Adrenal glands are common sites of disease involved in a wide spectrum of pathology. Several imaging studies allow accurate diagnosis of adrenal masses, separating inconsequential benign masses from the lesions that require treatment. This article discusses contemporary adrenal imaging techniques, imaging appearance, and the optimal imaging algorithm for the workup of common adrenal masses.
Key points
- •
Adrenal masses are common and mostly benign in patients without known malignancy.
- •
Most adrenal masses can be accurately characterized by contemporary computed tomography, magnetic resonance imaging, and positron emission tomography.
- •
Computed tomography and magnetic resonance imaging are excellent tools in the detection of clinically suspected hyperfunctioning adrenal mass.
- •
Appropriate utilization of imaging is important for optimal management, to separate benign inconsequential adrenal masses from those that require treatment.
The adrenal gland is a common site of disease and can harbor a wide range of pathology. Because of expanding clinical indications for cross-sectional imaging and improved spatial resolution of computed tomography (CT), magnetic resonance imaging (MRI) and ultrasound scan, adrenal masses are now frequently discovered incidentally. The prevalence of adrenal masses at CT is approximately 5%, comparable to the estimated prevalence in the general population of 3% to 7%. Most adrenal lesions are benign, most commonly nonfunctioning adenoma. However, the adrenal gland is also a common site of metastasis in oncologic patients. The adrenal gland can also be the source of hyperfunctioning tumors that require intervention and, more rarely, primary malignant neoplasms. Contemporary adrenal imaging is highly accurate in both the detection and characterization of adrenal masses. This article discusses the role of imaging in the evaluation of more common adrenal masses, with primary emphasis on CT and MRI.
Preimaging planning
Normal Adrenal Gland
The adrenal glands are well visualized on abdominal CT and MRI. They are located anterosuperiorly to the kidneys within the perirenal space, enclosed by perirenal fascia. The normal adrenal glands are homogeneous in density or signal, and have an inverted V or Y shape ( Fig. 1 ). The arterial supply to the glands is via the superior, middle, and inferior adrenal arteries (branches of the inferior phrenic artery, aorta, and renal artery, respectively). The venous drainage of the adrenal glands is predominantly by the central vein, typically draining directly into the inferior vena cava on the right and the caudal path on the left into the left renal vein. The adrenal gland is composed of the adrenal cortex and medulla, 2 functioning units with different embryologic origin and endocrine functions. The adrenal cortex secretes cortisol, aldosterone, and androgen, and the adrenal medulla secretes epinephrine and norepinephrine.
Principles and Rationales for Imaging Studies
The selection of the optimal adrenal imaging modality depends on the reason for imaging, whether the test is for detection or characterization of an adrenal mass, as described in a later discussion. Other factors, such as contrast allergy, renal insufficiency, and radiation concern may also play a role in imaging modality selection.
Detection of an abnormality is finding the lesion, most commonly to assess for metastasis in patients with an established malignancy. In this setting of metastatic workup, contrast-enhanced CT is the most appropriate tool with positron emission tomography (PET) increasingly used in certain malignancies, such as lung cancer. Another important clinical scenario of adrenal mass detection is to localize a suspected hyperfunctioning tumor in a patient with biochemical evidence of hormonal excess. Either CT or MRI is used to localize most of the hyperfunctioning tumors, and occasionally metaiodobenzylguanidine scintigraphy may be necessary to localize a suspected pheochromocytoma.
Characterization of an abnormality is determining lesion histology using imaging. Certain adrenal masses have specific benign diagnostic features at detection, so that further workup is not warranted. However, adrenal masses often have a nonspecific appearance, especially at original contrast-enhanced CT performed for another reason. For these adrenal “incidentalomas,” defined as adrenal masses detected incidentally on an imaging examination performed for other reasons, the imaging goal is to separate a benign mass, most commonly an adenoma, from a mass that requires treatment. CT and MRI are the most commonly used imaging tools in characterizing adrenal masses, with PET usually reserved for patients with known extra-adrenal malignancy. The imaging appearances on these studies reflect physiologic differences of adenoma from malignant masses: intracytoplasmic lipid content, contrast washout pattern, and metabolic activity.
CT is highly accurate in diagnosing adenoma, because both lipid content and washout characteristics can be used, as discussed later. The main advantages of MRI over CT are in patients in whom iodinated contrast is contraindicated because of allergy or renal insufficiency or in young patients in whom radiation exposure is a concern. The premise behind PET imaging is that malignant tumors are usually glucose avid because of increased metabolic activity. Most metastatic adrenal masses show increased activity, whereas most benign adrenal lesions do not. The need for imaging-guided biopsy to diagnose an adrenal mass has decreased in recent years as advances in adrenal imaging now allow accurate characterization of most adrenal masses. The imaging modalities used to characterize adrenal masses are summarized in Table 1 .
| Imaging Procedure | Rationale for Selection | Issues |
|---|---|---|
| CT | Most widely available Diagnosis based on density or CT washout | Contrast allergy and renal insufficiency (when contrast is necessary for diagnosis) Radiation in young patients |
| MRI | Young patients and patients with renal insufficiency | MR incompatible device (eg, pacemaker) |
| PET | Mostly in patients with known cancer | Not recommended in patients without a known malignancy |
Preimaging planning
Normal Adrenal Gland
The adrenal glands are well visualized on abdominal CT and MRI. They are located anterosuperiorly to the kidneys within the perirenal space, enclosed by perirenal fascia. The normal adrenal glands are homogeneous in density or signal, and have an inverted V or Y shape ( Fig. 1 ). The arterial supply to the glands is via the superior, middle, and inferior adrenal arteries (branches of the inferior phrenic artery, aorta, and renal artery, respectively). The venous drainage of the adrenal glands is predominantly by the central vein, typically draining directly into the inferior vena cava on the right and the caudal path on the left into the left renal vein. The adrenal gland is composed of the adrenal cortex and medulla, 2 functioning units with different embryologic origin and endocrine functions. The adrenal cortex secretes cortisol, aldosterone, and androgen, and the adrenal medulla secretes epinephrine and norepinephrine.
Principles and Rationales for Imaging Studies
The selection of the optimal adrenal imaging modality depends on the reason for imaging, whether the test is for detection or characterization of an adrenal mass, as described in a later discussion. Other factors, such as contrast allergy, renal insufficiency, and radiation concern may also play a role in imaging modality selection.
Detection of an abnormality is finding the lesion, most commonly to assess for metastasis in patients with an established malignancy. In this setting of metastatic workup, contrast-enhanced CT is the most appropriate tool with positron emission tomography (PET) increasingly used in certain malignancies, such as lung cancer. Another important clinical scenario of adrenal mass detection is to localize a suspected hyperfunctioning tumor in a patient with biochemical evidence of hormonal excess. Either CT or MRI is used to localize most of the hyperfunctioning tumors, and occasionally metaiodobenzylguanidine scintigraphy may be necessary to localize a suspected pheochromocytoma.
Characterization of an abnormality is determining lesion histology using imaging. Certain adrenal masses have specific benign diagnostic features at detection, so that further workup is not warranted. However, adrenal masses often have a nonspecific appearance, especially at original contrast-enhanced CT performed for another reason. For these adrenal “incidentalomas,” defined as adrenal masses detected incidentally on an imaging examination performed for other reasons, the imaging goal is to separate a benign mass, most commonly an adenoma, from a mass that requires treatment. CT and MRI are the most commonly used imaging tools in characterizing adrenal masses, with PET usually reserved for patients with known extra-adrenal malignancy. The imaging appearances on these studies reflect physiologic differences of adenoma from malignant masses: intracytoplasmic lipid content, contrast washout pattern, and metabolic activity.
CT is highly accurate in diagnosing adenoma, because both lipid content and washout characteristics can be used, as discussed later. The main advantages of MRI over CT are in patients in whom iodinated contrast is contraindicated because of allergy or renal insufficiency or in young patients in whom radiation exposure is a concern. The premise behind PET imaging is that malignant tumors are usually glucose avid because of increased metabolic activity. Most metastatic adrenal masses show increased activity, whereas most benign adrenal lesions do not. The need for imaging-guided biopsy to diagnose an adrenal mass has decreased in recent years as advances in adrenal imaging now allow accurate characterization of most adrenal masses. The imaging modalities used to characterize adrenal masses are summarized in Table 1 .
| Imaging Procedure | Rationale for Selection | Issues |
|---|---|---|
| CT | Most widely available Diagnosis based on density or CT washout | Contrast allergy and renal insufficiency (when contrast is necessary for diagnosis) Radiation in young patients |
| MRI | Young patients and patients with renal insufficiency | MR incompatible device (eg, pacemaker) |
| PET | Mostly in patients with known cancer | Not recommended in patients without a known malignancy |
Diagnostic imaging techniques
CT
Most adrenal masses are well visualized on routine abdominal CT, typically reconstructed at 5-mm thickness. Dedicated adrenal CT is performed when necessary to further characterize a known adrenal mass. Adrenal CT is performed with the patient in supine position as follows:
- •
Unenhanced sections are acquired through the adrenal gland with image reconstruction at 2 to 3 mm in axial and coronal planes.
- •
An elliptical region of interest (ROI) is placed in an adrenal mass. If the density of the adrenal mass measures ≤10 Hounsfield units (HU), then it is a benign lipid-rich adenoma and the examination is complete.
- •
If the density of the adrenal mass measures greater than 10 HU, then contrast material is injected intravenously.
- •
The next data sets are acquired at 60 seconds and 15 minutes after the start of contrast injection using the same CT acquisition parameters.
- •
Density measurements are obtained of the adrenal mass on unenhanced, dynamic, and delayed imaging, and percentage of contrast washout is calculated using the formula further discussed below.
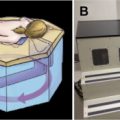
MRI
The principle MRI technique used in adrenal evaluation is chemical shift imaging (CS-MRI) obtained with in-phase and out-of-phase T1 gradient-recalled echo pulse sequences. CS-MRI exploits the different resonant frequencies of protons in fat and water molecules, with fat protons resonating at a slower frequency. Thus, at a predetermined echo time when the protons in fat and water molecules are out of phase, the net effect is signal cancellation within a voxel compared with when the protons are in phase. Most adrenal adenomas containing sufficient amount of lipid, thus, lose signal on out of phase compared with in phase. The lipid-rich adrenal adenoma will appear dark on out-of-phase imaging. When an adrenal mass is not diagnostic of an adenoma at CS-MRI, T2-weighted sequence and gadolinium-based, contrast-enhanced series are obtained for further characterization of an adrenal mass.
PET
PET and PET-CT utilizing fluorine-18-2fluoro-2-deoxy-D-glucose (FDG) are primarily performed in oncologic patients. To achieve and optimize a diagnostic scan, patients need to refrain from significant exercise for 24 hours, and their glucose level has to be less than 200 mg/dL before PET. At total-body PET-CT, CT, and PET are acquired separately. First, the patient receives intravenous administration of the FDG radiopharmaceutical, and then 75 minutes later, a CT without intravenous iodinated contrast is obtained followed immediately by PET acquisition. After these acquisitions, the CT images are fused (coregistered) with the metabolic PET dataset, which provides accurate anatomic localization of abnormal PET activity and also allows adrenal CT density measurements. These factors improve diagnostic performance of adrenal characterization in oncology patients.
Interpretation and assessment of clinical images
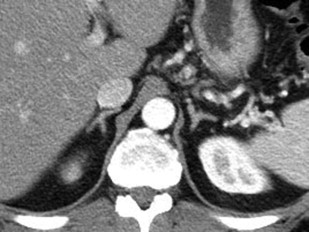
Adenoma
Adenomas are the most common adrenal lesion encountered in the general population, and most are not hyperfunctioning. Adenomas are typically well-defined, round, or oval masses of smooth margins and homogeneous density. One of the key diagnostic features of adenomas is the presence of intracellular lipid. Adrenal adenomas are composed of varying amount of intracytoplasmic lipid, and at unenhanced CT their density measurements are inversely related to the amount of lipid content. Based on this principle, adenomas can be separated from malignant masses using unenhanced CT density measurements. A threshold of 10 HU allowed adenoma to be diagnosed with 71% sensitivity and 98% specificity on a meta-analysis, and is the standard threshold used to diagnose a lipid-rich adenoma on CT ( Fig. 2 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree