Comprehensive Care of the Cancer Patient with Pain
Comprehensive cancer care encompasses a continuum that progresses from disease-oriented, curative, life-prolonging treatment through symptom-oriented, supportive, and palliative care extending to terminal hospice care. This continuum requires that care is both of high quality and comprehensive in nature. Elements of highquality care include the use of evidence-based treatment, where evidence is gained from high-quality clinical trials; doing what is done often and, hopefully, done well; recognizing the need to treat the whole patient and not just the disease; and treating the patient with compassion. Comprehensive care implies coordinated, integrated care that involves providers and patients working together to address each of the varied issues that impact the cancer patient and family.
Traditional cancer care systems have frequently not offered cancer patients a prospective and comprehensive plan for treatment and symptom management, with provisions for updating and evaluating such a plan with the assistance of a health care professional, and a follow-up plan for monitoring and treating possible late effects of cancer and its treatment. Cancer survivors commonly experience the underdiagnosis and undertreatment of the symptoms of cancer, a problem that begins at the time of diagnosis and often becomes more severe at the end of life. The failure to treat the symptoms, side effects, and late effects of cancer and its treatment has a serious adverse impact on the health, well-being, and the quality of life of cancer survivors. Patients with cancer are sometimes put in the untenable position of choosing between potentially curative therapies and palliative care instead of being assured access to comprehensive care that includes appropriate treatment and symptom management.
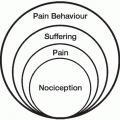
Comprehensive cancer care should incorporate access to psychosocial services and management of the symptoms of cancer (and the symptoms of its treatment), including pain, nausea and vomiting, fatigue, and depression. Pain management is, and should be, an integral component of comprehensive cancer care.1 Designing an effective pain control strategy for the individual patient requires knowledge of the ways in which a patient’s cancer, cancer therapy, and pain therapy can interact. Collaboration with different health care providers (such as medical oncologists and radiation oncologists) is essential to successful pain management. The National Cancer Institute (NCI)-designated cancer centers are characterized by scientific excellence and the capability to integrate a diversity of research approaches to focus on cancer. Many organizations that are dedicated exclusively to health care designate themselves comprehensive cancer centers based on their self-assessment of their prevention, diagnostic, and treatment services. However, the term “comprehensive” as used by the NCI requires more than state-of-the-art care and services and includes a strong research base interactive with a wide spectrum of prevention, care, education, information and dissemination activities that broadly serve communities and regions of the country. From a pure clinical perspective, the goals of patient care in oncology are often complex, but they broadly comprise prolonged survival, as well as optimizing comfort and function. Adoption of these goals logically leads to a multimodality treatment approach targeted to specific problems (Fig. 14.1).
Treatment of the whole patient requires that the clinician not only attempts to treat the tumor and to increase survival, but also relieves the side effects of both the cancer and the treatment, and improves quality of life.2




Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree