Collection site
Comments
Abscesses, subcutaneous sites
Aspirate abscess; sample base of subcutaneous lesions
Blood
Use maximum amount of blood recommended for the system being used
Bone marrow
Pediatric Isolator™ recommendedb
CSF
Do not refrigerate
Draining sinus tracts
Search for granules of eumycotic mycetoma; wash several times with saline containing antibiotics
Ear
Rotate swab firmly in outer ear
Eye
Inoculate corneal scrapings directly onto plates in a “C” shape
Hair
Use forceps to collect several hairs with shaft intact and sample any active lesions
Intravenous catheters
Use Maki (“roll”) method
Lower respiratory
Process promptly for dimorphic pathogens (BAL, brush, aspirate, wash, sputum)
Medical devices (valves, hardware, etc.)
Dislodge any biofilms before inoculation into liquid medium
Nails
For dermatophytes, agents of dermatomycoses, and Candida spp.; clean with 70 % alcohol; collect subungual debris and clip affected nails
Nasal sinus
Surgical collection, commonly ethmoid and maxillary sinuses
Open wound
Aspirate or swab vigorously
Prostatic fluid
Primarily for blastomycosis
Skin
For dermatophytes; clean with 70 % alcohol and scrape vigorously
Sterile body fluids
May be concentrated by centrifugation or syringe filtration
Tissue
Surgical collection; use punch biopsies for skin lesions
Urine
Early morning midstream collection
Vagina
Primarily for refractory vaginal candidiasis
Vitreous fluid
Needle aspiration
Upper respiratory (oral)
Swab lesions, use selective media for yeasts
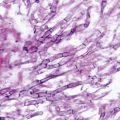
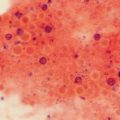
Prior to receipt in the mycology laboratory, a portion of all tissue samples submitted for culture should also be placed in formalin for submission to the histology laboratory. Histopathologic examination together with appropriate stains are usually necessary to document fungal invasion. These may include the routine hematoxylin and eosin (H&E) stain, Gomori methenamine silver (GMS) stain, periodic acid–Schiff (PAS) stain, and others. Discussion of the use of histopathology and of mycological stains is found in Chap. 4 of this book. See also Appendix C of the CLSI M54-A document [5]. As a part of routine processing, the mycology laboratory should also examine a portion of the specimen directly by microscopy, typically with the use of a potassium hydroxide (KOH) preparation, gram stain, calcofluor white fluorescent stain, India ink stain (limited to cerebrospinal fluid examination for Cryptococcus neoformans), or some other method (Table 2.2). Observation of fungal structures by direct microscopy and/or histopathology is essential to corroborate organism recovery in culture (rule out contamination). Table 9.4 in Sect. 9.1.1 of the CLSI M54-A document [5] provides a useful listing/description of yeasts and yeast-like fungi seen in clinical specimens.
Table 2.2
Useful direct microscopy methods for the routine mycology laboratorya
Method | Comments |
|---|---|
Calcofluor white | Requires fluorescence microscope; can be used with KOH to detect all fungi, including Pneumocystis |
Gram stain | Detects most fungi, which are present; however, Cryptococcus spp. may exhibit only faint staining |
Giemsa stain | Several modifications; detects intracellular H. capsulatum and intracystic bodies and trophozoites of Pneumocystis |
India ink stain | Commonly used from demonstration of capsular material of Cryptococcus neoformans in CSF |
Potassium hydroxide | Clears debris so fungi are more readily observed; stains may be added for better visualization of fungal elements |
Wright stain | Useful to detect intracellular H. capsulatum in bone marrow and peripheral smears |
The media used for primary isolation may vary according to personal preferences; however, certain basic tenets apply to all media used for primary recovery. Material from nonsterile sites should be cultured on media that will support fungal growth but also inhibit bacteria. Antibacterial agents, alone or in combination, are added for this purpose. Common choices include chloramphenicol (< 16 µg/ml), gentamicin (5–100 µg/ml), penicillin (20 µg/ml), streptomycin (40 µg/ml), and ciprofloxacin (5 µg/ml). These agents should not be included, however, when actinomycetes are suspected. Media may also be made selective by the addition of the eukaryotic protein synthesis inhibitor cycloheximide at 0.5 µg/ml. This may be useful in the detection of dimorphic fungi and dermatophytes; however, many clinically significant saprobic fungi may be suppressed, leading to failure in recovering opportunistic etiologic agents in compromised hosts. Therefore, media with and without this agent should routinely be employed. Enriched media with 5–10 %, sheep erythrocytes may be incorporated into the battery for fastidious thermally dimorphic fungi such as H. capsulatum and Blastomyces dermatitidis. Peptone-based versus plant-based media may also be a consideration. Many of the opportunistic filamentous fungi prefer plant-based media, producing more typical colony morphologies and more diagnostic structures, thus increasing the potential to make identification possible from primary plates. Plant-based media may also be made selective with antibacterial agents or cycloheximide. Table 2.3 lists several commercially available media that may be used for both primary isolation and identification. Please consult Sects. 10.2 and 10.3 in the CLSI M54-A document for additional information [5]. The choice of tubed versus plated media is made based upon space constraints, personal preference, and safety. The greater surface area provided by plates is preferred by many laboratorians (and always preferred by the fungi!), as manipulation of cultures, isolation procedures, etc. are more easily performed on plates. When used, plate lids should be firmly attached with an air-permeable material or plates sealed in air-permeable bags to avoid cross-contamination or laboratory worker exposure.
Table 2.3
Media useful for primary isolation and identificationa
Medium | Uses/Comments |
|---|---|
Sabouraud dextrose agar (SDA) | For yeasts |
Usually adequate for aspergilli | |
Poor color and conidiation for black moulds | |
Classic morphologic descriptions for dermatophytes | |
CHROMagar Candidab | Contains chromogenic substrates and antimicrobial agents; for isolation and identification of yeasts |
Albicans IDc | As above |
Potato dextrose agar (PDA) | Useful for all mould recovery/identification |
Potato flakes agar (PFA) | |
Brain heart infusion (BHI) agar | |
Inhibitory mould agar (IMA) | |
Yeast extract phosphate medium | |
Sabhi agar | |
Mycosel agar™ § or Mycobiotic agar | SDA with chloramphenicol and cycloheximide |
Dermatophyte test medium (DTM) | |
Dermatophyte identification medium (DIM) |
Optimally, cultures should be incubated at 30 °C (± 1 °C). If this temperature is not available, room temperature near 25 °C should be used. Seven-day incubation is generally adequate when screening for yeasts from oropharyngeal or vaginal sites. Although 4-week incubation times have been traditionally recommended, studies suggest that 3 weeks are adequate to detect fungal growth from most other specimens, excluding those from skin, hair, and nails, and in cultures requested specifically to attempt to recover dimorphic pathogens [27]. The time required for development of diagnostic structures, particularly for some coelomycetes and ascomycetes, may be considerably longer, up to several weeks [28, 29].
Examining Cultures
One recommendation for culture examination is every day for the first 3 days and twice a week thereafter. Alternate reading schedules can be found in the CLSI M54-A document, Sect. 11.1 [5], depending upon the source of the isolate. Cultures of yeasts are typically creamy to waxy, while moulds appear velvety to woolly to cottony. Some safety precautions common to both yeasts and moulds include the careful handling of plates and tubes so as not to create aerosols of infectious material and the prevention of contamination of patient cultures with ubiquitous fungi from the work surroundings.
Phenotypic Yeast and Yeastlike Organism Identification
Yeast cultures, consisting of unicellular organism that replicate by budding, may be handled on the open bench, adhering to the same safety precautions as for bacteria. Yeast and yeastlike fungi should be examined for their colony color (white to cream to pink; brownish-black for the yeast synanamorph of Exophiala species when observed on Sabouraud dextrose agar; blue to green to pink for Candida species on CHROMagar Candida™ (CHROMagar Microbiology, Paris, France)), growth rate, temperature requirements (or preferences), macroscopic morphology (smooth, wrinkled, glabrous, moist, dry, etc.), and microscopic morphology (size and shape, presence of blastoconidia, capsules, germ tubes, pseudohyphae, true hyphae, chlamydoconidia, etc.). Yeast morphology is most reliably observed on a cornmeal agar plate using the Dalmau method [30]. This technique involves streaking a very small amount of yeast onto a plate in two parallel lines, streaking back and forth over these lines for better isolation, and covering the area with a flame-sterilized coverslip. The plate is incubated at room temperature for 18–24 h and then examined microscopically for diagnostic structures. Tease mounts may also provide useful information. Additional procedures that may be required for the identification of yeasts include the reduction of nitrate to nitrite, urease activity, the ability of the organism to grow on media containing cycloheximide, and assimilation and fermentation patterns. Many commercial systems, both manual and automated, are available to assist in yeast identification.
Phenotypic Mould Identification
Any filamentous organisms recovered on culture should be examined and manipulated in a biological safety cabinet. While moulds can be recovered on a variety of media, conidiation/sporulation is generally enhanced on plant-based media. If not used in primary isolation, plant-based media should be employed in the identification process. Moulds should be examined for their growth rate, temperature requirements, and macroscopic morphology to include color (hyaline to brightly colored or phaeoid (brownish to blackish)), texture (velvety, woolly, granular, cottony, etc.), and the observation of any diagnostic features visible to the naked eye. The microscopic detail may be studied using tease mounts or temporary tape mounts (clear tape only) in lactophenol cotton blue. The preferred technique to demonstrate diagnostic structures and methods of conidiogenesis for most filamentous fungi is the slide-culture method. Additionally, this method can provide a permanent mount that can be preserved in a slide collection for future studies and is extremely useful for comparison with other similar isolates or atypical strains. Members of the order Mucorales (which includes Rhizopus, Lichtheimia (formerly Absidia), Mucor, and several other genera) may rapidly overgrow slide cultures, making this method less than optimal for studying these fungi.
Slide cultures should also not be set up on Moulds where the clinical history suggests a dimorphic pathogen such as H. capsulatum, B. dermatitidis, Coccidioides species, Paracoccidioides brasiliensis (not commonly seen in the USA), or Talaromyces (Penicillium) marneffei (usually restricted to HIV-infected individuals from endemic areas of Southeast Asia) [31]. Tease mounts should be prepared for these isolates in a mounting fluid known to kill the fungus, such as lactophenol cotton blue. Sporothrix schenckii, and other Sporothrix spp. [32], also dimorphic organisms, pose less of an exposure risk, and may be examined by slide culture. H. capsulatum and B. dermatitidis may be definitively identified using the DNA Gen-Probe® (AccuProbe, San Diego, CA) methodology. This method, which confirms a Coccidioides species, does not, however, differentiate between Coccidioides immitis and Coccidioides posadasii.
Molecular Fungal Identification
While this work contains a chapter on diagnostic molecular biology (Chap. 3), information about fungal identification would be incomplete without brief mention here of the most commonly used molecular method for the identification of clinical isolates. The method most often cited is sequencing with identification of the isolates by comparative sequence analysis [33–35]. Briefly, genomic DNA is extracted, an optimal gene target is amplified and sequenced, and the data are aligned and analyzed. The most common targets useful for a wide range of fungi are within the ribosomal DNA (rDNA) and include the internal transcribed spacer (ITS1 and ITS2) regions and the D1/D2 regions of the large ribosomal subunit. Sequence results are then compared against type strains or other credible deposits in a database using the BLASTn algorithm. GenBank is a commonly used database; however, it is non-curated, so there is no assurance that the sequence data deposited is from a correctly identified isolate, thus making it imperative that the molecular identification is compatible with the phenotypic features. While the ITS and D1/D2 regions are very useful, additional targets may be needed for some genera such as beta-tubulin (TUB), calmodulin (CAL), actin (ACT), CO1 (the mitochondrial cyctochrome oxidase 1 gene), the translation elongation factor (TEF), and others [36]. Other databases that are curated such as those at the Centraalbureau voor Schimmelcultures (CBS) and the online Fusarium database [37] are often necessary for a definitive identification. In light of cost containment and the dwindling number of individuals trained in classical morphologic identification, more laboratories are considering adding the sequencing of isolates in conjunction with phenotypic methods or as a stand-alone method. It should be noted that sequence-alone identification of limited or noninformative targets without a comparison of the phenotypic features has the potential for misidentification of isolates that could negatively impact patient management [36].
Taxonomy, Classification, and Nomenclature
Many volumes have been dedicated to the taxonomy, classification, and nomenclature of clinically significant fungi. Herein, this work only highlights some of the basic concepts. The classification scheme accepted by most authorities will be presented for the kingdom fungi. The term classification, in the fungal sense, refers to the application of names for the categories into which the taxa (taxonomic groups) may be grouped, with some subdivisions regarding their relative order. “Taxonomy” refers to this classification in a very systematic way, and nomenclature is the assigning of names to fungi. These processes, previously regulated by the rules of the International Code of Botanical Nomenclature (ICBN), are now under the auspices of the International Code of Nomenclature for algae, fungi, and plants. The Melbourne Code, adopted in 2011, and published in 2012 [3, 38], resulted in major changes which became effective January 1, 2013. Some of the most significants are as follows: (a) the abolishment of Article 59 of the previous ICBN, permitting multiple names for the same organism (such as one name for the anamorph and one for the teleomorph, i.e., such as the use of both Aspergillus fumigatus and Neosartorya fumigata); (b) the need to determine which name will be used (an ongoing process); and (c) the deposition of isolate information into a recognized repository for the valid publication of a fungal name. The following is an abbreviated classification scheme for the kingdom Fungi:
Group | Group Ending |
|---|---|
Kingdom | none |
Subkingdom | none |
Phylum | mycota |
Subphylum | mycotina |
Class | mycetes |
Order | ales |
Family | aceae |
Genus | no specific ending |
Species | no specific ending |
Variety | no specific ending |
The phyla in which the sexual or teleomorph forms of the majority of human/animal pathogens reside are the Ascomycota, Basidiomycota and the Glomeromycota (formerly the Zygomycota) [4]. An example of this classification scheme for the ascomycete, Microascus cinereus, recovered from lower respiratory sites [39], would look like this:
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree