| Characteristic | Spasmodic croup | Laryngotracheobronchitis | Bacterial tracheitis | Supraglottitis |
|---|---|---|---|---|
| Age range | 6 mo–3 yr | 0–6 yr (peak, 6 mo–3 yr) | 1 mo–6 yr | Infants ≤2 mo, older children, and adults |
| Etiology | ? Viral ? Airway reactivity | Parainfluenza virus (1, 2, 3) Influenza Respiratory syncytial virus Adenovirus | Staphylococcus aureus Haemophilus influenzae Corynebacterium diphtheriae | Haemophilus influenzae (Hib/non-b) Streptococcus pneumoniae Group A streptococcus Haemophilus parainfluenzae |
| Onset | Sudden | Insidious | Rapid deterioration | Sudden |
| Clinical manifestations | Afebrile Nontoxic Barking cough Stridor Hoarse | Low-grade fever Nontoxic Barking cough Stridor Hoarse | High fever Toxic Barking cough Stridor Hoarse | High fever Toxic Nonbarking cough Muffled voice Drooling Dysphagia Sitting, leaning forward |
| Endoscopic findings | Pale mucosa Subglottic swelling | Deep-red mucosa Subglottic swelling | Deep-red mucosa Copious tracheal secretions | Cherry-red epiglottis Arytenoepiglottic swelling |
| Complete blood count, differential | Normal | Mild leukocytosis Lymphocytosis | Normal to mild leukocytosis Marked Bandemia | Marked leukocytosis Bandemia |
| Radiographic findings | Subglottic narrowing | Subglottic narrowing | Subglottic narrowing Irregular tracheal border | Large epiglottis Thick arytenoepiglottic folds |
| Therapy | Mist Calm ?Racemic epinephrine ?Steroids | Corticosteroids Racemic epinephrine Nebulized budesonide Intubation (if necessary) | Intubation Antibiotics | Intubation Antibiotics |
| Response | Rapid | Transient | Slow (1–2 wk) | Variable (hours–days) |
| Intubation | Rare | Occasional | Usual | Usual |
Croup usually follows a relatively mild upper respiratory infection. Its onset is commonly abrupt and occurs in the late evening and night. Viral infection with associated inflammation of the nasopharynx spreads inferiorly to the respiratory epithelium of the larynx and trachea. The subglottic region in children is normally narrow and surrounded by a firm ring of cartilage. Small swelling of this narrow subglottic area will significantly restrict air flow and produce audible inspiratory stridor, while the impairment of the mobility of the vocal cords will produce hoarseness.
Rapid, objective, and calm assessment of severity must be done to determine management and without respiratory compromise. The presence of chest wall retractions and stridor at rest are most critical (Table 30.2). Anteroposterior radiologic examination of the soft tissues of the neck (with medical monitoring) may be useful when the diagnosis is in question. The classic steeple sign is produced by the cone-shaped narrowing of the proximal 1-cm subglottic area of the trachea, at the conus elasticus to the level of the true vocal cords. It is produced by edema with elevation of the tracheal mucosa and the loss of the normal lateral convexities (shoulders) of the air column (Figure 30.1). Direct visualization of the airway can be attempted if the symptoms are not typical and the child is stable. If intubation appears imminent or there is a strong suspicion of epiglottitis, this should be performed under anesthesia. In croup, the supraglottic region appears normal.
| Condition | Treatment |
|---|---|
| Mild | |
| No stridor No chest wall retractions No respiratory distress at rest | Analgesics, hydration as needed Single dose of oral dexamethasone (0.6 mg/kg body weight) Educate parents (illness, when to seek medical assessment) |
| Moderate | |
| Stridor at rest Mild chest wall retractions No agitation or significant respiratory distress | Above including oral dexamethasone, 0.6 mg/kg Observe in emergency room If improved with no stridor or retractions, educate, home If no or minimal improvement by 4 h, hospitalization |
| Severe | |
| Stridor may decrease with worsening airway obstruction Significant respiratory distress Severe chest wall retractions Agitation or lethargy Decreased air movement Possibly cyanosis | Nebulized racemic epinephrine 2.25% (0.5 mL/2.5 mL saline) or L-epinephrine 1:1000 (5 mL), may repeat Oral or parenteral dexamethasone 0.6 mg/kg, may repeat If contraindications to oral medication, consider nebulized budesonide 2 mg with epinephrine Humidifed oxygen (≤92% room air 02 sat, consider heliox) ICU care, intubation as necessary |
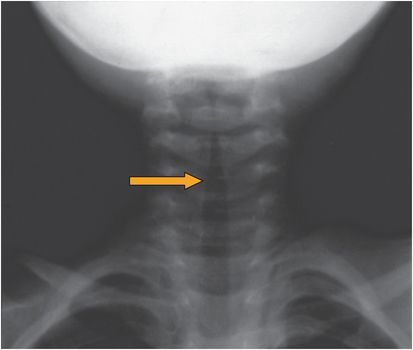
Figure 30.1 The “steeple sign” of croup. Anteroposterior radiograph of the upper airway (arrow) of a patient with croup. (Courtesy of Drs. A. Weber and H. D. Curtin, Dept. of Radiology, Massachusetts Eye and Ear Infirmary, Boston, MA.)
Therapy
Management includes corticosteroids, nebulized budesonide, and nebulized epinephrine. Oxygen or heliox are often used as supportive treatment. No clear data exist on the benefits of mist or humidified air. Analgesics improve sore throat and overall comfort. Antitussives, decongestants, and “prophylactic” antibiotics are not beneficial.
Due to the sustained anti-inflammatory effects of corticosteroids, they have been shown to improve the status of not only severe croup but also mild to moderate croup. Dexamethasone in doses of 0.15 to 0.6 mg/kg has been shown to be beneficial and decreases the need for hospitalizations and unscheduled medical visits even in mild croup. Oral, intramuscular, and intravenous routes of administration are all effective, with nebulized dexamethasone possibly less effective. Nebulized budesonide, 2 mg, has been shown to be as effective as dexamethasone but is often reserved for patients with intractable vomiting or for simultaneous administration with epinephrine in severe respiratory distress because it is substantially more expensive and more difficult to administer. The combination of oral dexamethasone and nebulized budesonide is no better than either alone. For the management of outpatient croup, oral prednisolone, 2 mg/kg/day as two divided doses per day, may be considered as an alternative, but comparison studies have been limited to oral dexamethasone.
Owing to the rapid onset of action, the use of nebulized racemic epinephrine has markedly reduced the need for intubation, even in hospitalized patients, to less than 2%. L-epinephrine (1:1000) is as effective as racemic epinephrine. Improvement occurs within minutes, but symptoms can recur within 2 hours; therefore, patients must be observed in the emergency room for 3 hours.
The administration of oxygen should be reserved for children with significant respiratory distress and hypoxia (oxygen saturation on room air ≤92%).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





