| Species | Reservoir | Vector | Human disease |
|---|---|---|---|
| B. henselae | Cat, dog, raccoon | Cat flea (Ctenocephalides felis), other? | CSD, retinitis, IE, myocarditis, encephalopathy, aseptic meningitis, myelitis, neuropathy, osteomyelitis, BAP, glomerulonephritis, purpura, pseudomalignancy, prolonged asymptomatic bacteremia |
| B. quintana | Rat, human? | Louse | CSD, IE, trench fever, encephalopathy, BAP, osteomyelitis, prolonged asymptomatic bacteremia |
| B. vinsonii subsp. berkhoffii | Coyote, dog | Unknown | IE |
| B. vinsonii subsp. arupensis | White-footed mouse | Unknown | IE, neurologic disorders |
| B. koehlerae | Cat, raccoon | Flea, C. felis | IE |
| B. elizabethae | Rat | Oriental rat flea Xenopsylla cheopsis | IE |
| B. washoensis | California ground squirrel (Spermophilus beecheyi) | Unknown | Fever, myocarditis |
| B. alsatica | Rabbit | Unknown | IE |
| B. grahamii | Wild mice | Unknown | Neuroretinitis |
| B. clarridgeiae | Cat, raccoon | Flea, C. felis | Possible CSD |
Abbreviations: CSD = cat scratch disease; IE = infective endocarditis; BAP = bacillary angiomatosis and parenchymal bacillary peliosis.
The clinical spectrum of CSD in the immunocompetent host includes classic CSD as well as ophthalmologic, neurological, cardiovascular, parenchymal, musculoskeletal, and immune complex–mediated syndromes such as glomerulonephritis; as well as prolonged fever without adenopathy or focal lesions. Parenchymal masses associated with CSD have been mistaken for malignancies such as breast cancer or lymphoma.
In hosts with compromised cell-mediated immunity, including patients with acquired immunodeficiency syndrome (AIDS), solid organ transplant recipients, and patients with hematologic malignancies, B. henselae and B. quintana cause vascular tumors called bacillary angiomas (BA) and blood-filled cavities of liver and spleen, termed bacillary peliosis hepatis; these lesions are referred to collectively as “BAP.”
Classic cat scratch disease
CSD is the most common cause of regional lymphadenitis in children and young adults. Approximately 24 000 cases occur each year with a prevalence of roughly 9.3/10 000 ambulatory patients per year and a seroprevalence ranging from 3% to 6%. CSD tends to occur in late summer or fall and to vary in frequency with the geographic distribution of the cat flea, Ctenocephalides felis.
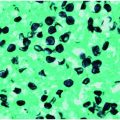
The first clinical manifestations of CSD appear 5 to 7 days after the scratch or bite from an infected cat, kitten, or cat flea, with the appearance of a small erythematous nodule at the site of bacterial entry. Although this inoculation papule may go unnoticed, it is said to be present in 70% of CSD cases. This nodule represents the initial host response to bartonella and is characterized by palisading macrophages, acute and chronic inflammatory cell infiltration, as well as activation and invasion of vascular endothelial cells. Painful swelling of the proximal lymph nodes follows the appearance of the inoculation papule by 7 to 14 days and may be accompanied by constitutional symptoms and fever. The histopathology of the lymph node is highly characteristic of CSD, involving both acute and chronic inflammatory cells and the presence of microabscesses that are described as “stellate.” Aggregates of small coccobacilli may be identified in these abscesses using either silver impregnation stains such as Warthin–Starry and Steiner stains or by immunofluorescent staining with commercially available monoclonal antibodies specific for B. henselae or B. quintana. The clinical diagnosis of classic CSD can also be confirmed by PCR of tissue or the demonstration of elevated immunoglobulin G (IgG) and IgM antibodies to B. henselae or B. quintana. Classic CSD usually resolves over several weeks to months without treatment. Although one prospective randomized controlled trial indicated that a 5-day course of azithromycin might hasten the resolution of lymph node swelling, most experts do not recommend antimicrobial therapy for mild to moderately severe CSD. Where lymph nodes become fluctuant and painful, needle aspiration may be all that is required to relieve discomfort and hasten resolution. The syndrome of classic CSD in immunocompetent hosts is thought to be due to an exuberant host response to relatively few organisms, which is one possible explanation for the relatively minor impact of antimicrobials in this setting (Table 127.2).
| Clinical presentation | Adult treatment recommendations |
|---|---|
| Mild to moderate classic CSD | No antimicrobials recommended |
| Severe CSD with large painful lymphadenopathy | Azithromycin, 500 mg PO, d 1, 250 mg d 2–5, aspiration if fluctuant |
| Retinitis | Doxycyclinea, 100 mg PO BID for 4–6 wk, + rifampin, 300 mg PO BID for 4–6 wk; consider topical corticosteroids |
| Encephalopathy | Doxycyclinea, 100 mg PO or IV for 6 wk, + rifampin, 300 mg PO BID for 4–6 wk; duration is not a matter of consensus at this time |
| Suspected Bartonella BCNE | Gentamicin, 3 mg/kg/d × 14 d, + ceftriaxone, 2 g/d IV or IM × 6 wk |
| Confirmed Bartonella BCNE | Gentamicin, 3 mg/kg/d IV × 14 d, + doxycyclinea, 100 mg BID × 6 wk |
| Trench fever, prolonged B. quintana bacteremia | Gentamicin, 3 mg/kg/d IV × 14 d, + doxycyclinea, 200 mg/d PO × 4 wk |
| BA | Erythromycin, 500 mg PO QID × 3 mo, or doxycycline, PO QID 100 mg BID × 3 mo |
| PH | Erythromycin, 500 mg PO QID × 4 mo, or doxycyclinea, PO QID 100 mg BID × 4 mo |
a Substitution of minocycline for doxycycline has not been addressed in published reports.
Abbreviations: CSD = cat scratch disease; BCNE = culture-negative infectious endocarditis; BA = bacillary angioma; PH = peliosis hepatitis.
Ophthalmologic CSD
Approximately 3% of CSD patients develop ocular pathology. These manifestations may be unilateral or bilateral and include conjunctivitis, retinitis, choroiditis, iridocyclitis, endophthalmitis, or orbital abscess with osteomyelitis.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree