tissue, thus allowing the differentiation of soft from bone tissue and the calculation of the bone mineral content (BMC) and surface area of the bone scanned. The BMC is then divided by the bone surface area to calculate the bone mineral density (BMD).
The patient’s BMD is then compared to the mean BMD of an adult healthy reference population. The number of standard deviations the patient’s BMD is compared to that of the reference population is expressed as the T-score which is then used to classify subjects according to the World Health Organization guidelines ( Fig. 1 ) into three categories: osteoporosis (T-score −2.5 or lower), osteopenia (T-score less than −1.0, but higher than −2.5), or normal BMD (T-score −1.0 or higher). The patient’s BMD may also be compared to that of an age-matched population and the results expressed as Z -scores ( Fig. 2 ).
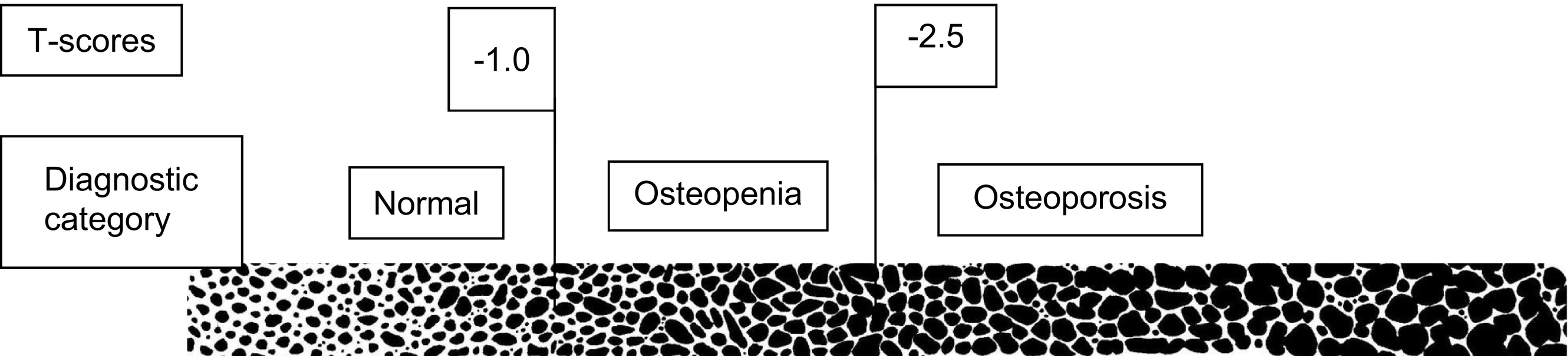
Fig. 1
T-scores and diagnostic classification (MCQ #1).
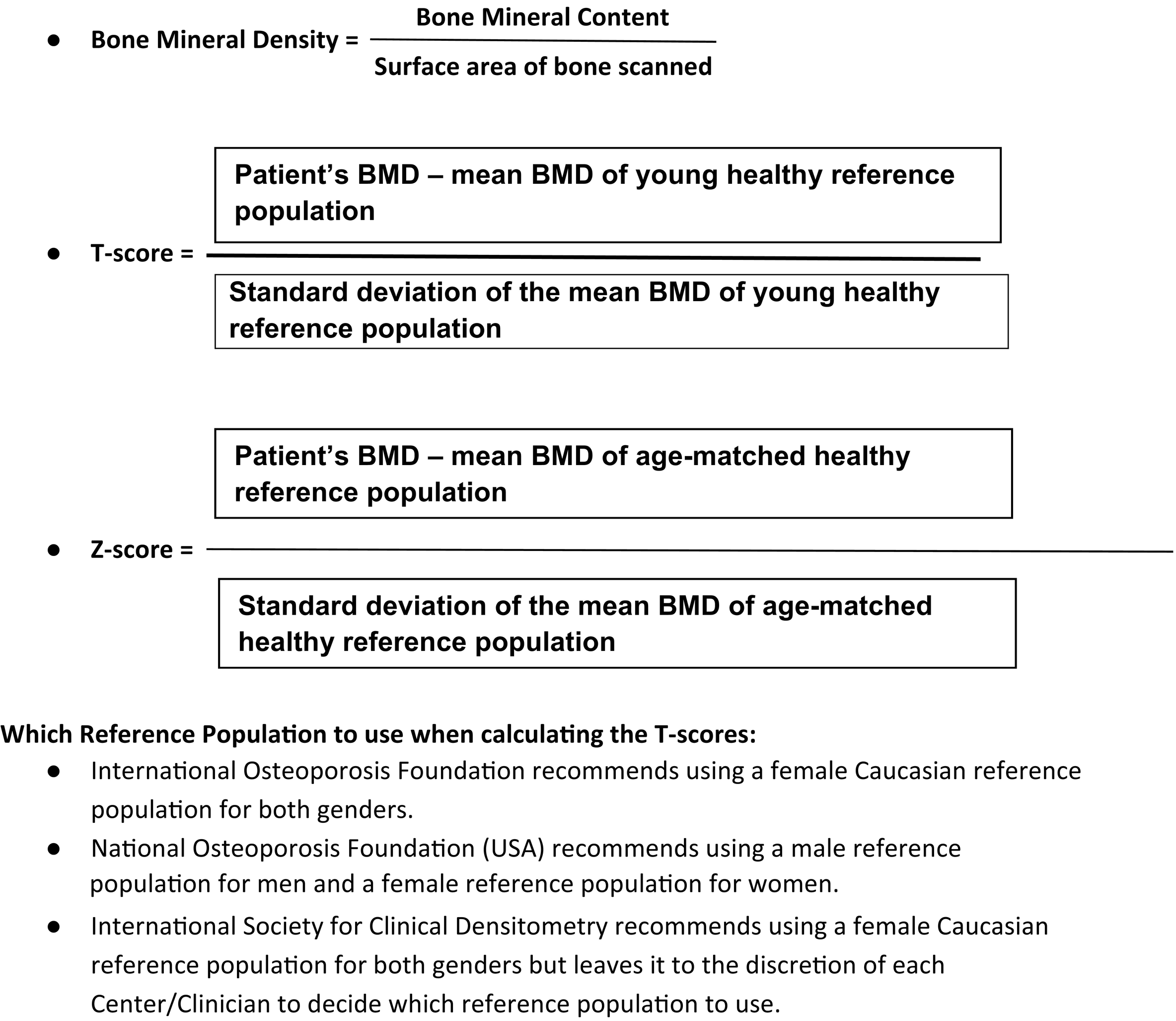
Fig. 2
Calculating BMD, T- and Z -scores.
The densitometric diagnosis is based on the lowest T-score of the femoral neck, total hip, upper 4 lumbar vertebrae (antero-posterior projection only, not lateral), or distal one-third radius of the nondominant arm. Although several sites are considered when the hip is scanned, only the BMD and T-scores of the femoral neck and total hip are considered. Similarly, although the BMD and T-scores of various sites of the distal radius are routinely calculated and listed on the computer-generated report, only the one-third (or 33%) distal radius site of the nondominant arm should be considered for diagnostic purposes ( Fig. 3 ).
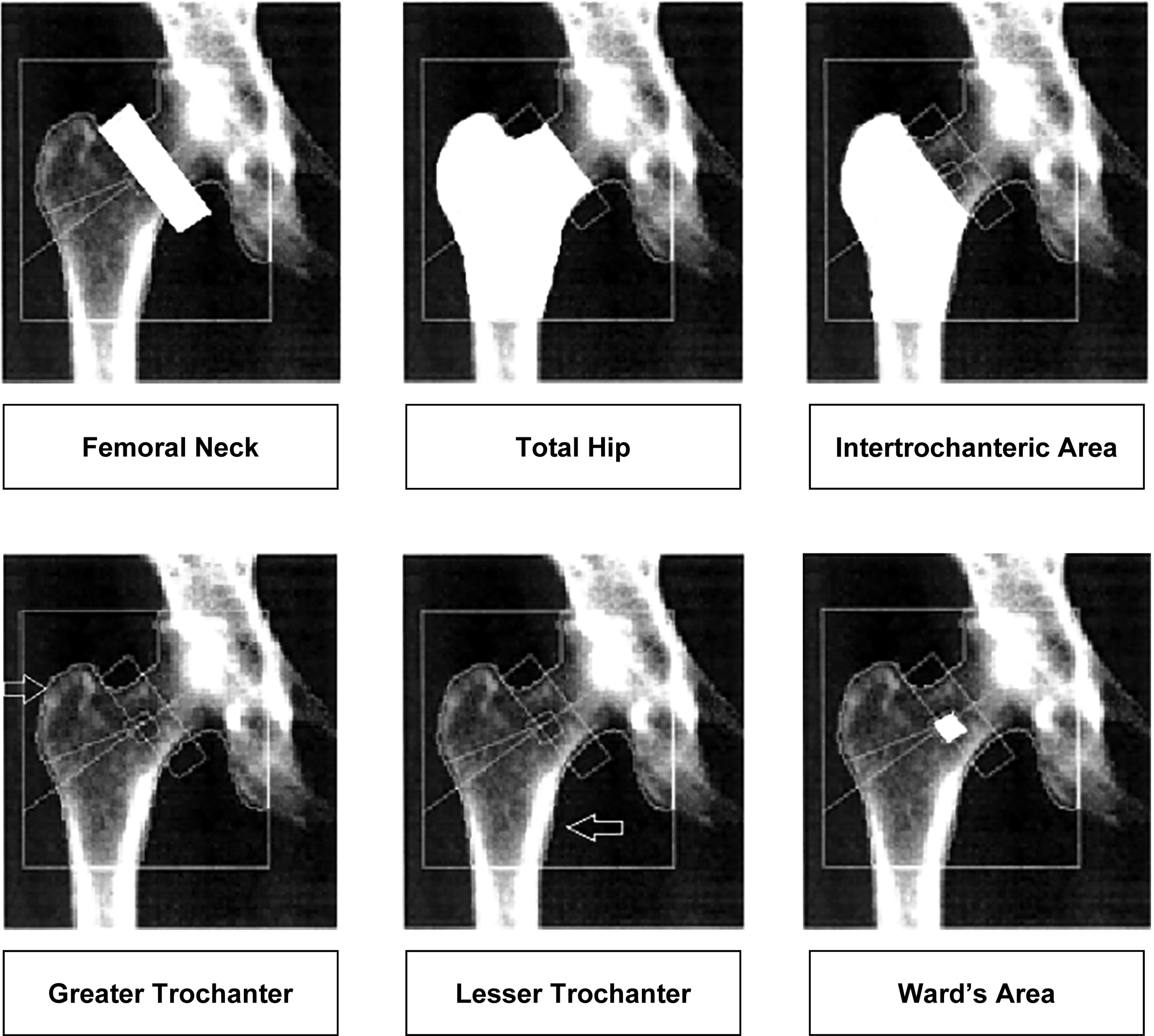
Fig. 3
Anatomical Sites Scanned—Proximal Femur.
The minimum recommended is to scan one hip and the lumbar vertebrae. There is no consensus as to which hip should be scanned: this is often determined by the physical location of the densitometry table in the scanning room. Many centers, however, routinely scan both hips and the lumbar vertebrae and modern densitometers offer the possibility of scanning both hips simultaneously without having to reposition the patient. There is also evidence to show that when both hips are scanned more patients with osteoporosis will be identified ( Fig. 4 ).
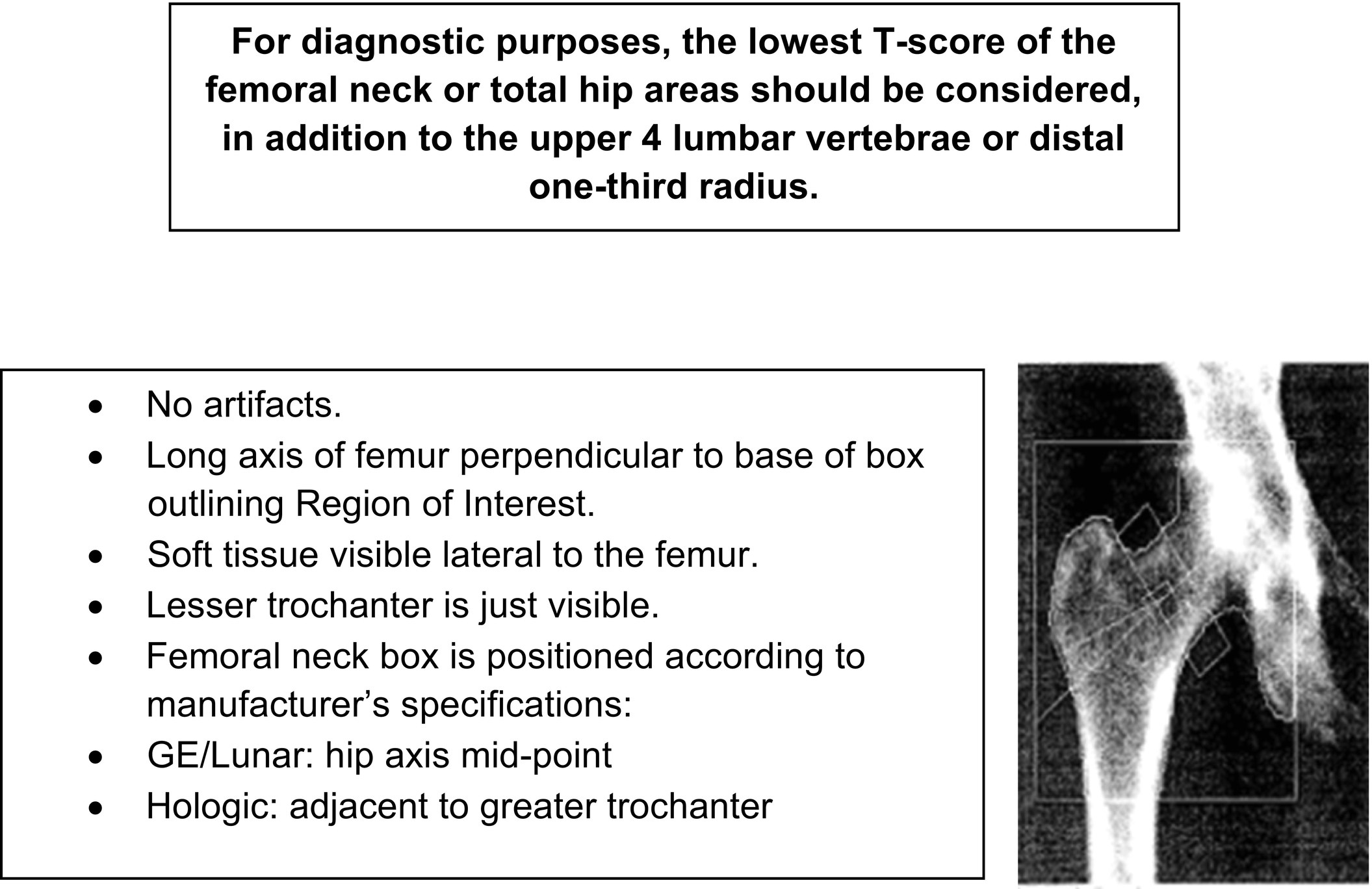
Fig. 4
Characteristics of a well-positioned DXA scan of the proximal femur.
Another advantage of scanning both hips is that it allows monitoring the patient’s BMD even after a hip fracture is sustained or the patient undergoes hip replacement surgery. In some centers the Vertebral Fracture Assessment (VFA) is also routinely done. VFA is further discussed in another case.
As long bones are not perfect cylinders and as the BMD is an aerial, not volumetric density calculated by dividing bone mineral content by bone surface area, any change in the bone surface area may affect the results. It is therefore important to ensure that patients having a DXA scan done be positioned exactly according to universal guidelines to ensure meaningful comparison to the reference population and calculation of the T-scores ( Fig. 5 ).
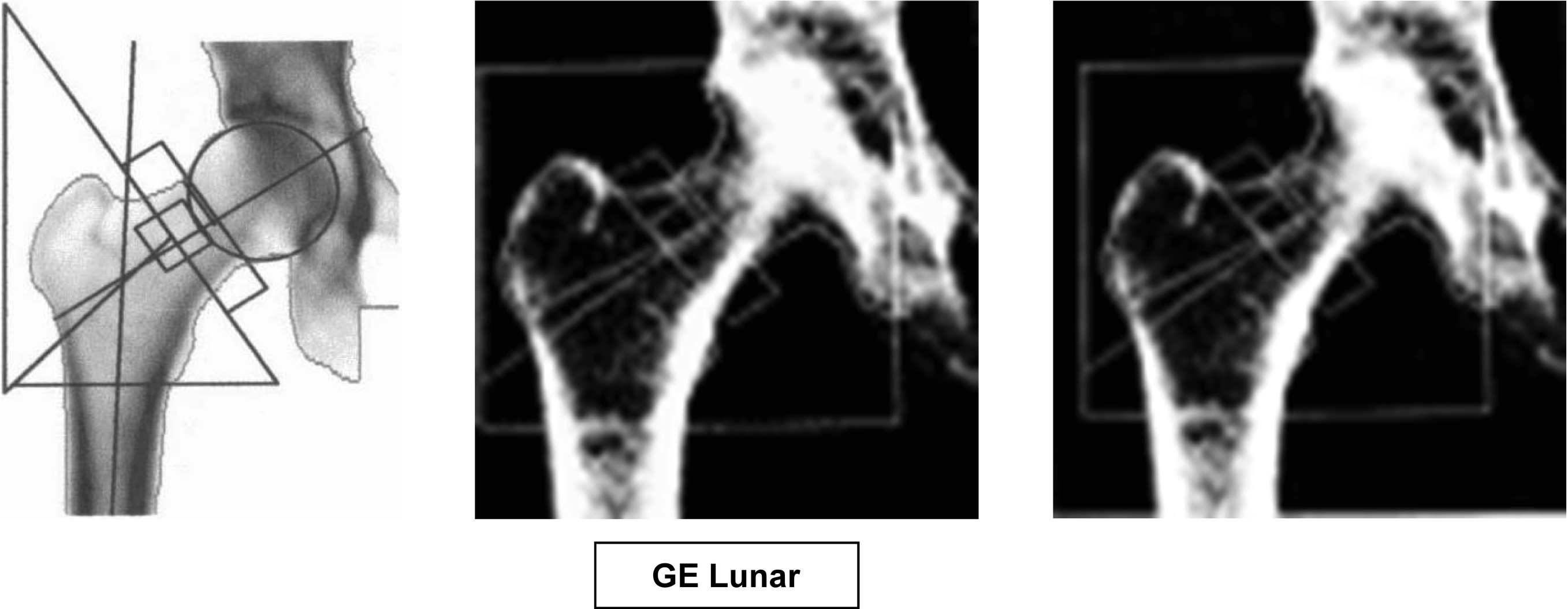
Fig. 5
Placement of femoral neck box: GE Lunar densitometers place it on the midpoint of the hip axis. Hologic densitometers anchor it to the greater trochanter.
Therefore, before accepting the scan results, it is important for the clinicians to review the pictorial scans to ensure the patient has been properly positioned, the regions of interest correctly identified, and the absence of artifacts. The anatomical sites scanned, criteria of well-positioned patients, and some common errors in positioning and analyzing the scans are shown in the accompanying figures.
Given the poor prognosis after a fragility fracture is sustained and given the availability of relatively safe medications that can significantly reduce the risk of fractures, including hip fractures, the challenge is to identify patients at risk of sustaining fractures before these fractures occur. This is particularly relevant as the morbidity and mortality associated with osteoporotic hip fractures are significant: one-year mortality is increased by 8% to 36%, with the rate being higher in men than in women, about 20% of the survivors require long-term institutional care and only about 40% are able to resume their prefracture level of independence. After a fracture is sustained the risk of subsequent fractures is increased by about 2.5-fold, thus triggering a vicious cycle. The health-related quality of life in men with osteoporosis is significantly impaired after sustaining an osteoporotic fracture.
BMD is an important factor, probably the single most important factor, determining fracture risk, but it is not the only one and many other factors modulate the BMD/fracture relationship. Indeed, many patients with a densitometric diagnosis of osteoporosis do not sustain fractures and many patients with osteopenia or even normal BMD sustain fractures, including fragility fractures. It has therefore been suggested that the diagnosis of osteoporosis in addition could be made on clinical grounds based on an elevated fracture risk. Notwithstanding, assessing fracture risk should be an integral part of the diagnostic process of osteoporosis as it may be used to develop a management strategy tailored to the circumstances of individual patients and convince patients and attendants of the gravity of fractures. This is further discussed in other cases in this series.
There are no laboratory tests to diagnose osteoporosis. They are used to identify secondary causes of osteoporosis. Markers of bone turnover are sometimes used for diagnostic purposes and to monitor the patient’s response to treatment. Laboratory tests are discussed in another case in this series.
- A.
- 2.
The T-score, not BMD, is used to diagnose osteoporosis because of different densitometers:
- A.
Use different technologies to produce the 2 waves of X-rays.
- B.
Use different algorithms to differentiate soft from bone tissue.
- C.
Use different anatomical sites.
- D.
A and B.
- E.
A, B, and C.
Correct answer: E
Comment:
The absolute BMD is different when measured by different densitometers because of all the previously listed reasons. Whereas Hologic densitometers consider the area immediately adjacent to the greater trochanter as being the femoral neck, GE Lunar densitometers consider the femoral neck area at the midpoint of the hip axis. The femoral neck BMD, therefore, is often different when the patient is scanned with GE Lunar or Hologic densitometer ( Fig. 6 ). Therefore the “T-score” rather than the absolute BMD is used to assess the patient’s bone status.
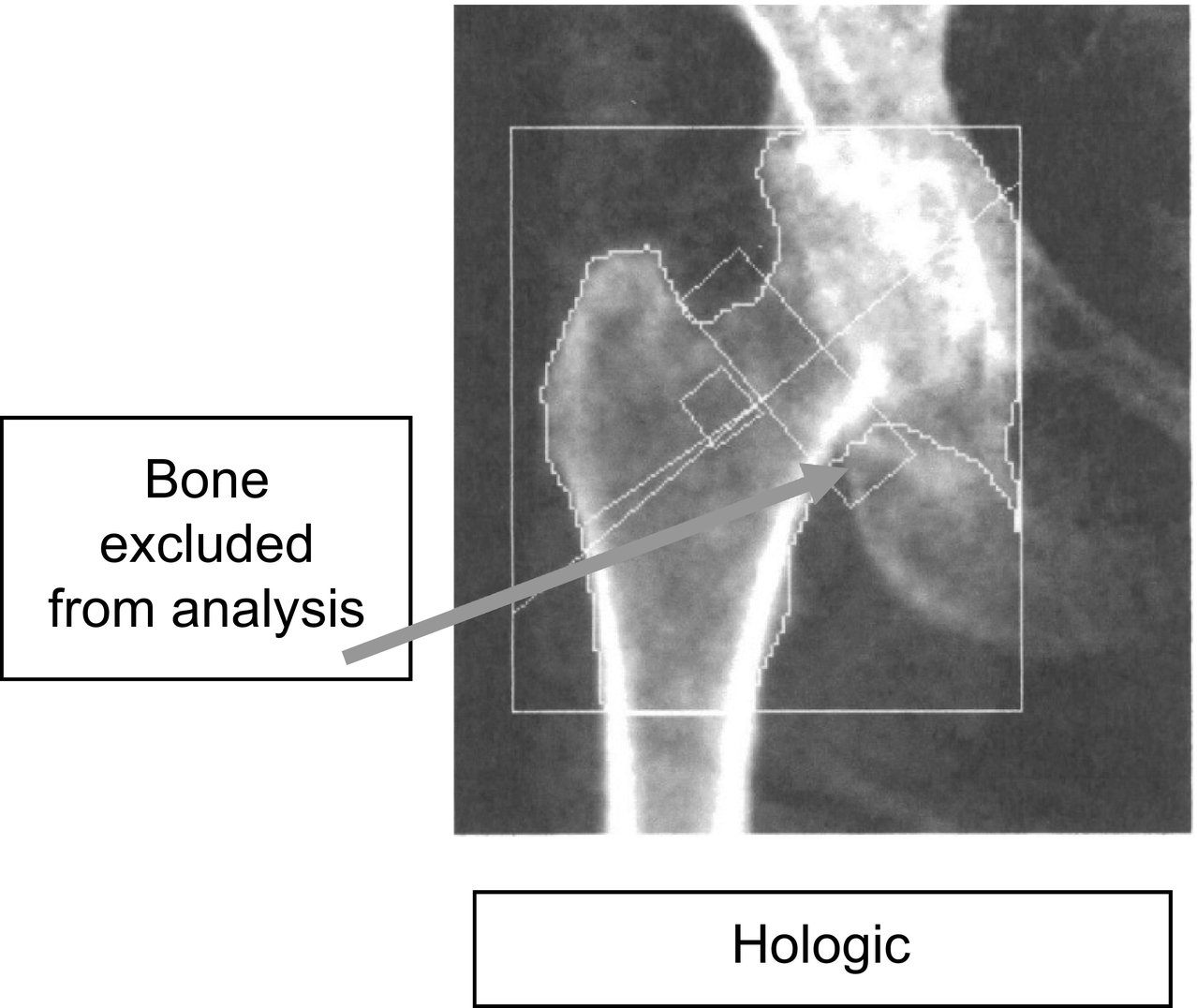
Fig. 6
Software is available to ensure femoral neck box only contains femoral neck and no part of neighboring bones.
Although it may appear more rational to compare the patient’s BMD to that of an age-matched population, the patient’s BMD is compared to a reference population in whom the risk of fracture is low, i.e., an adult healthy population, hence the use of the T-score.
In the USA, the National Osteoporosis Foundation recommends that the young healthy reference population used to derive the T-scores be gender specific, i.e., in men T-scores be calculated based on a male reference population and in women the T-scores be derived from a female reference population. On the other hand, the International Osteoporosis Foundation (IOF) recommends using a female Caucasian population for both genders and all races. The International Society for Clinical Densitometry (ISCD) also recommends using a female Caucasian reference population but leaves it to the discretion of individual centers to determine which reference population to use for men.
T-scores are also used in several permutations to estimate fracture risk. This is further discussed in another case in this series. T-scores should not be used to monitor the patient’s progress; this is best done by monitoring changes in BMD.
Z -scores represent the number of standard deviations the patient’s BMD is compared to an age and gender-matched healthy reference population. Depending on the manufacturers of the bone densitometer, the reference population also may be matched to the subject’s ethnic group. Z -scores are used in children, adolescents, premenopausal women, and men under the age of 50 years who are then classified as having a “low bone mass for given age” if the Z -score is 2 or more standard deviations below that of the reference population or “normal bone mass for given age” if the Z -score is less than 2 or more standard deviations below the mean of the reference population. In the absence of fragility fracture(s), the term “osteoporosis” is not recommended in these populations.
Some clinicians use Z-scores in postmenopausal women and men over the age of 50 years to determine the extent of workup to identify secondary causes of osteoporosis. A level of −2.0 is sometimes used as a rough guide, but this figure has not been satisfactorily substantiated ( Figs. 7–13 ).
- A.