Fig. 10.1
Intraoperative closure after myomectomy with inverted absorbable monofilament suture
Fig. 10.2
Reconstructed uterine wall and enucleated myoma before morcellation and extraction
10.2 Material and Methods
Laparoscopic myomectomy was performed in patients with symptoms such as disturbed menstrual bleeding, pelvic pain, and infertility.
The laparoscopic enucleation of fibroids always followed the same pattern:
1.
Injection of a 0.05 % vasopressin solution in 1–4 locations under the myoma capsule.
2.
Longitudinal incision of the capsule with the aim of enucleating the fibroid under the capsule, leaving the capsule in situ (this can usually be easily peeled like an orange).
3.
Grasping of the fibroid with a myoma screw, traction, and bipolar or ultrasound coagulation of spiral arteries. Coagulation of the myoma pedicle and the myoma is twisted out of its bed.
4.
Rinsing of the myoma bed with Ringer’s lactate and coagulation of larger bleedings.
5.
Adaption of wound edges with several deep sutures to a depth of 5–20 mm without touching the endometrium. Only rarely is a double layer of sutures necessary. Whenever the uterine cavity is opened, it has to be closed with individual sutures.
6.
Morcellation of the fibroid with one of the commercially available morcellators and fibroid extraction.
The hysteroscopic enucleation of a submucous fibroid is performed by filling the uterine cavity with Purisole® and then in a continuous movement slicing the fibroid into pieces (electroresection) and retracting the pieces through the cervix. Bleedings can be controlled by pressure release and coagulation with the roller ball or with the cutting loop.
10.2.1 Questionnaire for Patient Data
A questionnaire was sent to 392 patients with fertility problems who were treated by laparoscopy or hysteroscopy at the Department of Obstetrics and Gynaecology, University Hospitals Schleswig-Holstein, Campus Kiel. One hundred and fifty-four patients (40 %) returned the questionnaire that posed questions concerning myomectomies, endometriosis resection, ovarian cyst enucleation, and adhesiolysis.
Patients were evaluated as follows:
Group A = all patients (n = 392)
Group B = patients who answered the questionnaire (n = 154)
Group C = patients from group B who became pregnant (n = 78)
10.3 Results
Of the 392 patients who underwent laparoscopic surgery for fertility problems in our department in 2008/2009, in 129 cases (32 %) myomas (fibroids) were the indication for surgery. Of these 129 patients, in 56 cases (14.3 %) myomas were the only indication for infertility. In 44 cases (11.2 %) myomas appeared together with another disease: in 20 cases (5.1 %) with other genital abnormalities, in 18 cases (4.6 %) with tubal pathology, in 3 cases (0.8 %) with endometriosis, and in 3 cases (0.8 %) with ovarian cysts. The combined appearance of myomas with more than one other genital disturbance was found in 29 patients (7.5 %).
10.3.1 Frequency of the Different Myoma Localizations
Figures 10.3, 10.4, and 10.5 show the frequency of myomas within the whole evaluation. Multiple sites often occurred and this resulted in a higher incidence (n = 140). The location of fibroids were evaluated as diffuse (within the uterine wall), submucous, intramural, subserous, and submucous as well as at multiple locations. Primarily a deep, diffuse myomatosis was found in 60 % of patients in group A, in 62 % of patients in group B, and in 59 % of patients in group C. Submucous fibroids occupied second position in group A (16 %) and subserous fibroids occupied second position in group B (19 %) and group C (21 %). Third position was occupied by subserous fibroids in group A (13 %) and by submucous fibroids in group B (12 %) and group C (14 %). In all three groups, intramural fibroids were the most rarely found: group A (11 %), group B (8 %), and group C (7 %) (Table 10.1).
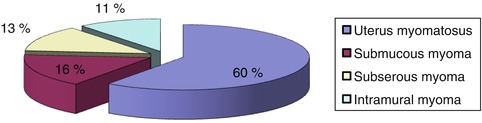
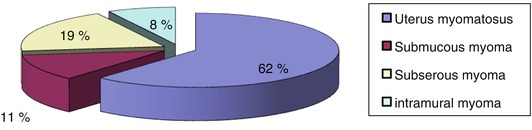
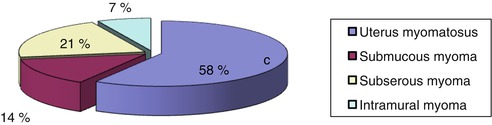
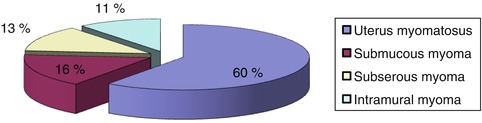
Fig. 10.3
Localization of myomas in the 392 patients (group A)
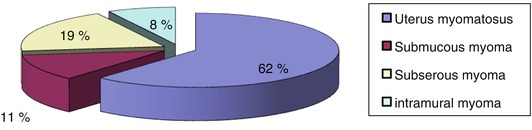
Fig. 10.4
Localization of myomas in the group which answered the questionnaire (group B)
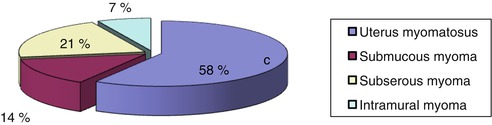
Fig. 10.5
Localization of myomas in the group which became pregnant (group C)
Table 10.1
Frequency of myoma locations in the individual groups, A, B, and C
Location | Group A (all patients) | Group B (patients who answered the questionnaire) | Group C (patients who became pregnant) |
|---|---|---|---|
Combined subserous-intramural | 84 | 32 | 17 |
Submucous | 23 | 6 | 4 |
Subserous | 18 | 10 | 6 |
Intramural | 15 | 4 | 2 |
Total | 140 | 52 | 29 |
10.3.2 Side Effects and Symptoms
The following side effects were observed in descending frequency: bleeding abnormalities (33.3 %), tubal patency, degree 1–2 (23 %), adhesions (22 %), and intramural tubal occlusions (15 %).
In 122 patients a laparoscopic myoma enucleation was performed. In 61 % of patients the myomas were situated subserous-intramural, in 18 % submucous, in 13 % subserous, and in 8 % intramural. In 33 patients adhesiolysis was necessary prior to the myomectomy.
Figure 10.6 shows the procedures performed on the 392 patients who underwent laparoscopic surgery for infertility in 2008/2009.
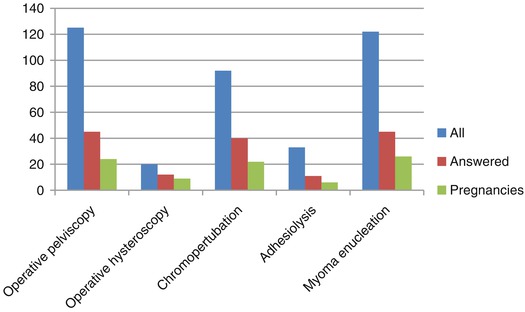
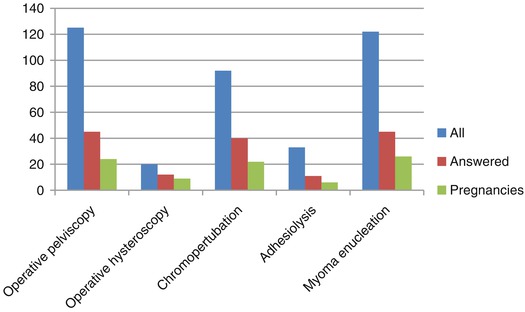
Fig. 10.6
Laparoscopic surgical procedures performed for infertility according to groups A, B, and C
10.3.3 Additional Previous Therapy for Fibroids
Figure 10.7 shows clearly that pregnancy rates increased after pretreatment and surgery.
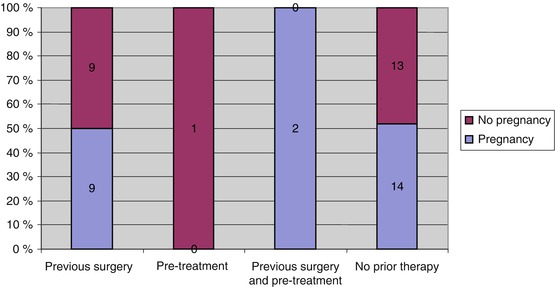
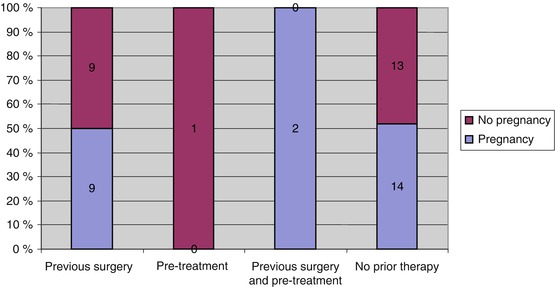
Fig. 10.7
Influence of surgery and pretreatment on pregnancy rates of patients with myomas
10.3.4 Pregnancies and Deliveries
The average age of the evaluated patients was 34.6 years. Different pregnancy rates resulted depending on the localization of the fibroids. The lowest pregnancy rate was achieved after intramural fibroid resection. The resection of intramural-subserous fibroids resulted in a good pregnancy and delivery rate, and the highest pregnancy rate was achieved after submucous fibroid resection (Figs. 10.8 and 10.9).
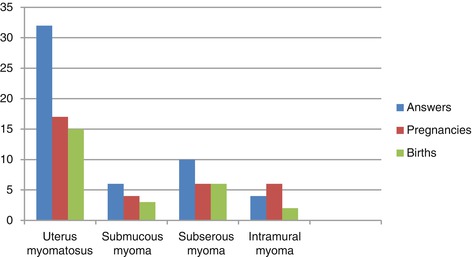
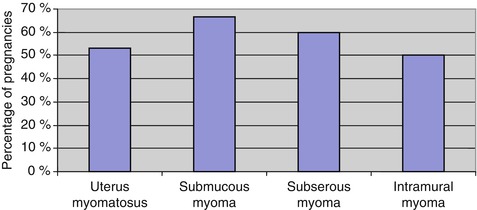
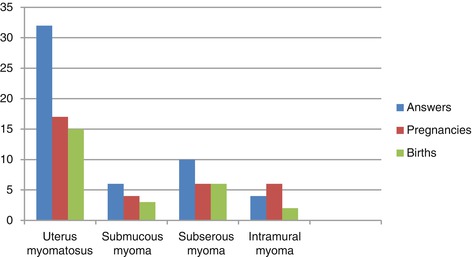
Fig. 10.8
Number of pregnancies and deliveries according to localization of myoma with display of answers
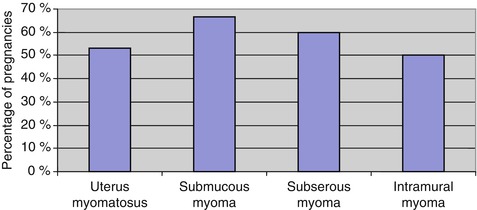
Fig. 10.9
Number of pregnancies according to myoma localization
10.3.5 Mode of Delivery
Eleven of the 129 myomectomy patients underwent a cesarean section. Of these 129 patients, only 25 suffered from myomas alone; all others had multiple morbidities. The 14 pregnancies (56 %) which resulted in this group of 25 led to 12 deliveries (48 %), 5 (42 %) of which were spontaneous and 7 (58 %) cesarean sections. In the group of patients who underwent myomectomy for fertility problems, we had a pregnancy rate of 53 % (n = 17) and a delivery rate of 47 % (n = 15).
10.3.6 Complications
Four complications occurred in the group of myomectomy patients at or after delivery: bladder descensus after delivery, placenta accrete, one uterine rupture, and one emergency cesarean section due to imminent asphyxia of the baby.
10.4 Discussion
Recent advances in endoscopic surgical techniques and the increased sophistication of surgical instruments have offered new operative methods and techniques for the gynecologic surgeon [10]. Recent years have witnessed a marked increase in the number of gynecological endoscopic procedures performed, mainly as a result of technological improvements in instrumentation. Laparoscopy has become an integral part of gynecologic surgery for the diagnosis and treatment of abdominal and pelvic disorders of the female reproductive organs. Endoscopic reproductive surgery intended to improve fertility may include surgery on the uterus, ovaries, pelvic peritoneum, and fallopian tubes.
10.4.1 Laparoscopic Myomectomy and Pregnancy Outcome
Uterine leiomyomas are the most common benign tumors of the female reproductive tract and affect 30–40 % of reproductive-age women. Although they are seldom the sole cause of infertility, myomas have been linked to fetal wastage and premature delivery. Several elements indicate that myomas are responsible for infertility. For example, the pregnancy rate is lower in patients with myomas, and in cases of medically assisted procreation, the implantation rate is lower in patients presenting with interstitial myomas. There is other indirect evidence supporting a negative impact, including lengthy infertility before surgery (unexplained by other factors) and rapid conception after myomectomy [11]. Approximately 50 % of women who have not previously conceived become pregnant after myomectomy [12]. Because medically treated fibroids tend to grow back or recur, most fibroids that cause symptoms are managed surgically (Table 10.2).
Table 10.2




Treatment modalities for uterine leiomyomas
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree