Introduction
Water accounts for about 60% of body weight in an average human, varying mainly with degree of adiposity. As the percentage of body fat increases, the amount of body water decreases. Water is distributed in virtual compartments in the body, moving between compartments by osmosis or by pumps. Total body water (TBW) is about 42 l in a 70 kg person, or 600 ml kg−1. TBW is divided into intracellular fluids (two-thirds TBW, 400 ml kg−1) and extracellular fluids (one-third TBW, 200 ml kg−1). About 75% of the extracellular fluid is distributed interstitially between cells (150 ml kg−1) and about 25% of extracellular fluid is found in the intravascular space (50 ml kg−1).1
The spaces define the clinical syndromes of fluid loss. The principal regulator of extracellular water is sodium, because of active transport of sodium into this space. The principal regulator of the larger intracellular compartment is the effective osmolarity of the extracellular fluid. By osmosis, essentially equal tonicity is maintained across both compartments. Intravascular volume depletion leads to hypotension, compensatory tachycardia, decreased tissue perfusion and shock. The intravascular volume is highly protected to prevent these complications, primarily regulated by a sodium pump. Water is transferred to the intravascular volume from the extracellular compartment and the intracellular compartment.
Loss from the extracellular compartment is termed intravascular volume depletion and loss from the intracellular compartment is termed dehydration. Loss from both compartments is termed hypovolaemia.
Water Loss
Water can be lost from the body via renal, cutaneous, respiratory and gastrointestinal routes. The kidney is the main controller of body water. The kidneys filter about 150 l of fluid per day, but only about 1% (1.5 l) is excreted as urine. Cutaneous water loss, through sweating, is a major thermoregulatory mechanism. Large amounts of heat are dissipated by sweat. The volume of water loss is usually around 500 ml per day, but can increase substantially in the presence of fever, high environmental temperatures, increased physical activity, increased metabolism or burns. A relatively small amount of water (around 200 ml per day) can be lost through respiration. This loss is affected by ventilatory volume and the environmental relative humidity. A large amount of water passes through the intestines each day and is recovered by the colon. Because of this, a relatively small amount of water (about 100 ml per day) is lost through faeces. However, gastrointestinal loss can increase significantly in the presence of diarrhoea, vomiting or other gastrointestinal pathology and cause severe dehydration.
Regulation of Water Balance
The balance between water loss and water repletion is regulated by arginine vasopressin (AVP). AVP works as an antidiuretic hormone, thereby regulating water excretion, and also by stimulating thirst, which regulates water ingestion. This balance is so carefully maintained that the osmolarity varies only between 282 and 298 milliosmoles (mOsm) per kilogram. Disorders of this careful balance can lead to severe illness and death.
AVP, the main water-regulating hormone, is controlled by osmotic sensors in the hypothalamus, and to a lesser extent by baroreceptor (pressure) signals. AVP levels increase rapidly with small increases in osmolality and produce sensations of thirst. The osmotic level for stimulation of AVP appears to be 284 mOsm kg−1, with sensations of thirst appearing at a threshold of 294 mOsm kg−1.2 However, the data suggest that other non-osmotic triggers for thirst occur when the osmolarity is in the normal range. Moreover, there appears to be an individual set point that varies from person to person.3
Increased water loss due to exposure to heat, fever, insufficient fluid consumption and physical activity results in an increase in osmolality and a decrease in plasma volume (hyperosmotic hypovolaemia), the main cause of dehydration. In such situations, dehydration stimulates both thirst and increases in AVP levels. This results in thirst, which increases fluid ingestion (when access is available), and a decrease in urinary output due to increased tubular water reabsorption in the nephron. Because of urine concentration, the urine becomes a darker yellowish colour. Changes in urine colour, urine osmolality and urine specific gravity have been used estimate levels of hydration.
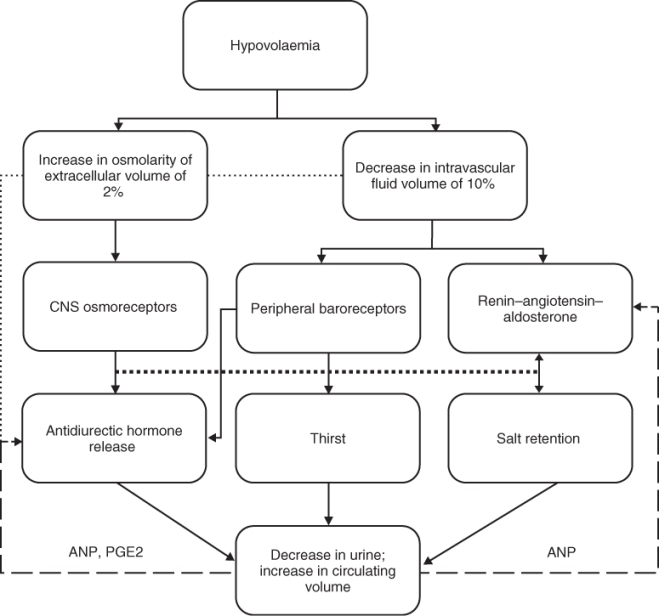
The act of drinking rapidly suppresses the release of AVP, through a reflex mechanism in the oropharynx. Water balance is also affected by changes in intravascular volume. A loss of about 10% of circulating intravascular volume also stimulates the osmoreceptors. Loss of intravascular volume directly stimulates thirst and water intake through baroreceptors located in the vascular system. The renin–angiotensin–aldosterone system is also activated by stimulation of the baroreceptors, with the effect of increasing salt intake.
Negative feedback loops operate in conjunction with these systems. Osmotic dilution shuts off the thirst stimulus and AVP secretion. Continued osmotic dilution also stimulates the renin–angiotensin–aldosterone system to retain sodium and restore osmolarity. The renin–angiotensin system controls salt intake and thereby controls intravascular volume. Other hormones include atrial natriuretic peptide, which has a negative feedback to decrease AVP secretion and the renin–angiotensin–aldosterone system. Urodilatin and the oropharyngeal swallowing reflex also appear to play a role. A simplified diagram of volume regulation is shown in Figure 18.1.
Figure 18.1 Simplified regulation of water balance. CNS = central nervous system; ANP = atrial natriuretic peptide; PGE2 = prostaglandin E2.
Water Regulation in Older Adults
In older persons, the regulation of water balance appears to be impaired. There is a diminished thirst response to in older persons to water deprivation4 or infusion of hypertonic saline.5 When older and younger men were restricted in water intake over a 24 h period that produced equal weight loss, healthy men aged 67–75 years were less thirsty and drank less water over 2 h compared with younger men.6 In studies using heat stress and exercise to induce hyperosmolarity and a volume deficit, older individuals tended to operate at a higher plasma osmolality, indicating a shift in the set point of the regulatory system.7 Again, the perception of thirst was not different in older men. Other studies have found that older men perceived a greater thirst, but drank the same amount of water as younger men in response to passive heat stress.8
In the face of water loss producing either an osmoreceptor or a baroreceptor stimulus, older persons exhibit a decreased thirst sensation and reduced fluid intake. Fluid replacement is effective but slower in older persons. Chronic fluid maintenance in response to repetitive dehydration also appears to be reduced, contributing to a decrease in the ability to expand plasma volume. The age differences in the physiological control systems associated with dehydration are more closely associated with a decrease in thirst perception. The data suggest that there is a higher osmotic operating point for thirst sensation under normal daily conditions and a diminished sensitivity to thirst triggered by the vascular baroreceptors.9
Dehydration, Intravascular Fluid Loss and Hypovolaemia
Physiologically, the term dehydration refers specifically to a decrease in intracellular water. A loss in the intravascular compartment results in intravascular volume depletion. Loss of both intracellular water and intravascular water is more appropriately termed hypovolaemia. Dehydration is always hypernatraemic, whereas intravascular volume depletion can be either hypernatraemic, hyponatraemic or isotonic.
Hypertonic intravascular volume depletion results when water losses are greater than sodium losses. Fever results in loss of water through the lungs and skin and, when combined with limited ability to increase oral fluid intake, is perhaps the most common cause of hypernatraemic intravascular volume depletion. As water is transferred from the intracellular compartment to maintain intravascular volume, total body water decreases, causing dehydration. Characteristic laboratory parameters include hypernatraemia (serum sodium levels >145 mmol l−1) and hyperosmolality (serum osmolality >300 mmol kg−1).
Isotonic intravascular volume depletion results from a balanced loss of water and sodium, which can occur during a complete fast. Vomiting and diarrhoea, because of large amounts of both water and electrolytes in gastric contents, will result in isotonic dehydration.
Hypotonic intravascular volume depletion occurs when sodium loss exceeds water loss. This type of dehydration occurs primarily with overuse of diuretics causing excess loss of sodium. The serum sodium is decreased (<135 mmol l−1) and the serum osmolality is low (<280 mmol kg−1).
Diagnosis of Dehydration
There is no accepted definition of dehydration. A number of parameters have been used to suspect or define dehydration, but all have limitations.10
Body Composition
The components of body water can be accurately measured by research techniques such as radiological dilution. Bioelectrical impedance11–13 can determine total body water and extracellular water, estimating the intracellular water by subtraction. Bioelectrical impedance is based on the fact that fat-free mass has a much greater electrical conductivity than fat mass. However, the standard error of the fluid compartment estimates may be as high as ±2 l. Moreover, these modalities may not be readily available in clinical settings.
Body Weight
A useful definition of dehydration is a loss of ≥3% of body weight. However, this presumes knowing the stable body weight prior to dehydration. This is useful in athletes and younger persons, but is not practical in older individuals. Weight fluctuations due to disease or drugs may be misleading, and at the lower body weights in older persons may be a total of 3–4 lb (∼1.3–1.8 kg), which is in the standard error of measurement of most scales.
Physical Examination
The physical signs of dehydration are often confusing, particularly in older adults. Clinical signs of extravascular volume deficit are often misleading. The most helpful physical findings are either severe postural dizziness such that the patient cannot assume an upright position or a postural pulse increment of 30 beats min−1 or more. The presence of either finding has a poor sensitivity for moderate intravascular volume depletion due to blood loss (22%) but a much greater sensitivity for large blood loss (97%). Supine hypotension and tachycardia are frequently absent in extravascular fluid loss, and the finding of mild postural dizziness has no proven value. The presence of a dry axilla supports the diagnosis of dehydration [positive likelihood ratio, 2.8; 95% confidence interval (CI), 1.4–5.4], and a moist mucous membrane and a tongue without furrows argue against the presence of dehydration (negative likelihood ratio, 0.3; 95% CI, 0.1–0.6 for both findings). In adults, the capillary refill time and poor skin turgor have no proven diagnostic value.14
Laboratory Parameters
Given the paucity of sensitive clinical signs, laboratory evaluation provides the clinical gold standard. The diagnosis of extracellular volume depletion can be suspected from history and careful physical examination, but requires support of adjunctive data from laboratory studies. The diagnosis of intracellular volume depletion cannot be established without laboratory analysis of serum sodium or calculation of serum tonicity.15
Serum osmolarity is very sensitive, rising in dehydration with as little as a 1% change in body weight.16 During dehydration due to insufficient fluid intake, both plasma sodium and osmolarity are significantly elevated. Serum osmolarity can be measured directly or estimated by the following formula:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








