9
Cystic and Spindle Cell Neoplastic Mimics of the Liver
INTRODUCTION
Cysts are increasingly diagnosed by improved methods of imaging of the liver and bile ducts. Small cysts rarely cause symptoms and their findings are invariably incidental, whereas larger cysts may displace or compress adjacent structures and can be symptomatic.
There are several types of grossly visible cysts within the liver. Some are neoplastic cysts such as mucinous cystic neoplasms, while others are congenital or developmental in origin such as simple biliary cyst, peribiliary cyst, Caroli disease, and solitary foregut cyst. Caroli disease and multiple simple biliary cysts are part of hepatic fibropolycystic disease, which encompasses choledochal cyst, polycystic liver disease, congenital hepatic fibrosis, and Caroli disease. The various manifestations of hepatic fibropolycystic disease are thought to stem from ductal plate malformation in different parts of the biliary tree. Both simple biliary cyst and peribiliary cyst may also be associated with autosomal dominant polycystic kidney disease to a variable extent (454).
Most of simple hepatic cysts are benign, which can be ensured by imaging modalities. On ultrasound, simple cysts have smooth walls and echo free contents with an increase of through transmission of the sound waves. CT scan demonstrates a low attenuation value of the content equivalent to water, nonenhancing with contrast.
Multiseptated or complex cysts, cysts with mural nodules, or thick-walled cysts are potentially malignant or may represent cystic metastasis from other organs. Cystic metastases are part of the differential diagnosis of hepatic cysts when single or multiple liver cysts are newly formed, when they enlarge in a short period of time, when there is elevation of serum tumor markers, or when there is rapid progression of symptoms. Cystic metastases are either due to central necrosis of solid metastases or to cyst-forming carcinomas of the colon, pancreas, stomach, ovary, thyroid, or kidney. Imaging techniques such as abdominal ultrasound and magnetic resonance imaging (MRI) can be used to obtain information on the presence of a vascular signal in wall nodularities or septae, on the presence of wall enhancement on MRI, and on the nature of the cystic contents. To confirm the diagnosis, repeated fine needle aspiration of the cystic wall may be necessary.
Primary spindle cell lesions of the liver represent either sarcomatoid hepatocellular carcinoma or sarcomatoid cholangiocarcinoma, or spindle cell neoplastic mimics such as inflammatory myofibroblastic tumor (IMT). The majority of malignant mesenchymal lesions are metastatic sarcomas, such as gastrointestinal stromal tumor and leiomyosarcoma. Malignant primary mesenchymal lesions of the liver are rare. Angiosarcoma is the most common type of primary mesenchymal lesion among these rare lesions. A handful of reported cases of primary leiomyosarcoma, fibrosarcoma, liposarcoma, osteosarcoma, and malignant peripheral nerve sheath tumor of the liver can be found in the literature.
SIMPLE BILIARY CYST
A simple biliary cyst is a unilocular cyst lined by a single layer of biliary epithelium. The underlying stroma is composed of dense fibrous tissue and is often collagenized. Synonyms for simple biliary cyst include “solitary bile duct cyst,” “solitary unilocular cyst,” and “simple nonparasitic cyst.” Simple biliary cyst does not communicate with the biliary tree, and its frequent coexistence with biliary microhamartoma suggests that simple biliary cysts arise from biliary microhamartoma (von Meyenburg complex).
 CLINICAL FEATURES
CLINICAL FEATURES
Simple biliary cysts can be single or multiple and occur at all ages, but the majority of simple biliary cysts occur in patients over 40 years old and the prevalence increases with age. They are rare in children, although there were reported cases of simple biliary cyst in infants (455,456). The rare occurrence of these cysts in fetuses and newborns have raised the notion that these cysts are possibly congenital in origin (457). Another possible origin of these biliary cysts is from dilatation of peribiliary glands, perhaps related to congenital or genetic factors (458); however, this last hypothesis is more suitable for the pathogenesis of peribiliary cyst. Two cases of left-sided gallbladder, in which the gallbladder was attached to the lower surface of the left lateral segment of the liver, have been reported in association with congenital simple biliary cysts (459).
Simple biliary cysts are usually located directly subcapsular, but some may occur deeper in the liver parenchyma or in the hilar region (460). Obstructive jaundice has been reported in centrally located cyst that led to obstruction of large bile ducts (461). Ascites, hepatic venous outflow obstruction, and spontaneous rupture are rare (462,463).
When multiple cysts are present, they often represent a component of autosomal dominant adult polycystic disease. PKD-1 and PKD-2 genes with their polycystin-1 and polycystin-2 gene products in autosomal adult polycystic disease were found to be important molecules that were closely related to the primary cilia of renal tubules (454). The failure of primary cilia may be responsible for cyst formation in the livers and kidneys of these patients. Polycystic liver disease is most often associated with autosomal polycystic kidney disease although polycystic liver may be an isolated finding and is genetically linked to chromosome 19p13.2–13.1 (464). About half of the patients with polycystic liver disease have polycystic kidneys, whereas the majority of patients with polycystic kidneys have a polycystic liver.
Simple biliary cysts typically demonstrate imaging characteristics of an uncomplicated, simple, fluid-containing lesion by various imaging modalities.
 PATHOLOGIC FEATURES
PATHOLOGIC FEATURES
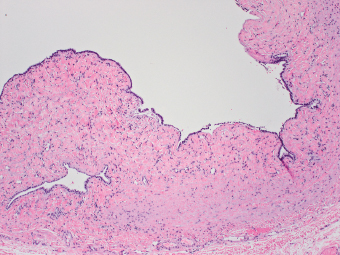
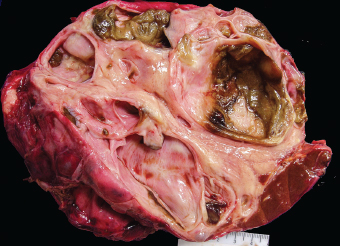
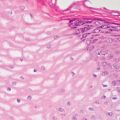
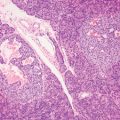
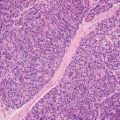
Simple biliary cysts are grossly well-demarcated, round to ovoid cysts and generally unilocular (Figure 9.1). Several types of cyst contents can be encountered: serous or mucoid fluid, blood stained if traumatized, or purulent if infected (465). The cyst is lined by a layer of columnar or low-cuboidal biliary epithelium with basally located nuclei, surrounded by dense fibrous stroma, which is often collagenized and rarely calcified (Figure 9.2). Macrophages containing hemosiderin, cholesterol, cholesterol crystals, or cellular debris from the cyst cavity may be present within the wall. Biliary microhamartomas (von Meyenburg complexes) are often found adjacent to simple biliary cysts (Figure 9.3). Repeated hemorrhage or infection may cause cyst wall thickening or mural nodule formation (466).
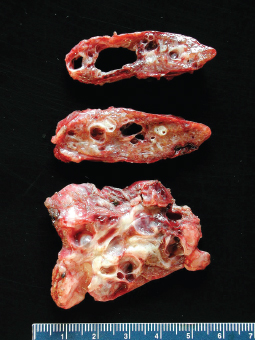
FIGURE 9.1 Simple biliary cyst involving a segment of the liver. The inner lining is smooth. The surrounding liver parenchyma is compressed and atrophic.
FIGURE 9.2 Simple biliary cysts are lined by a layer of cuboidal biliary epithelium.
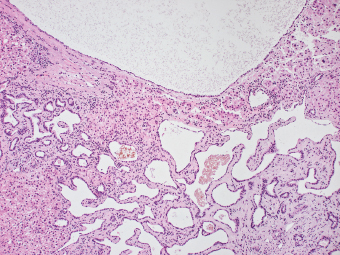
FIGURE 9.3 Biliary microhamatoma, composed of dilated and tortuous ductular structures containing bile concretion, is often present within the wall of a simple biliary cyst.
The liver may be enlarged when multiple cysts are present. They can be diffusely scattered in the liver or restricted to one lobe, usually the left. The larger cysts are probably formed by rupture of septa between adjacent cysts, and the cut surface of the liver may display a honeycomb appearance.
 DIFFERENTIAL DIAGNOSES
DIFFERENTIAL DIAGNOSES
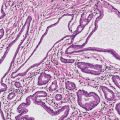
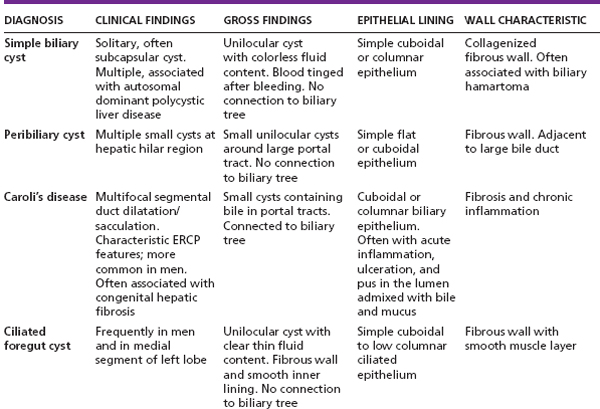
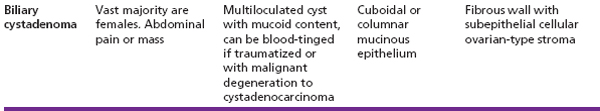
The differential diagnoses of simple biliary cysts include other benign hepatic cysts, such as peribiliary cyst, mucinous cystic neoplasm (Figures 9.4 and 9.5), and ciliated foregut cyst (see Table 9.1).
Hemorrhage followed by thickening of the wall may cause gross and microscopic resemblance of simple biliary cyst to mucinous cystic neoplasm, but the ovarian-type stroma characteristic of mucinous cystic neoplasm is not identified in simple biliary cyst.
FIGURE 9.4 Benign mucinous cystic neoplasm is typically a multiloculated cyst with brown-colored material as evidence of old hemorrhage.
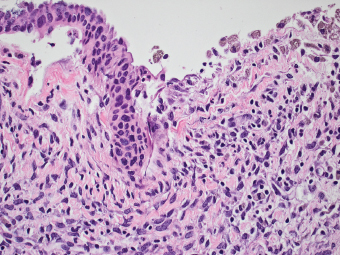
FIGURE 9.5 The inner lining of benign mucinous cystic neoplasm is cuboidal to low columnar mucinous epithelium. Macrophages containing hemosiderin are present at denuded epithelial lining. The underlying stroma is hypercellular, resembles that of ovary.
TABLE 9.1 Differential Diagnosis of Cystic Neoplastic Mimics of the Liver
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree