CALCIUM BALANCE DURING PREGNANCY
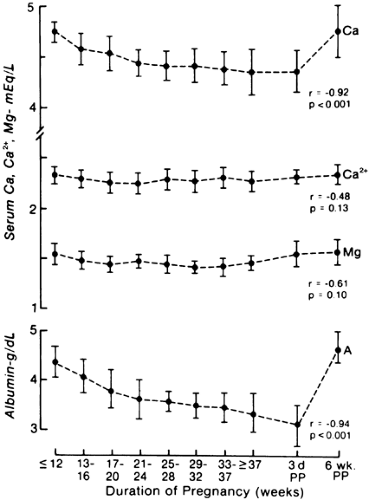
Twenty-five to 30 g of calcium is transferred from the mother to the fetus during gestation; ˜300 mg per day is transferred in the third trimester.88 A net loss of calcium into the urine also occurs because of the increased glomerular filtration that is associated with pregnancy.89 Serum total calcium levels decrease modestly from 2.4 mmol/L to 2.2 mmol/L, in parallel with a fall in serum albumin levels from 4.7 to 3.2 g/dL. Ionized calcium levels remain unchanged88,89 and 90 (Fig. 110-4).
The primary adaptational event to counter this negative calcium balance is an increase in circulating 1,25-dihydroxy-vitamin D levels; this results in increased intestinal absorption of calcium.91,92 Although this augmented formation of 1,25-dihydroxyvitamin D has been thought to result from increases in parathyroid hormone, serum levels have been reported to be low, normal, and high,88,89,90,91 and 92 probably because of differences in the detection of parathyroid hormone cleavage products.91,92 Women who have poor calcium intake during gestation probably develop significant negative calcium balance despite these adaptive changes; thus, an intake of at least 1200 to 1600 mg per day has been recommended.93
Serum calcium levels in the fetus are greater than those in the mother, suggesting active transport of calcium across the placenta.88,89 The fetal hypercalcemia suppresses the fetal parathyroids, so that the neonate is relatively hypoparathyroid at birth.88,89 The elevated calcium levels present in cord blood fall to a nadir at 24 to 48 hours of age. In the absence of confounding factors such as maternal diabetes mellitus, preterm birth, or birth hypoxia, the parathyroid glands in the neonate generally recover quickly88,89 (see Chap. 49).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree