| Conjunctivitis | Keratitis | ||||||
|---|---|---|---|---|---|---|---|
| Bacterial | Viral | Allergic | Bacterial | Viral | Iritis | Glaucoma (acute) | |
| Blurred vision | 0 | 0 | 0 | +++ | 0 to ++ | + to ++ | ++ to +++ |
| Pain | 0 | 0 | 0 | ++ | 0 to + | ++ | ++ to +++ |
| Photophobia | 0 | 0 | 0 | ++ | ++ | +++ | + to ++ |
| Discharge | Purulent + to +++ | Watery + to ++ | White, ropy + | Purulent +++ | Watery + | 0 | 0 |
| Injection | +++ | ++ | + | +++ | + | 0 to + (limbal) | + to ++ (limbal) |
| Corneal haze | 0 | 0 | 0 | +++ | + to ++ | 0 | + to +++ |
| Ciliary flush | 0 | 0 | 0 | +++ | + | +++ to +++ | + to ++ |
| Pupil | Normal | Normal | Normal | Normal or miotic (iritis) | Normal | Miotic | Mid-dilated Nonreactive |
| Pressure | Normal | Normal | Normal | Normal | Normal | Normal, low or high | High |
| Preauricular nodes | Rare | Usual | 0 | 0 | 0 | 0 | 0 |
| Smear | Bacteria PMNs | Lymphs | Eosinophil | Bacteria PMNs | 0 | 0 | 0 |
| Therapy | Antibiotics | Nonspecific | Nonspecific | Antibiotics | Antivirals (if herpes) | Cycloplegia Topical steroids | Medical or surgical |
+, Mild; ++, moderate; +++, severe; PMNs, polymorphonucleocytes.
Etiology
Numerous studies have demonstrated that, regardless of the etiology, acute conjunctivitis follows a benign course and results in few sequelae even without specific antibiotic therapy. Because characteristic signs and symptoms can distinguish bacterial and viral syndromes, the diagnosis of conjunctivitis is based largely on clinical history and examination. Cultures are normally reserved for neonatal or hyperacute conjunctivitis or in patients with a course greater than 2 to 3 weeks, classified as chronic conjunctivitis. A history of contact with other patients with conjunctivitis, bilateral involvement, or exposure to groups of children is associated with the more contagious viral agents. Signs of preauricular lymph node swelling (with the exception of hyperacute or chlamydial conjunctivitis), a follicular palpebral conjunctival reaction, and clear discharge or copious tearing are also more consistent with acute viral conjunctivitis. A papillary conjunctival reaction, mucopurulent discharge, and the lack of local lymph node swelling is more suggestive of bacterial conjunctivitis. When indicated, diagnostic workup consists of conjunctival swabs for Gram and other histologic stains as well as culture.
Viral conjunctivitis
Acute conjunctivitis, defined as less than 2 to 3 weeks duration, is most commonly viral, especially in adults. Adenovirus is a commonly identified pathogen in outbreaks of acute viral conjunctivitis. Although usually associated with types 8 and 19, epidemic keratoconjunctivitis (EKC) has been associated with several other serotypes and is highly contagious, spread by direct contact from hand to eye. In addition to the classic signs of viral conjunctivitis, patients with EKC may develop an immune keratitis consisting of corneal subepithelial infiltrates approximately 2 or 3 weeks after the onset of the conjunctivitis. The corneal inflammation results in complaints of foreign-body sensation, photophobia, and, possibly, decreased vision sometimes lasting days to months. Pharyngoconjunctivitis has a similar ocular presentation but is associated with serotypes 3 and 7 and includes fever and pharyngitis. Viral cultures are reserved for tracking large outbreaks because results usually are available after symptoms have subsided. The recent introduction of an in-office, rapid, reproducible adenovirus antigen screening test should prove to be of more clinical utility. The virus may remain viable on surfaces for many days to weeks, making control of outbreaks problematic. True EKC may remain highly transmissible from patient to patient for 2 weeks or more, and, therefore, requires strict hygiene instruction as well as isolation precautions, especially during the phase of copious discharge. Acute hemorrhagic conjunctivitis associated with enterovirus 70 and Coxsackievirus A24 is a highly transmissible follicular conjunctivitis with preauricular adenopathy with the added feature of subconjunctival hemorrhages (Figure 11.1). Currently available topical antivirals are not efficacious in any of these entities, making primary treatment supportive with topical lubricants, cool compresses, and topical nonsteroidal anti-inflammatory drugs (NSAIDs). Topical corticosteroids have been used cautiously in patients with debilitating symptoms of EKC-related keratitis, but their use is controversial.
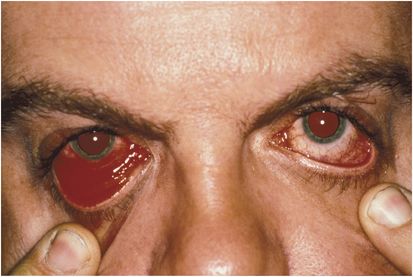
Figure 11.1 Self-limited acute hemorrhagic conjunctivitis.
Either herpes simplex type 1 or 2 may result in a primary follicular conjunctivitis seen in children and young adults. Primary conjunctivitis is normally unilateral with a palpable preauricular lymph node associated with a classic vesicular eyelid or periorbital eruption (Figure 11.2). Systemic antivirals are indicated for primary infection. Because vision-threatening sequelae are associated with corneal involvement, topical trifluridine 1% five to nine times per day or topical ganciclovir five times per day may also be added to either treat or reduce the risk of herpes simplex virus (HSV) keratitis by shortening the duration of the HSV conjunctivitis. Recurrence is common.

Figure 11.2 Primary herpes simplex blepharitis and conjunctivitis.
Chronic viral conjunctivitis may be associated with molluscum contagiosum, usually seen in children. The chronic follicular conjunctivitis is caused by viral shedding into the eye from an eyelid or periorbital molluscum, characteristically a pearly white nodule with an umbilicated center (Figure 11.3). These lesions are typically small and multiple and spread by direct contact. Immunocompromised individuals may present with much larger lesions. Treatment of the molluscum lesion by incision and curettage of its center or excision is curative of the associated conjunctivitis.
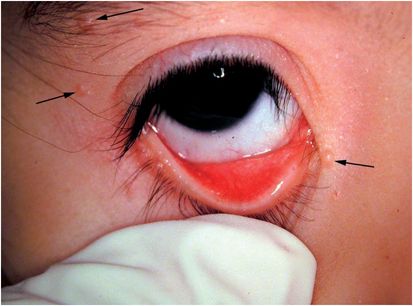
Figure 11.3 Molluscum contagiosum chronic follicular conjunctivitis.
Bacterial conjunctivitis
Most bacterial conjunctivitides are self-limited, have low morbidity, and respond well to most available topical broad-spectrum antibiotics, obviating the need for microbiologic identification. Definitive evaluation and specific treatment is, however, required in hyperacute conjunctivitis, a rapidly progressive, purulent, destructive infection, and neonatal conjunctivitis to avoid local and systemic complications more common to these two entities.
Hyperacute conjunctivitis
Hyperacute conjunctivitis is usually associated with Neisseria species, most commonly Neisseria gonorrhoeae in newborns and young sexually active adults. A copious, rapidly accumulating mucopurulent discharge, intense redness, and periorbital swelling are characteristic of hyperacute conjunctivitis. It is one of the few acute bacterial conjunctivitides that develops a preauricular lymphadenopathy. Rapid corneal and conjunctival penetration can result in severe corneal ulceration and ocular destruction if left untreated. It is considered a true ocular emergency. This potential for ocular complications and systemic infection with N. gonorrhoeae necessitates microbiologic identification as well as systemic antibiotic therapy (see Table 11.2). Local sterile saline lavage can be symptomatically helpful. Because of a significant incidence of coinfection, systemic therapy directed against Chlamydia
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree





