Chapter 25
Burns
Helen McCarthy
Introduction
It has been estimated that approximately 250 000 people suffer from a burns injury each year in the UK with only a small number being admitted to hospital [1, 2]. The 2008 International Burn Injury Database (iBID) report estimated that 18 600 (44%) of those admitted to hospital are children with the majority (75%) being under the age of 5 years [3]. These figures have generally remained unchanged over the past 10 years.
Assessment of injury
Thermal injury can be classified in a number of ways but include contact, flame, electrical and chemical burns as well as scalds [4]. The main causes and types of thermal injury in children and adolescents are listed in Table 25.1. The most common injury reported in children is a scald (61%) with contact burns accounting for 21% and 8% of injury being as a result of a flame burn [3].
Table 25.1 Causes and types of burn injury
| Type of burn | Cause of burn |
| Water | Kettle, teapot, cup, mug, bath, saucepan |
| Contact | Radiator, iron, oven, hot water bottle |
| Flame | House fire, chip pan, electric/coal fire, barbecue |
| Fat | Chip pan, oven trays |
| Chemical | Cement, hair dye, cleansing agents, cytotoxic drugs |
| Electrical | Electrical appliances, overhead and underground cables |
| Other | Overexposure to radiotherapy, frostbite, animal manure |
It is well documented that the size and depth of a thermal injury has a direct impact on morbidity and mortality [5, 6]. Burns are dynamic injuries that are rarely uniform in depth and therefore require continual reassessment [4, 7].
Burn depth is generally classified as partial or full thickness. Partial thickness injuries are further subdivided into superficial, where only the epidermis is affected; superficial dermal, where the injury extends through the epidermis into the dermis and blistering is observed; deep dermal where the injury extends through the dermis but does not infiltrate the subcutaneous tissue [7].
Burn size relates to the surface area affected by the injury. There are a number of ways to assess burn size. The simplest method is the ‘palmar surface’, which is based on the palm of the patient’s hand (including fingers) being approximately 0.8% of the total body surface area (TBSA) [7]. This method works well with small injuries but with increasing wound size becomes less so. In adults the Wallace ‘rule of nines’ is commonly used, and this has been adapted for children (Table 25.2) [7]. The most common method for determining burn size in children is using the Lund and Browder charts which have been reproduced in many formats since originally proposed in 1944 [7–10].
Table 25.2 Methods of quantifying burn surface area
| Wallace ‘rule of nines’ | Lund and Browder | |||||||
| Adult | Child | < 1 year | 1 year | 5 years | 10 years | 15 years | Adult | |
| Head (front and back) | 18% | 9% | 19% | 17% | 13% | 11% | 9% | 7% |
| Neck (front and back) | 2% | 2% | 2% | 2% | 2% | 2% | ||
| Chest/trunk (front) | 18% | 18% | 13% | 13% | 13% | 13% | 13% | 13% |
| Back/trunk (back) | 18% | 18% | 13% | 13% | 13% | 13% | 13% | 13% |
| Arm (front and back) | 9% | 9% | ||||||
| Upper arm (front and back) | 4% | 4% | 4% | 4% | 4% | 4% | ||
| Lower arm (front and back) | 3% | 3% | 3% | 3% | 3% | 3% | ||
| Hand (front and back) | 3% | 3% | 3% | 3% | 3% | 3% | ||
| Perineum | 1% | 1% | ||||||
| Genitalia | 1% | 1% | 1% | 1% | 1% | 1% | ||
| Buttocks (both) | 5% | 5% | 5% | 5% | 5% | 5% | ||
| Leg (each) | 18% | 13.5% | ||||||
| Thigh (front and back) | 5.5% | 6.5% | 8% | 9% | 9% | 9.5% | ||
| Lower leg (front and back) | 5% | 5% | 5.5% | 6% | 6.5% | 7% | ||
| Foot (top and bottom) | 3.5% | 3.5% | 3.5% | 3.5% | 3.5% | 3.5% | ||
Adapted from Hettiaratchy and Papini [7].
The severity of an injury combines the depth, size and other factors. In children the types of burn are
- a major burn, defined as a full thickness burn covering an area of >10% TBSA
- a partial thickness burn of >20% TBSA
- burn injuries to the eyes, ears, face, hands or feet or other areas that are likely to result in functional impairment
- burns complicated by another major trauma or inhalation injury [6]
Metabolic response to burn injury
Thermal injury results in a marked change in metabolism that is reported to last up to 12 months or longer depending on the severity of the original injury [11–14]. Initially there is a reduction in metabolic rate that lasts 3–5 days. This is the ‘ebb phase’. During this period there is evidence that the requirements of the child fall below the estimated average requirements (EAR) for age [15]. This is then followed by the hypermetabolic ‘flow phase’ which is associated with physiological, endocrine and immunological changes [11–14, 16, 17]. The exact cause of the hypermetabolic response remains poorly defined; however, catecholamines, corticosteroids and inflammatory cytokines are primary mediators with raised levels being observed for an extended period post injury [16].
Modern medical and nursing management has had the effect of moderating the hypermetabolic response to the burns injury [12, 16]. These include early excision and grafting; increased use of artificial skin and other novel wound coverings; regular analgesia; control of ambient temperature; and nutritional intervention [17–19]. Nonetheless the metabolic response remains elevated and evidence clearly links this to the extent of the injury, and in children their age and gender [20–22].
Aim of nutritional support
The aim of nutritional support in a child with a thermal injury is to provide appropriate intervention in order to moderate the hypermetabolic response, promote optimal wound healing and maintain normal growth. It is well documented that improved nutritional status in the critically ill patient reduces the likelihood of complications (e.g. infection, poor wound healing) and length of stay in hospital [23–25].
Nutritional requirements
Factors influencing the nutritional requirements of a child with a thermal injury are listed in Table 25.3. A full assessment of nutritional requirements should be made taking these and any additional factors, such as surface area used as donor sites for skin grafts, into consideration.
Table 25.3 Factors influencing nutritional requirements
| Age |
| Sex |
| Weight |
| Height/length |
| Pre injury nutritional status |
| Current nutritional status |
| Percentage burn surface area |
| Thickness of burn |
| Grafted area |
| Extent of healing |
| Comorbidities |
Energy requirements
Several researchers have investigated energy requirements in children with thermal injuries. Although the gold standard method for estimating energy requirements would be to measure them daily using indirect calorimetry and adjusting all nutritional support to meet these figures, this is often impractical. Calculations have been proposed to estimate energy requirements and, while these are commonly used in clinical practice, there is some evidence to suggest their accuracy is limited [26, 27].
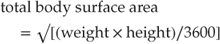
Energy requirements in children with burns rarely rise above the EAR in the first 24 hours post burn injury [15, 28]. Therefore it may be reasonable to aim for the EAR for age initially for all injuries, particularly those classified as minor or of a small surface area. Commonly used formulas for estimating energy requirement for children are detailed in Table 25.4. These include the Curreri Junior formula and the Galveston or Hildreth formula [29–33]. These formulas require an estimate of body surface area and burn surface area. There are a number of equations to aid with this estimation, but the simplest is probably the Mosteller formula [34]:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






