Fig. 11.1
(a) Low-grade ductal carcinoma in situ (grade 1): low-grade monomorphic nuclei, inconspicuous nucleoli, diffuse chromatin, cells maintain polarity around gland-like spaces, no comedo necrosis. (b) Intermediate-grade ductal carcinoma in situ (grade 2): low- to intermediate-grade nuclei with mild size variation, occasional nucleoli, diffuse to coarse chromatin, polarity loss around gland-like spaces, may have comedo necrosis. (c) High-grade ductal carcinoma in situ (grade 3): high-grade pleomorphic nuclei, prominent nucleoli, coarse to clumped chromatin, usually solid with no nuclear polarity, comedo necrosis common. (d) Ductal carcinoma in situ with microinvasion: this is an example of ductal carcinoma in situ, grade 2, with microinvasion (pT1mi: ≤1 mm invasion) into the adjacent stroma
However, the natural course or history of untreated DCIS is really unknown, partially due to current surgical therapy that often removes the majority of the disease [1–3]. Additionally, the overall percentage of “nonprogressing” DCIS is unclear. There are some model estimates of the incidence of DCIS that will progress into IBC if left untreated as high as 100–270 per 100,000 [3, 4]. This model further estimates that women can survive >30 years with nonprogressing DCIS, while the average time interval for progressive DCIS to become IBC is 3 months, with the IBC remaining subclinical for about 2.5–3 years.
The incidence of DCIS has been increasing at a rapid rate since the 1970s, coinciding with the adoption of screening and diagnostic mammography as the key driver for this increase. Over 80 % of all DCIS is diagnosed initially by mammography, accounting for 17–34 % of all mammographically detected breast neoplasms [5, 6]. According to the Surveillance, Epidemiology, and End Results (SEER) program from 1975 to 2008, in situ disease (DCIS and LCIS) accounted for ~15 % of all new breast cancer diagnoses in the United States [7]. Thus, DCIS will account for about 22 % of all newly diagnosed breast cancers or 63,300 cases of DCIS for 2012 [8].
Although it is recognized that DCIS is likely an intermediary to the development of IBC, the risk of death from DCIS remains quite low. Utilizing the SEER database, the 10-year risk of death for DCIS that was diagnosed between the years 1984 and 1989 is 1.9 % [9]. This low rate is consistent with other studies examining the long-term outcomes of DCIS, consistently reported as <2 % at 10 years from diagnosis [10–12]. Although the risk of death from DCIS remains low, the risk of a local recurrence is estimated to be between 2.4 and 15 % at 5 years and 10–24 % at 10 years [13]. Achieving local control is clearly the preferred method of achieving both long-term survival and preventing a local recurrence.
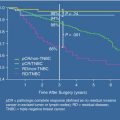
There is also a correlation between tumor grade and patient outcomes, consistently showing that a higher tumor grade (grade 3) is associated with a higher risk of local recurrence with DCIS and IBC compared to intermediate-grade (grade 2) or low-grade (grade 1) DCIS [13, 14]. Other factors associated with a higher risk of local recurrence are cellular architecture (comedo necrosis), the presence of microinvasion, multifocality, and possibly the lack of calcification. One possible tool available is the Van Nuys Index, developed to predict the chances of a local recurrence based upon four different predictors [15]. This predictive model is scored from 4 to 12, based upon tumor size, width of the negative margin, pathologic classification, and patient age, with each predictor scored from 1 to 3. Several studies have revealed a consistent correlation between the Van Nuys risk category and patient outcomes, showing that women within the highest risk category (Van Nuys score of 10–12) have a 224 % greater odds of mortality than women in the 4–6 risk category [16].
There are several demographic risk factors for the development of DCIS, and with few exceptions, with the same factors associated with the development of IBC. The incidence of DCIS is strongly related to age, with DCIS extremely uncommon in women younger than 40 years old. In fact, the incidence is only 2.5 per 100,000 for women ages 30–34, with a steady increase in incidence as the age increases, peaking at 96.7 per 100,000 women aged 65–69 [17, 18]. However, it should be noted that no matter what the age group, IBC is more common than DCIS. Other demographic risk factors associated with an increased likelihood of developing DCIS are race, urban versus rural living, lower educational level, and higher socioeconomic status. In terms of race, the incidence is highest for Caucasian women, followed second by African-American and Asian-Pacific Islanders.
Of note, caution should be taken when the younger patient, <40 years old, who present with DCIS, as they often present with some unique characteristics, such as a palpable mass, nipple discharge, or even breast pain. A recent study by Alvarado et al. shows that younger (<40 years old) patients with DCIS more often have multicentric disease, present with one or more clinical findings, and opt for, or require, mastectomy with immediate reconstruction [19]. Furthermore, the point is made that such patients should only be offered conservative surgery with an understanding that adjuvant radiotherapy will be delivered to the remaining breast.
Several reproductive factors have been shown to have a fairly weak association with an increased development of DCIS, such as late menopause (after 55 years of age), oral contraceptive use, and parity (age of first live birth <30 years of age) [20].
There does not appear to be any definitive evidence that the use of HRT is associated with an increased risk of DCIS. Biologic factors, such as density of the breast tissue, have also been examined. One study showed that premenopausal women with heterogeneous or extreme breast density had the highest risk of developing DCIS than women with scattered density [21]. Other studies have associated a strong family history of IBC or those with obesity, BRCA 1/2 mutational carriers, or a strong family history (high familial risk) with an increased odds for developing DCIS [22, 23]. Lastly, there is ample evidence that point to a protective effect from both tamoxifen and raloxifene for breast cancer prevention, with tamoxifen being more effective for preventing DCIS.
Initial Assessment
The initial assessment of the patient with DCIS begins with a thorough evaluation of all radiographic studies. This usually begins with a screening mammogram, with the vast majority of identified DCIS associated with a new area of microcalcifications when compared to previous films. The usual characteristics of suspicious or malignant-appearing calcifications are typically present, such as pleomorphic, grouped, linear, branching, irregular-shaped, and dystrophic calcifications. Comparative calcifications of a benign nature are generally larger, more rounded, and uniform in density, such as the “popcorn calcifications” associated with a fibroadenoma. Occasionally, DCIS may present initially as a palpable mass in about 10–15 % of all cases, also associated with a significantly higher potential for occult invasion, multicentricity, and locoregional recurrence [24, 25]. Several studies suggest that if left untreated, DCIS has the capacity to progress to invasive breast cancer in 30–50 % of all cases of DCIS [26, 27].
For DCIS, what is identified on the mammogram is often an underestimation of the entire extent of disease, as the DCIS is commonly found to extend along the ducts and may involve a large portion of the breast with multiple foci. Furthermore, even with the latest diagnostic imaging techniques, such as breast MRI, it is still difficult to accurately ascertain the true extent of DCIS. The Agency for Healthcare Research and Quality (AHRQ) as part of the US Department of Health and Human Services has thoroughly examined the utility of the increasing use of breast MRI and its impact upon treatment and outcomes for patients with DCIS [28]. The authors concluded that breast MRI consistently results in changes in treatment, primarily due to a differential ability for it to detect multicentric and contralateral disease, as well as accurately estimate the size of the tumor.
In our practice, we have incorporated breast MRI as an additional tool that often provides supplemental information, in addition to other studies, that is important to discuss with patients in determining the most appropriate operative intervention. It is not uncommon to obtain a breast MRI for patients with a 1.5 cm diameter area of grade 2/3 microcalcifications identified on mammography to ultimately have a much wider diameter area found on breast MRI. Additionally, contralateral abnormalities are often identified, with many found to be biopsy-proven high-risk lesions or even invasive cancer. Of course, this will greatly change the subsequent discussion with our patients, outlining the findings in detail and how this will impact the ultimate operative approach.
We should also point out the significance of additional areas identified on MRI that are deemed suspicious and requiring further intervention. Such areas may further require a biopsy or even a 6-month follow-up study with ultrasound or repeat MRI. Many patients at this point simply “throw in the towel,” not wanting to delay their treatment any further with possible further diagnostic testing and biopsy. Most will opt for definitive and expeditious treatment of their cancer with mastectomy. Lastly, once the latter decision is made, many patients will further wish to discuss the risks, advantages, and disadvantages of contralateral prophylactic mastectomy for maximal risk reduction and, secondly, for improved symmetry and cosmetic outcome associated with bilateral breast reconstruction. Of importance, many patients will often strongly express their desire to obtain some semblance of “peace of mind,” not wanting to have to worry about developing breast cancer in the contralateral breast in the future. Although it is well established that patients will overestimate their risk, many will still opt for contralateral mastectomy for this reason.
Surgical Management
The surgical management of DCIS is dependent upon a number of factors. One important factor that will ultimately determine the most appropriate surgical approach is the overall size (diameter) of the DCIS. Both mammogram and ultrasound can be very useful in determining the overall size of the area and whether it is multifocal or multicentric. If either is still indeterminate, breast MRI may be beneficial as an adjunct to further assessing the area in question. Once the area has been determined to be unifocal, a discussion about breast conservation can be pursued with the patient.
Once the final pathology has been reviewed, it is important to discuss whether the DCIS is pure low grade, intermediate grade, or high grade, with or without microinvasion (DCISM). We generally divide our operative approach based upon the overall grade of the DCIS, with low-grade DCIS having the smallest chance of spreading to the adjacent draining nodal basin (usually <2 %). Thus, for patients with pure low-grade DCIS, we do not recommend sentinel lymph node mapping as part of breast conservation. However, we spend some time discussing the importance of adjuvant hormonal and radiation therapy.
Achieving local control is the key to good overall patient outcome and preventing local recurrence. Positive surgical margins (tumor at ink) are consistently shown to be associated with increased DCIS and invasive breast cancer recurrence [29–31]. In our practice, we plan our operative approach with attempting to remove the specimen with 10-mm margins of normal-appearing surrounding breast tissue. Upon removal of the lumpectomy specimen, we orient the specimen (short superior stitch at 12 o’clock and a long lateral stitch at 3 or 9 o’clock) followed by an intraoperative specimen radiograph in order to confirm that the previously placed core biopsy clip has been removed and is within the central portion of the lumpectomy specimen.
Additionally, we then send over the lumpectomy specimen for margin analysis, which involves the pathologist. The pathologist will first gross the specimen followed by inking of all of the surgical margins and subsequent serial gross sectional analysis of the tumor itself and biopsy cavity. A gross measurement is then made in order to assess the closest margin to the tumor, and if less than 2 mm by gross measurement, we will re-excise this margin intraoperatively.
We then await the final pathology based upon any re-excision margins that have been removed. It is uncommon that a return to the operating room is required due to a positive margin, occurring in <5 % of all cases of lumpectomy for DCIS. If the final margins are found to be <2 mm and assuming there is further tissue to be removed with re-excision, we will offer the patient a re-excision of margins in order to achieve negative margins. If there are multiple margins involved with DCIS, we will recommend a completion mastectomy in order to clear extensive, multifocal DCIS. If the deep margin is <2 mm or focally involved and the pectoralis fascia has been previously removed, then we do not recommend a return to the operating room. We will send this patient for radiation therapy with a likely boost to this area.
For patients identified with having either intermediate-grade DCIS, high-grade DCIS, or DCISM, we recommend concomitant sentinel lymph node mapping of the draining ipsilateral nodal basin. The likelihood of identifying SLN positivity in the intermediate- to high-grade group (without microinvasion) is between 5 and 10 % and those with microinvasion between 10 and 16 % [32, 33]. Even so, such positive findings in the SLN in any of these groups are likely to be either micrometastatic disease or isolated tumor cells (ITC’s), with little, if any, overall impact on ultimate survival or outcome [32, 33]. However, there remains uncertainty in the preoperative setting as to the accurate identification of pure low-grade DCIS, often found to be upstaged to either intermediate- or high-grade DCIS, DCISM, or even invasive breast cancer. Thus, we discuss the nuances of performing SLNB in all of our patients with DCIS, clearly outlining the above findings and coming to a consensus with the patient about performing SLNB in the setting of DCIS.
There are other situations where SLNB may be justified in patients with DCIS, such as those with high-risk factors for harboring occult invasion. Preoperative factors for harboring occult invasion are older patient age, diagnosis by core needle biopsy, large-diameter DCIS, comedo-type necrosis, high-grade (grade 3) DCIS, a palpable mass, and tumor visible by ultrasound [32, 33]. For those patients that present with a palpable mass, which can be seen in 10–20 % of all cases of DCIS, it is very likely that there will be adjacent areas of invasive cancer found in about 25–35 % of all cases.
Therefore, we would strongly recommend SLNB as part of BCT. The last reason to perform SLN mapping are for those patients with DCIS who are undergoing a mastectomy. Recently, Shah et al. examined the SEER database to identify those patients with DCIS (all grades) between the years 2000 and 2008 (total of 20,177) who also underwent a SLNB as part of the operation [34]. They found that 51 % of all patients did not undergo a SLNB as part of the mastectomy procedure, with various reasons for this low percentage of patients being offered SLNB.
There is ongoing debate as to the benefit of performing a SLNB in patients with DCIS when compared to those with invasive breast cancer. Recent results from the ACOSOG Z10011 trial have examined the role of SLNB in patients with IBC (not DCIS). They conclude that there is no difference in either disease-free or overall survival in those patients with invasive breast cancer who have limited disease within the SLN and subsequently undergo a completion axillary lymph node dissection [35]. Clearly, the role of performing a SLNB in patients with DCIS can be questioned in many cases, with much of the decision based upon the grade of the DCIS, the presence of microinvasion, and the level of suspicion for concomitant areas of unrecognized invasive disease.
Adjuvant Therapy for DCIS
Based upon the current literature, it is clear that patients who have undergone operative removal with BCS (lumpectomy) for their DCIS should follow with adjuvant radiation therapy. Whole breast radiation therapy following BCS is associated with a significant reduction of local DCIS recurrence, with little, if any, impact upon improving overall survival. Both prospective and retrospective studies have demonstrated excellent long-term outcomes at 10 and 15 years after BCT with radiation. There have been four prospective, randomized trials that have extensively examined the utility of adding radiation therapy after lumpectomy, with all showing that the addition of radiation therapy after lumpectomy reduces the risk of local recurrence by about 50 % and for a subset of invasive local recurrence [10, 31, 36–40]. Thus, it is clear that radiation therapy after lumpectomy is an important adjuvant treatment option for patients undergoing BCT with lumpectomy.
However, it is much less certain as to a defined subset of patients that may not benefit from adjuvant radiation therapy. It is likely that not all patients with DCIS require radiation therapy after BCT, but there is a lack of evidence supporting its omission in suspected low-risk patients. To date, there has yet to be a definitive trial that has been able to identify such a group of patients who do not benefit from adjuvant radiation therapy as part of BCT for patients with DCIS. Some studies suggest that if one is able to obtain a >10 mm or greater surgical margin on the lumpectomy specimen, then it may be possible to eliminate the need for adjuvant radiation therapy [41–43].
Current areas of controversy:
1.




Do we overdiagnose and potentially overtreat DCIS? It is quite likely that we are overdiagnosing and overtreating a fair proportion of patients who present with early findings based upon screening mammography. Recently, the independent UK Panel on Breast Cancer Screening addressed this very question, on whether breast cancer screening does more harm than good [44]. They provide the best available data for the UK setting, based upon a meta-analysis of 11 randomized trials examining the role of breast cancer screening and observational studies of the relative risk of breast cancer mortality for women invited to screening compared to controls. The panel concludes that there is about a 20 % relative risk reduction for those who undergo regular screening mammography, with a best estimate of overdiagnosis in the range of 11–19 %. This translates into about 1 % being overdiagnosed in the next 20 years for >300,000 women aged 50–52 who are invited in the United Kingdom to be screened every year.
To the contrary, Wallis et al. report that incidence of DCIS rose rapidly since the inception of the National Health Service Breast Screening Programme (NHSBSP) in 1988 [45]. Many consider this rapid increase a representation of both overdiagnosis and overtreatment, with Wallis et al. reporting on the long-term follow-up of 700 noninvasive breast cancers (DCIS) over the first 10-year screening period (1988–1999). After a median follow-up of 183 months (range of 133–259 months), 102/700 (14.6 %) patients were identified with a first local recurrence, with 49/102 (48 %) being invasive breast cancer. The median time to the first noninvasive recurrence was 15 months and 60 months for invasive cancer. Additionally, they show that high-grade DCIS initially is associated with a much shorter interval to local recurrence with invasive recurrence (76 months) compared to those with low-/intermediate-grade DCIS (131 months). Thus, even with short-term follow-up, there will be a significant number of missed events, especially with invasive breast cancer as the first local recurrence.
Bleyer et al. utilized the SEER data to examine the trends from 1976 to 2008 for the incidence of early-stage breast cancer (DCIS and localized disease) and late-stage breast cancer (regional and distant disease) among women >40 years old [46]. They report that as a direct result of screening mammography, the number of cases of early-stage breast cancer that are detected each year has doubled, from 112 to 234 cases per 100,000 women in the United States. They further estimate that breast cancer was overdiagnosed (i.e., tumors are found by mammography that would not have led to clinically apparent disease) in 1.3 million women in the past 30 years. In 2008, they estimate that breast cancer was overdiagnosed in >70,000 women, accounting for 31 % of all breast cancers diagnosed that year. This study is supported by several other studies that examine this issue of overdiagnosis of not just DCIS but of invasive breast cancer [47]. Although these studies raise serious questions about the value of screening mammography to our respective societies, it is a much more complicated task to distill down the ever-increasing data in order to discuss the treatment decisions to be made with our patients.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree