Aspiration Pneumonia and Aspiration Pneumonitis
Pneumonia is a common cause of death among older people despite the availability of potent novel antimicrobials. Whereas the death rate of juvenile pneumonia has decreased nearly to zero, that of old people has remained unchanged over the past 100 years. In other words, the traditional approach has proven a limited success: as Osler put it over 100 years ago, ‘pneumonia is actually a friend to the old’.1 Both the increased incidence of pneumonia and high mortality among older people are a consequence of a number of age-related factors including coexisting illnesses, therapeutic interventions and decreased host defence mechanisms. In these, aspiration is possibly the most important risk factor for pneumonia in the elderly.2 Aspiration is defined as the inhalation of oropharyngeal or gastric contents into the larynx and the lower respiratory tract. Several pulmonary syndromes may occur after aspiration, depending on the amount and the nature of the aspirated material, frequency of aspiration and the host’s response to the aspirated material.3 Aspiration pneumonia is an infectious process caused by an inhalation of the oropharyngeal secretions that are colonized by pathogenic bacteria, whereas aspiration pneumonitis including Mendelson syndrome is a chemical injury caused by an inhalation of sterile gastric contents.3 Although there is some overlap between these syndromes, they are distinct clinical entities. This chapter focuses on the pathophysiology and the management of aspiration pneumonia and aspiration pneumonitis.
Mechanisms for Development of Aspiration Pneumonia or Aspiration Pneumonitis
Aspiration Pneumonia
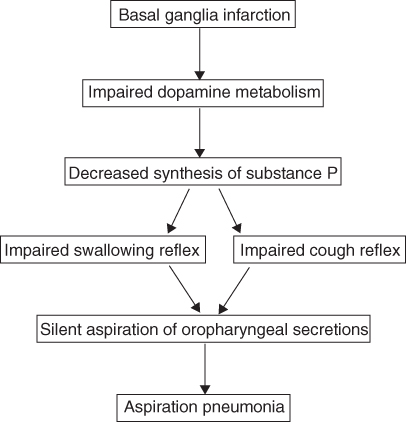
Pneumonia in the elderly is often caused by a non-apparent swallowing disorder.2 Such ‘silent aspiration’ frequently occurs and is a more important cause of pneumonia than acute aspiration of gastric content in older people.4 Silent aspiration of oropharyngeal bacterial pathogens to the lower respiratory tract is an important risk factor for community-acquired pneumonia5 and also nosocomial pneumonia in the elderly.6 Normal hosts are less likely to develop pneumonia because they aspirate smaller volumes or are able to clear bacteria rapidly.7 However, an extremely small volume (0.01 ml) of saliva contains pathogenic numbers of bacteria.7 Elderly patients with a predisposition to aspiration frequently aspirate oropharyngeal secretions and the development of pneumonia occurs when normal pulmonary defence mechanisms are overwhelmed.8 Adequate protective reflexes in the airway are important and suppression or absence of these reflexes has led to pneumonia.8 For example, Nakajoh et al. reported that the incidence of pneumonia was higher in patients having both a latency of swallowing response longer than 5 s following stimulation with 1 ml of distilled water and a cough threshold for inhalation of citric acid aerosol higher than a concentration of 1.35 (log mg ml−1).9 Thus, the progressive loss of protective reflexes (i.e. swallowing and cough reflexes) with age is thought to be one of the mechanisms for aspiration pneumonia, which is often seen in older people.10 In fact, impaired swallowing and cough reflexes have been shown in patients suffering from aspiration pneumonia.11 However, re-evaluation of age-related changes in protective reflexes in individuals who lead active daily lives has shown that both reflexes do not decrease with the advance of age,12, 13 indicating that involutional and degenerative changes associated with ageing often result in marginally compensated protective reflexes.14 Disorders of the central nervous system are more likely to develop in the elderly and pneumonia has been estimated to occur in about one-third of patients with stroke.15 The most important factor contributing to the development of pneumonia in patients with stroke is suggested to be dysphagia with aspiration.16 Nakagawa et al. have shown that the risk of pneumonia was significantly higher in patients with basal ganglia infarcts than in patients with or without cerebral hemispheric strokes in other locations.8 They found that multiple episodes of pneumonia occurred only in patients with bilateral basal ganglia infarcts and that there was a higher mortality rate associated with pneumonia in these patients.8 Delayed triggering of the swallowing reflex occurs in patients with infarcts in the basal ganglia.14 These results strongly suggest that disruption of basal ganglia functions is critically important in the development of aspiration pneumonia. The pharyngeal, laryngeal and tracheal epithelia, the most important sites for the initiation of swallowing and cough reflexes, have an extensive plexus of nerves that contains substance P.17, 18 Capsaicin desensitization, which diminishes substance P from the airway and upper digestive tract, or an administration of neurokinin (NK)-1 receptor antagonist remarkably attenuated the cough response to tussive stimuli19, 20 and distilled water-induced swallowing reflex in guinea pigs,21 suggesting an important role of substance P-containing nerves in the initiation of these protective reflexes. Thus, irritation of laryngeal and pharyngeal mucosa by stimuli may activate capsaicin-sensitive sensory nerves, releasing substance P, with the result that protective reflexes are initiated by stimulation of the glossopharyngeal and vagal sensory nerves.19 Treatment with a dopamine agonist in the rat brings about a heightened striosomal expression of substance P and both dopamine D1 and D2 antagonists decrease substance P.22 Mice lacking the dopamine D1 receptor23 and those treated with dopamine D1 receptor antagonist24 showed abnormal motor activities and feeding and swallowing problems. An impairment of dopamine metabolism in the basal ganglia is observed in patients with infarcts in the basal ganglia.25 Taking these facts together, the mechanisms of silent aspiration may be speculated as shown in Figure 48.1. Patients with basal ganglia infarcts may suffer from reduced dopamine metabolism, which decreases substance P in the glossopharyngeal and vagal sensory nerves. Reduction in substance P concentration in these nerves impairs both swallowing and cough reflexes, which increases the frequency of silent aspiration. Because the action of swallowing and coughing is a fundamental defence mechanism against aspiration of oropharyngeal contents into the respiratory tract, impairment of both reflexes is one of the major reasons for the development of aspiration pneumonia (see Figure 48.1). In patients with aspiration pneumonia, unlike those with aspiration pneumonitis, the episode of aspiration is generally not witnessed. The diagnosis is therefore inferred when a patient at risk for aspiration has radiographic evidence of an infiltrate in a characteristic bronchopulmonary segment. Elderly persons frequently receive poor oral care, resulting in oropharyngeal colonization by potential respiratory tract pathogens, including Enterobacteriaceae, Pseudomonas aeruginosa and Staphylococcus aureus. These pathogens are aspirated and may cause pneumonia.3
Figure 48.1 Possible mechanisms for development of aspiration pneumonia in patients with basal ganglia infarction.
Aspiration Pneumonitis
Aspiration pneumonitis is defined as acute lung injury after the inhalation of regurgitated sterile gastric contents. This syndrome occurs in patients who have a marked disturbance of consciousness such as that resulting from a drug overdose, seizures, a massive cerebrovascular accident or the use of anaesthesia.3 The syndrome most commonly described as aspiration pneumonitis is Mendelson syndrome.26 Reflux of gastric fluids into the airway can damage the respiratory tract.27 Marked damage to the tracheal mucosa can occur even when the volume of aspirated gastric fluid is too small to cause clinically significant aspiration pneumonitis and repeated long periods of aspiration of gastric fluid may even cause interstitial pulmonary fibrosis. Damage is always more severe when the pH of the gastric contents is low, but gastric fluid also contains substances other than acid which cause airway damage and delay healing of the airway epithelial damage.3, 27 Since airway epithelial damage by gastric content probably arises from the additive effects of acidity,27 treatment of gastroesophageal reflux using antiacids such as histamine-H2 receptor antagonists alone may not improve symptoms caused by aspiration of gastric fluids.3
Treatments for Aspiration Pneumonia and Aspiration Pneumonitis
Aspiration Pneumonia
Antibiotic therapy is unequivocally indicated in patients with aspiration pneumonia. The choice of antibiotics should depend on the setting in which the aspiration occurs and also the patient’s general health. However, antibiotic agents with activity against Gram-negative organisms, such as third-generation cephalosporins, fluoroquinolones and piperacillin, are usually required.3 Kanda et al. evaluated an additive effect of angiotensin-converting enzyme (ACE) inhibitor and amantadine to the conventional antibiotic therapy for pneumonia and found that the combined administration of these drugs can shorten the duration of hospitalization and antibiotic use, inhibit methicillin-resistant Staphylococcus aureus (MRSA) infection and lower the medical cost for treatment of pneumonia.28
Aspiration Pneumonitis
Although it is common practice, the prophylactic use of antibiotics in patients in whom aspiration is suspected or witnessed is not recommended.3 However, empirical antibiotic therapy is appropriate for patients who aspirate gastric contents and who have small-bowel obstruction or other conditions associated with colonization of the gastric contents.3 Antibiotic therapy should be considered for patients with aspiration pneumonitis that fails to resolve within 48 h after aspiration. Empirical therapy with broad-spectrum agents such as fluoroquinolone or piperacillin is recommended. Corticosteroids have been used for decades in the management of aspiration pneumonitis. However, there are limited data on the role of these agents.29
Strategies for the Prevention of Aspiration Pneumonia (Figure 48.2)
Pharmacological Therapy
Capsaicin
Because substance P is a neurotransmitter of the swallowing reflex and is depleted in patients with aspiration pneumonia,30 capsaicin, a pungent substance in red peppers that stimulates sensory nerves, may improve the swallowing reflex in these patients.2 Ebihara et al. measured the swallowing reflex with a bolus injection of 1 ml of distilled water into the pharynx through a nasal catheter and suggested that the addition of a low dose of capsaicin to liquid or food may stimulate the swallowing reflex and help to prevent aspiration pneumonia in the elderly.31
Angiotensin-Converting Enzyme (ACE) Inhibitors
A well-known adverse effect of ACE inhibitors is a dry cough.32 Since substance P is degraded by ACE,33 its action is potentiated by ACE inhibitors.34 Using ACE inhibitors, substance P might accumulate in the upper respiratory tract because of inhibited ACE activity and cause an increase in the sensitivity of the cough reflex.2, 20 In a similar way to the cough reflex, ACE inhibitors improve the swallowing reflex in older patients with aspiration pneumonia.2 Sekizawa et al. compared the rate of pneumonia in stroke patients with hypertension treated by ACE inhibitors with that in stroke patients treated by other antihypertensive drugs and found that the risk of pneumonia is reduced by about one-third if ACE inhibitors are used for hypertension compared with the use of other antihypertensive drugs.35 ACE inhibitors, therefore, may have beneficial effects on the prevention of pneumonia in these patients. Arai et al. reported that the rate of pneumonia was significantly lower in elderly hypertensive patients given ACE inhibitors than that in those treated with calcium channel blockers.36 However, Teramoto and Ouchi refuted the advantage of ACE inhibitors over calcium channel blockers in preventing pneumonia in adult and elderly subjects with hypertension.37 In elderly individuals, the severity of the underlying cerebrovascular disease greatly affects susceptibility to pneumonia. ACE inhibitors could be useful in the prevention of aspiration pneumonia in elderly patients with stroke but not in those without stroke.
Dopamine and Amantadine
Delayed triggering of the swallowing reflex occurs in patients with basal ganglia infarctions2 and an impairment of dopamine metabolism in the basal ganglia is observed in these patients.25 Kobayashi et al. investigated whether levodopa improves the swallowing reflex in patients with basal ganglia infarctions who had a history of aspiration pneumonia.38 The subjects were given an intravenous drip infusion of levodopa (50 mg in 20 ml of saline) for 30 min. They found that the administration of levodopa improved the impaired swallowing reflex in these patients. Since dopamine supplementation improves the swallowing reflex in patients with cerebral infarctions, Nakagawa et al. investigated whether amantadine, a drug that acts as a dopamine releaser from dopaminergic nerve terminals, lowers the incidence of pneumonia in patients with cerebral infarctions.39
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree