15 Complications of Surgery
Craniotomy for resection of intrinsic brain tumors is performed to provide a histological diagnosis, ameliorate neurologic symptoms, and help improve survival. Several studies have suggested a favorable association between cytoreductive surgery and survival in patients with low-grade astrocytoma, malignant glioma, and single brain metastasis.1–4 During the same time period, there has been a significant evolution in the surgical management of these tumors, including the routine use of preoperative functional imaging, stereotactic navigation, cortical mapping, and intraoperative magnetic resonance imaging (MRI), all of which have improved our ability to localize and radically remove intrinsic brain tumors. For these reasons, there has been a renewed interest in understanding the risks of cytoreductive surgery to select appropriate candidates for aggressive tumor resection and to properly counsel patients regarding the expected outcomes of surgery. This chapter focuses on the complications associated with craniotomy for resection of intrinsic brain tumors (e.g., glioma, metastasis), with particular emphasis on the avoidance of these adverse events.
 Defining a Complication
Defining a Complication
There is significant disagreement regarding what constitutes a complication. Everyone recognizes that an outcome must be unwanted to be considered a complication of surgery. Whether a particular event is undesirable may be different for the surgeon, patient, and patient’s family. For example, a frontalis paresis developing after frontotemporal craniotomy would be considered an undesirable outcome by most neurosurgeons, whereas this deficit may go unnoticed by the patient. Another essential feature of a surgical complication is the unexpected nature of the outcome; in other words, the complication does not occur commonly. Most surgical procedures have a range of anticipated outcomes, and complications are those outcomes that deviate from this norm. However, classification of surgical outcomes is subjective. For example, a patient undergoing removal of a glioma located within the dominant supplementary motor area often experiences predictable postoperative neurologic deficits like hemiparesis that improve with time and rehabilitation. Should this be considered an expected, though undesirable, outcome of surgery or a neurologic complication? There is little consensus on this issue, although most surgical series document all adverse events without regard to whether they are expected.5–9 In practice, however, the neurosurgeon must undertake careful discussions with the patient and family regarding expected, though undesirable, outcomes lest these be viewed as complications.
Controversy
• If a patient develops an expected neurologic deficit after surgery, should it be classified as a complication? Does it make a difference whether it is transient or permanent?
Special Consideration
• The neurosurgeon must have an intimate knowledge of the complications and risk factors associated with craniotomy to counsel a patient regarding the optimal surgical option.
Classification of Complications
Various schemes have been introduced to classify surgical complications, and there is considerable overlap among them. Some authors view all complications as potentially avoidable and as resulting from three main causes: (1) lack of information (e.g., failure to recognize a preexisting medical condition); (2) incorrect judgment (e.g., suboptimal surgical approach); and (3) incorrect execution (e.g., excessive brain retraction).10 Implicit in this classification system is the concept that complications are generally under the neurosurgeon’s control, which certainly does not apply to most medical complications.
An alternative classification distinguishes among neurologic, regional, and systemic complications and provides a logical framework for discussing complications associated with craniotomy (Table 15.1).7 In this system, neurologic complications are events that directly produce motor, sensory, language, or visual deficits (e.g., edema, vascular injury, hematoma). Regional complications are related either to the wound (e.g., infection, cerebrospinal fluid [CSF] leak) or to the brain (e.g., seizures, hydrocephalus) but are not associated with neurologic deficits. Systemic complications include more generalized medical conditions (e.g., thromboembolism, pneumonia). These main categories can be further subdivided on the basis of the degree of severity. Major complications include events that are permanent, significantly affect quality of life, or require surgical intervention. In contrast, minor complications are transient or permanent events without significant functional impact, and those that resolve without surgery.
Table 15.1 Complications Associated with Craniotomy
| Neurologic | Regional | Systemic |
| Motor or sensory | Seizure | Deep vein thrombosis |
| Deficit | Hydrocephalus | Pulmonary embolus |
| Aphasia/dysphasia | Pneumocephalus | Pneumonia |
| Visual field deficit | Wound infection | Urinary infection |
| Caused by: | Meningitis | Sepsis |
| Direct brain injury | Brain abscess | Myocardial infarction |
| Brain edema | Cerebrospinal fistula | Gastrointestinal bleed |
| Vascular injury | Electrolyte disturbance | |
| Hematoma |
Source: From Wolters Kluwer Health. Sawaya R, Hammoud M, Schoppa D, et al. Neurosurgical outcomes in a modern series of 400 craniotomies for treatment of parenchymal tumors. Neurosurgery 1998;42:1044–1056. Reprinted with permission.
 Surgical Complications and Their Avoidance
Surgical Complications and Their Avoidance
General Considerations
The overall complication rate associated with craniotomy for intrinsic brain tumor ranges from 25 to 35% and includes all adverse events, expected and unexpected, regardless of severity.5–7,9 The complication rate of a particular series depends on the authors’ definition of a complication, the type of study (retrospective versus prospective), and the referral base of the institution. In general, higher complication rates are reported by those at tertiary neurosurgical centers that have prospectively analyzed complications and have included all adverse events, expected and unexpected.7
The key to minimizing complications is to thoroughly understand all potential adverse events associated with the procedure and to formulate a comprehensive plan to prevent their occurrence. The neurosurgeon must have an intimate understanding of the patient’s history, neurologic findings, and diagnostic studies to determine an accurate preoperative diagnosis. The surgical approach must be individualized to each patient, and the neurosurgeon should either be familiar with the steps of the procedure or request the assistance of a colleague. A complete understanding of the operative anatomy, which includes the structural and functional anatomy of the normal brain as well as any variations introduced by the tumor, is essential. The experienced neurosurgeon also mentally rehearses the entire operation and postoperative period to identify potential pitfalls and develop appropriate contingency plans.
Pitfall
• Complication rates among neurosurgical centers may not be directly comparable because of differences in the classification of complications and data collection methods (retrospective versus prospective).
Special Consideration
• The key to complication avoidance is rigorous judgment, careful planning, and meticulous execution.
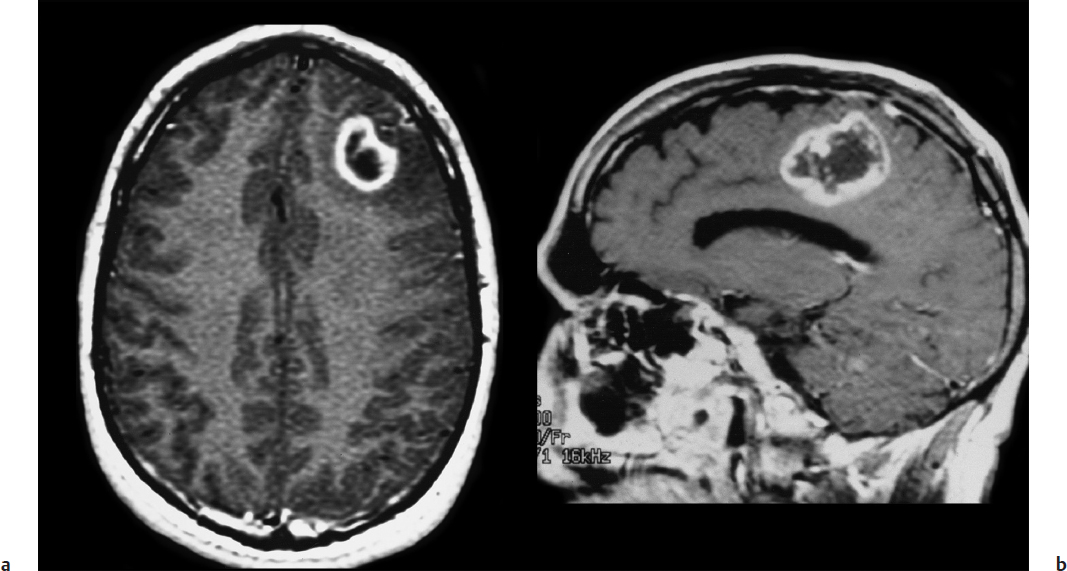
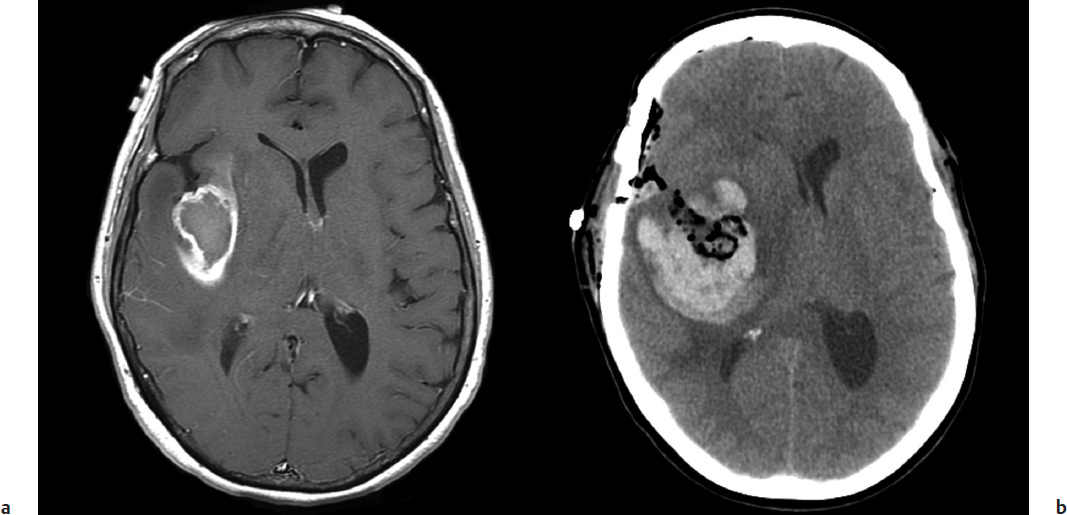
Neurologic Complications
The risk of a new neurologic deficit, minor or major, after craniotomy for intrinsic tumor ranges from 10 to 25% in modern surgical series.5–7,9 Risk factors shown to predict an adverse neurologic outcome include age > 60 years, Karnofsky Performance Scale (KPS) score< 60%, deep tumor location, and tumor proximity to eloquent brain areas.5–8 Despite the concern that aggressive tumor resection might lead to greater neurologic morbidity, two studies have demonstrated the opposite, namely, that gross total resection of intrinsic tumors, particularly malignant glioma, is associated with fewer neurologic complications than is subtotal resection.5,7 This finding is probably explained by the higher risk of postoperative edema and hemorrhage when a glioblastoma is incompletely removed.11 Recognition of the preceding risk factors enables the neurosurgeon to estimate the risk of a neurologic complication for an individual patient.7 In a clinical scenario, a 40-year-old patient with a normal neurologic examination and noneloquent tumor would have a predicted complication rate of about 5% (Fig. 15.1a). In contrast, a 65-year-old patient with a significant hemiparesis caused by a motor area glioblastoma would have a predicted complication rate as high as 26% (Fig. 15.1b).
Special Consideration
• The surgical approach must be individualized to each patient based on factors related to the patient (age, neurologic status, preference) and the tumor (size, location, presumed histology).
Injury to Normal Brain Structures
Neurologic complications result from one of the following etiologies: (1) direct injury to normal brain structures, (2) brain edema, (3) vascular injury, or (4) hematoma. Inadvertent injury to normal brain structures may occur because of incorrect localization of the tumor in relation to adjacent eloquent brain areas. Avoidance of this problem begins with intimate knowledge of the normal structural and functional anatomy of the operative field and the relationship of the tumor borders to adjacent critical brain structures. Functional MRI and diffusion tensor imaging can be used to determine tumor resectability and are powerful tools for surgical planning. For tumors located in the posterior frontal lobe, the motor strip can be identified by cortical mapping techniques and sub-cortical motor pathways preserved during tumor resection.12 Similarly, craniotomy using speech mapping with the patient awake allows the neurosurgeon to maximally resect dominant temporal lobe tumors while minimizing the risk of a postoperative language deficit.12
The introduction of frameless stereotactic techniques has revolutionized the practice of neurosurgery by providing an easy, intuitive, and accurate method for intracranial navigation. Frameless stereotaxis facilitates precise localization of superficial tumors and enables the neurosurgeon to plan optimal trajectories to approach deeply seated tumors, thereby minimizing brain injury associated with dissection. Normal structures like motor cortex can be readily identified and preserved. The information obtained from functional MRI and diffusion tensor imaging can be integrated into the frameless stereotactic system and used intraoperatively to maximize tumor resection while preserving neurologic function.13 The intraoperative feedback provided by stereotactic navigation must, however, be integrated with conventional techniques to assess the extent of resection, including visual inspection, measurement of the tumor cavity, and identification of normal adjacent structures (e.g., falx, skull base, sulci). More recently, intraoperative MRI has proven to be a useful adjunct by providing near real-time updates during the course of tumor surgery to overcome the problem of brain shift and maximize the degree of tumor resection.14,15
Pitfall
• The neurosurgeon should not rely too much on frameless stereotactic navigation to determine the extent of tumor resection because the accuracy of this information decreases when brain shifts occur during surgery. Intraoperative MRI provides near real-time updates that allow the surgeon to compensate for these changes.
Brain Edema
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree