Coronary Heart Disease: Introduction
Data from the National Center for Health Statistics have noted that the life expectancy at birth in the United States reached a record high of 77.5 years in 2003, attributable, in part, to the decline in mortality from heart disease during the past three decades. Despite this, coronary heart disease (CHD) remains the leading killer of both men and women in the United States. More than 80% of CHD deaths occur in persons older than 65 years of age. In addition, 37% of recognized acute myocardial infarctions (MIs) occur in those older than 75 years of age, and, although these account for roughly 6% of the U.S. population, 60% of all MI-related deaths affect elderly patients 75 years of age or older.
The diagnosis, management, and posthospitalization care of elderly patients with CHD involve interplay of patient heterogeneity, comorbid conditions, functional status, drug pharmacology, and biological differences. This complexity is compounded by extrapolation of “evidence-based care” obtained from cardiovascular trials from which older patients were poorly represented. Given these characteristics, an adopted approach to cardiac care of elderly patients often requires developing a patient-centered plan of care and incorporating an individual’s own goals and health expectations in the care decision process. While the term “elderly” has been used in the literature, no specific guideline to the care of elderly patients with CHD attributes a particular level of evidence to specific age. This chapter will reference specific age groups reported in the medical literature as available, bearing in mind that one’s chronologic age may be a poor surrogate for one’s overall health status.
Prevalence
The spectrum of CHD includes asymptomatic (or subclinical) CHD, chronic stable angina pectoris, unstable angina, and acute MI. Statistically, the first manifestation of CHD is an acute MI in 40% of cases and sudden death in 10% to 20% of cases. In the United States, the prevalence of overt CHD increases in a curvilinear fashion with advancing age in both men and women (Figure 76-1). Similarly, the annual rate of first heart attack rises with age in all race and gender subgroups. Furthermore, despite the fact that women typically have a 10-year lag in developing CHD as compared to men, the majority of patients with CHD ≥75 years of age or older are women because they typically have a longer lifespan.
It should also be realized that overt CHD represents just the tip of the coronary disease iceberg and a great number of elderly patients have asymptomatic, subclinical disease. Researchers for the Cardiovascular Health Study examined the prevalence of both clinical and subclinical cardiovascular disease in a large community-dwelling Medicare population by using a composite measure of MI on electrocardiogram (ECG) or echocardiography and abnormal carotid artery wall thickness or ankle–brachial blood pressure index and found that disease frequency increased from 22% in women aged 65 to 70 years to 43% in those aged 85 years or older. Similarly, the frequency of subclinical vascular disease in men increased from 33% to 45% in these age groups, respectively.
Effects of Aging on the Cardiovascular System
The development of CHD is multifactorial and can be influenced by genetic predisposition and comorbid conditions such as diabetes, as well as environmental and lifestyle determinants such as diet, smoking, and physical exercise. Not surprisingly, as these factors vary among individuals, one’s likelihood for developing CHD also varies. While it is often believed that CHD is inevitable with advancing age, autopsy studies have found that 40% of those persons in their nineties will not have occlusive coronary disease.
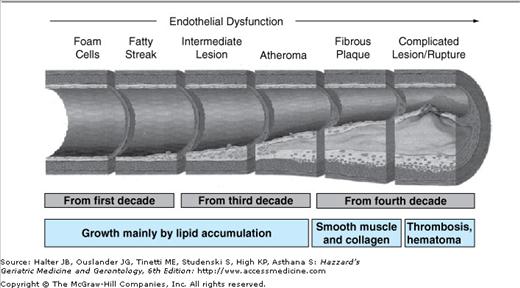
With this patient-to-patient variability noted, certain cardiovascular changes are seen more commonly with advancing age, and the aging process confers important physiological considerations in elderly patients. Diastolic heart failure, “heart failure with preserved ejection fraction,” accounts for up to 50% of heart failure in patients older than 70 years of age and often coexists with vascular disease, contributing to significant morbidity and mortality. The exact mechanism of diastolic heart failure continues to remain controversial, but altered left ventricular end-diastolic pressures and increased pulmonary venous pressures can result in symptoms of dyspnea and signs of pulmonary edema. This disease process occurs with a higher prevalence in elderly patients with a history of hypertension and atrial fibrillation. Recent observational data suggest that rehospitalization or 1-year survival mirrors that of systolic heart failure, challenging earlier assumptions that diastolic heart failure might be a more benign condition. In parallel, arterial stiffening in elderly patients results in isolated systolic hypertension and widened pulse pressures, factors previously associated with increased cardiovascular events. The aging of the vasculature often heralds blunted responses to protective vasodilatory mediators and progressive endothelial dysfunction. This endotheliopathy results in increasing numbers and severity of atherosclerotic plaques (Figure 76-2). The composition of these lesions also changes with age, with reduction in the soft lipid core and an increase in calcification and fibrosis. While more advanced calcified plaques are actually less likely to rupture, the sheer increase in lesion numbers leads to an increased overall likelihood for CHD events in the elderly patient.
Presentation
The elderly are much less likely than younger patients to present with “classic” exertional chest heaviness. Instead, older patients more often complain of a vague feeling of dyspnea, abdominal pain, fatigue, confusion, or malaise that may be misinterpreted as consequences of aging or other comorbid illness. Findings from the Global Registry of Acute Coronary Events, a large, prospective, multinational registry of acute coronary syndromes (ACSs), demonstrated that patients presenting with atypical symptoms were less likely to receive appropriate cardiac medications, undergo cardiac catheterization, and were at higher risk of in-hospital morbidity and mortality. The elderly can also have an impaired ischemia warning system, which delays their CHD presentation. In a series of patients with CHD undergoing treadmill testing, researchers found that patients aged >70 years took more than twice as long as their younger counterparts to report anginal symptoms after ECG-documented ischemia was noted. In the Worcester Heart Attack Study, patients 75 years of age and older had the longest prehospital delay of any age group, many outside the critical 6-hour window for fibrinolytic therapy. The Rapid Early Action for Coronary Treatment study quantified delay time as an additional 14 minutes for every 10-year increment in age, beginning with the age of 30 years. The significant prehospital delay among elderly patients is likely multifactorial and includes considerations such as atypical presentation, medical comorbidities, previous experiences within the health-care system, socioeconomics, access to care, and cognitive and functional impairments.
Difficulty in recognizing symptoms contributes to later presentation for acute CHD events in the elderly. In fact, studies show that more than two-thirds of patients with MI, >65 years of age, fail to reach an emergency department within 6 hours after the onset of their symptoms. Major predictors of a delay in MI presentation include advanced age, female sex, diabetes mellitus, and social isolation. Importantly, delays in MI presentation have strong prognostic implications and are closely associated with poorer outcomes in elderly patients. Thus, clinicians should proactively discuss with their patients that cardiac symptoms can vary widely and they should seek rapid medical attention if potential ischemic symptoms occur.
Diagnostic Evaluation
Given its prevalence and often atypical presentation in the elderly, clinicians must harbor a high index of suspicion for CHD in order to make the correct diagnosis. In taking a thorough clinical history, with emphasis on prior cardiovascular disease history, clinicians must pay close attention to assessing a patient’s major cardiac risk factors (smoking, hypertension, diabetes mellitus, and lipid status), as well as any symptoms suggestive of CHD. Eliciting the temporal course of these symptoms is also important. Patients with new, progressive, or refractory symptoms typically require an expedited—and possibly inpatient—evaluation, in contrast to those patients with chronic stable symptoms. Physicians should also assess the impact of symptoms on the patient’s functional status and overall quality of life, as these issues may alter preferences for invasive testing and/or need for coronary revascularization.
A systematic approach to the physical examination with awareness of age-related changes in the cardiovascular system may improve diagnostic accuracy and provide further clues to the presence of CHD. After evaluation of the patient’s general appearance, blood pressure assessment with an appropriately fitting sphygmomanometer, one that encircles at least 80% of the arm, and examination of pulses in the extremities should be performed. Some older patients develop calcific vascular disease, and pseudohypertension may be observed. This becomes an important distinction when further titration of antihypertensive medications may predispose the patient to symptoms of cerebral hypoperfusion. Dimunition of the femoral pulses or brachial–femoral delay may suggest the presence of atherosclerotic aortoiliac disease, and these findings may accompany observed dermatological changes with lower extremity hair loss. Performing ankle–brachial indices remains a useful and sensitive screening tool for identifying patients with peripheral vascular disease, a known risk factor for increased cardiovascular events. The cardiac examination may include signs of left- or right-sided heart failure (pulmonary edema, displaced point of maximal impulse, an S3, or peripheral edema) or characteristic murmurs of valvular heart disease. Once a thorough history and physical has been completed, further diagnostic evaluation should be based on the patient’s symptoms as outlined below.
For the asymptomatic elderly individual, risk factors, particularly blood pressure and lipid screening, should be measured as recommended for all aged patients in the Joint National Committee on Detection, Evaluation and Treatment of High Blood Pressure (JNC) VII and National Cholesterol Education Program (NCEP)—Adult Treatment Panel (ATP) III guidelines, as the elderly continue to remain the population with the lowest rates of blood pressure control. Obtaining a baseline ECG is also reasonable in the initial patient evaluation because of the high prevalence of “silent” MIs in the elderly population. This information should be summarized into a composite risk assessment using one of the multiple standardized indexes such as the Framingham Risk Score (http://www.framinghamheartstudy.org/risk/index.html).
Patients with low CHD risk (10-year CHD risk <5%) can generally be reassured without further testing, with a plan for reevaluation of their risk factors in 5 years. In contrast, patients at high risk (10-year CHD risk >20%) should receive aggressive risk factor intervention to the same degree as if they had already experienced an overt CHD event. Patients with intermediate risk (10-year CHD risk, 5–20%) may benefit from further testing to clarify their CHD risk. In these intermediate patients, laboratory studies such as homocysteine, lipoprotein (a), B-type natriuretic peptide, and C-reactive protein have been proposed as means of identifying those at higher risk and in need of more aggressive risk-factor modification. Recently, this “multimarker” strategy was evaluated in a study of the Framingham Offspring cohort. The findings suggested that for outcomes of death or first major cardiovascular events, multimarker scoring added only a small increase to conventional risk factors in the ability to classify risk. Therefore, the role of biomarkers to aid in risk stratification of patients who are ambulatory remains an area of ongoing research, and its implications for clinical practice have yet to be clearly elucidated. Beyond the standard history, physical examination, and simple laboratory tests, further diagnostic testing (carotid ultrasound, treadmill testing, echocardiography, or electron-beam computed tomography) in the asymptomatic elderly patient to detect occult or subclinical CHD remains controversial and is not generally recommended.
Elderly patients with symptoms suggestive of CHD should undergo a similar assessment of their likelihood for obstructive coronary disease based on algorithms that take into account symptom characteristics, including angina type (nonanginal, atypical, or typical), its course (stable, progressive, or unstable), and its duration. This initial assessment of a patient’s “pretest probability of disease” should then guide further diagnostic testing. In particular, clinicians need to be cognizant that, according to Bayesian theory, the predictive value of a test is influenced by the disease prevalence in the population tested. For example, clinicians may interpret a negative stress test in a high-risk elderly woman (pretest probability of disease 80%) as “ruling-out” the presence of CHD, whereas this patient’s post-test likelihood remains more than 60% (Table 76-1). For these reasons, elderly patients with high pretest likelihood for coronary disease should be considered for direct referral for cardiac catheterization (if revascularization is an appropriate option). At the other extreme, patients with a low pretest probability for CAD ≤20% (i.e., no risk factors, normal ECG, and very atypical symptoms) can often be followed clinically and/or be assessed for other etiologies of their symptoms (gastrointestinal, pulmonary, musculoskeletal, etc.). Elderly patients with an intermediate pretest probability for CHD (between 20% and 70%) are those in whom stress testing tends to have its greatest impact on clinical decision making.
HISTORY | AGE (yr) | PRETEST LIKELIHOOD OF SIGNIFICANT CAD* (%) | TREADMILL TEST† | POSTTEST LIKELIHOOD OF SIGNIFICANT CAD (%) |
|---|---|---|---|---|
Female, typical CP | 45 | 30 | Positive | 56 |
↑ Lipids | Negative | 16 | ||
75 | 80 | Positive | 92 | |
Negative | 63 | |||
Female, atypical CP | 45 | 5 | Positive | 12 |
No RF | Negative | 3 | ||
75 | 35 | Positive | 62 | |
Negative | 18 |
When a stress test is indicated, current guidelines still recommend standard exercise ECG as the test of choice for most patients. These tests provide very important prognostic information (including exercise duration and hemodynamic response), as well as electrocardiographic indications of ischemia (ST depression). Elderly patients, however, frequently experience difficulty with traditional stress testing because of deconditioning or comorbid illness or disability and may benefit from modified exercise protocols with lower starting levels and slower stage progression. Alternatively, for patients who cannot exercise sufficiently, one can use a pharmacologic-based stress test (dobutamine, adenosine, or dipyridamole).
In elderly patients with baseline ECGs abnormalities (resting ST depression, left bundle branch block, left ventricular hypertrophy with strain, or paced rhythms), imaging modalities, such as nuclear perfusion or stress echocardiography, are required. While these modalities significantly add to the cost of the test, these improve the diagnostic accuracy beyond stress ECG alone and provide information as to the location and extent of coronary disease. The published sensitivity and specificity for stress echocardiography and nuclear imaging (80–90% for each) are nearly identical in most series. Thus, the choice between the two should be based on local availability and expertise.
The use of cardiac catheterization in the elderly patient needs to be based on its potential risk–benefit ratio. While cardiac catheterization has become commonplace and relatively safe in contemporary practice, vascular injury, bleeding, MI, stroke, and even mortality can result, albeit rarely. Advanced age increases these risks slightly; however, the risk to life remains <0.2%, and the risk of other serious adverse events is <0.5%, even in those aged ≥75 years. Placing a patient even at minimal risk, however, is not worthwhile if the information obtained from a catheterization is unlikely to impact treatment decisions. For example, a cardiac catheterization may have limited impact on the management of an elderly patient who is not a candidate for coronary revascularization, based on medical comorbidity, cognitive decline, or personal preference.
Acute Coronary Syndromes
The pathophysiology of the ACS involves atherosclerotic plaque rupture, platelet activation/aggregation and embolization, endothelial dysfunction, inflammation, and thrombus formation. If the clot completely occludes the vessel, the patient suffers an acute MI, and an injury pattern (e.g., ST elevation) is often seen on the ECG. In contrast, patients with plaque rupture can also form a nonocclusive thrombus, resulting in subendocardial ischemia. These patients often have an acceleration of chest pain symptoms (unstable angina) and may have more subtle changes on the ECG (e.g., flipped T waves or ST depression). There is some evidence that plasma levels of procoagulation markers and coagulation factors are elevated in elderly patients, but it remains unclear whether these findings alone are responsible for increased thrombotic tendencies in the elderly or alter risk when accompanied by other traditional risk factors for thrombotic events.
There are also significant proportions of elderly patients who develop ACS secondary to exacerbations of chronic comorbid conditions or acute medical illnesses. These include sepsis, acute blood loss or chronic anemia, pneumonia, pulmonary embolism, chronic obstructive pulmonary disease, congestive heart failure, dysrhythmias, or hypertensive urgencies. A recent retrospective study demonstrated that approximately 30% of patients present with an acute noncardiac condition concomitant with an MI, contributing to increased in-hospital mortality and variations in receipt of cardiac medications and invasive cardiac therapies. These “secondary” ACSs usually occur in the context of increased myocardial oxygen demand or hemodynamic stress in patients with underlying coronary artery disease and represent a substantial number of cases.
Elderly patients who present with ischemic-type symptoms, which are rapidly progressive, severe, and refractory or which occur at rest, should be immediately transferred to an emergency care setting for further evaluation. Initial testing for myocardial damage should consist of an ECG and cardiac biomarkers (troponin [I or T] and/or creatinine kinase isoforms [CK-MB]). Some patients will have clear ST elevation, making the diagnosis of ST-segment elevation MI (STE MI) straightforward. In others, however, the ECG may be nondiagnostic and the diagnosis often being confirmed by elevations and temporal trends of cardiac biomarkers, with or without accompanying EKG changes. These patients are classified as having non-ST-segment elevation ACS (NSTE ACS).
Prognosis
Multiple studies have shown that once CHD is manifested, the risk of morbidity and mortality increases steadily with age. In two very large randomized trials of patients having with ST elevation, age was the single strongest predictor of both short- and long-term mortality, with the risk of death increasing 6% with each year after 65 years of age. In another large registry population, patients aged 65 to 74 years admitted for an MI were four times more likely to die during the hospitalization than those aged 55 or younger. This risk rose to greater than 10 times higher for patients aged ≥85 years. Elderly patients are also much more likely to suffer complications from their MI, including heart failure, cardiogenic shock, cardiac rupture, atrial fibrillation, stroke, acute renal insufficiency, and pneumonia. Finally, patients aged ≥75 years were three times more likely to be discharged to a nursing facility after an acute MI than those aged 65 to 69 years.
The reasons for increasing MI mortality and morbidity as a function of advancing age are multifold. Elderly patients have less cardiac reserve and more comorbid illness (e.g., pulmonary, renal, and cognitive impairments), limiting their ability to compensate for cardiac events. Also, as noted above, the elderly often present with “secondary” MIs where the cardiac event is a complication of another potential mortal primary process (i.e., sepsis), leading to high mortality. Finally, the elderly patients with MI present later, often receive less aggressive medical care, and undergo fewer potentially life-saving invasive procedures than younger patients.
The primary objective in the management of patients with STE MI is to provide early reperfusion therapy with either pharmacological means (i.e., fibrinolysis) or percutaneous intervention with balloon angioplasty. Numerous studies have confirmed that reperfusion therapy (fibrinolytic therapy or primary angioplasty) in patients presenting with acute STE MIs improves survival if performed in a timely fashion. An overview of the major thrombolytic trials from the Fibrinolytic Therapy Trialists’ Collaborative Group, a meta-analysis that included more than 58 000 patients, demonstrated a 15% relative risk reduction in death for patients 75 years of age or older with STE MI or bundle branch block treated with fibrinolytics. Despite elderly achieving a smaller relative reduction in death than younger patients, the trend toward absolute benefit in terms of lives saved with fibrinolytics was threefold greater in patients older than 75 years of age compared with those younger than 55 years.
In addition, an adjusted observational analysis from two studies using the Cooperative Cardiovascular Project database reported that patients aged ≥75 years actually had higher 30-day mortality with fibrinolysis than with standard medical therapy. Interestingly, in the one analysis that looked at 1-year outcomes, this early treatment risk in the very elderly reversed itself, and those treated with lysis actually had better survival rates after this interval (OR 0.84, 95% CI 0.79–0.89).
The possible therapeutic benefits of thrombolysis must be weighed carefully against the risks, especially in the elderly. Data from the Fibrinolytic Therapy Trialists’ meta-analysis showed that patients aged >70 years had nearly a threefold higher relative risk of intracranial hemorrhage, the most feared complication in the postlytic period, after fibrinolysis than those aged <60 years. Bearing this in mind, clinicians should realize that intracranial hemorrhage is a rare event and the absolute risk of this complication after fibrinolysis in those >70 years remains between 0.7% and 2.1% in major trials and nearing 3% in those older than 85 years of age. The risk factors for intracranial hemorrhage include low body weight, elevated blood pressures, facial or head trauma, and dementia. Dementia was found in one trial to significantly increase the risk for intracranial hemorrhage by threefold.
In contrast with these mixed results for fibrinolysis, reperfusion for STE MI with timely percutaneous transluminal coronary angioplasty (PTCA) is almost universally associated with improved outcomes in all age groups. For example, a recent randomized study of primary PTCA versus thrombolysis in patients with STE MI showed a 40% relative risk reduction for death, MI, and stroke in patients treated within 3 hours of presentation with PTCA. Primary PTCA in treatment of MI in the elderly is also supported by a series of observational analyses. In the Cooperative Cardiovascular Project analysis, acute PTCA was associated with lower 30-day and 1-year mortality when compared to no therapy or thrombolysis among elderly patients with acute MI.
The only caveat to the successes of primary PTCA in elderly patients was seen in a trial of patients with very-high-risk MI whose course was complicated by cardiogenic shock (i.e., hypotension and signs of poor tissue perfusion). In one trial, those randomized to primary PTCA had significantly higher survival rates; however, this effect was age dependent, and those >75 years had actually had much higher mortality risk with PTCA.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree