ANTERIOR PITUITARY GLAND AND PREGNANCY
The normal pituitary gland enlarges during pregnancy, predominantly because of the estrogen-stimulated hyperplasia and hypertrophy of the prolactin (PRL)-producing lactotropes.10 PRL levels rise gradually throughout gestation.11 This stimulatory effect of pregnancy on the pituitary has important implications for the patient with a preexisting prolactinoma who desires pregnancy.
In the second half of pregnancy, pituitary growth hormone (GH) secretion falls, and levels of a GH variant made by the syncytiotrophoblastic epithelium of the placenta increase in the circulation to as high as 10 to 20 ng/mL.12,13 The decreased production of normal pituitary GH presumably results from negative feedback effects of the placentally produced variant.12,13 In patients with acromegaly who have autonomous GH secretion and become pregnant, both forms of GH persist in the blood throughout pregnancy.14
PROLACTINOMA
Hyperprolactinemia is responsible for approximately one-third of all cases of female infertility.15,16 Hyperprolactinemia impairs
the hypothalamic–pituitary–ovarian axis at several levels, the primary site of inhibition being at the hypothalamus.16 The differential diagnosis of hyperprolactinemia is extensive (see Chap. 13).
the hypothalamic–pituitary–ovarian axis at several levels, the primary site of inhibition being at the hypothalamus.16 The differential diagnosis of hyperprolactinemia is extensive (see Chap. 13).
For patients with prolactinomas, the choice of therapy may have important consequences for decisions regarding pregnancy. Transsphenoidal surgery is curative in 50% to 60% of cases and rarely causes hypopituitarism when it is performed on women with microadenomas. However, it cures a much smaller number with a considerably greater risk of causing hypopituitarism when it is performed for macroadenomas, and may affect fertility.16
Bromocriptine therapy restores ovulatory menses in 80% to 90% of women (see Chap. 13 and Chap. 21). Once this has been accomplished, and if pregnancy is desired, mechanical contraception is used until the first two or three cycles have occurred, so that an intermenstrual interval can be established. In this way, a woman will know when she has missed a menstrual period, a pregnancy test can be performed quickly, and the precise gestational age of the fetus will be known. Moreover, bromocriptine will have been given for only 3 to 4 weeks of the gestation. In addition to its efficacy in lowering PRL levels, bromocriptine reduces the size of PRL-secreting macroadenomas by at least 50% in more than half of all patients.16
Cabergoline is a dopamine agonist that is given just once or twice weekly. Cabergoline is as effective as, if not more effective than, bromocriptine in lowering PRL levels and is clearly better tolerated.17 In addition, cabergoline has similar efficacy to bromocriptine in reducing tumor size.18,19
EFFECTS OF PREGNANCY ON PROLACTINOMA GROWTH
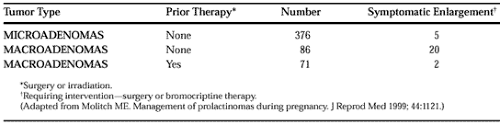
In women with prolactinomas, the stimulatory effect of the hormonal milieu of pregnancy may result in significant tumor enlargement during gestation (Fig. 110-1). In a survey of 19 reported series,20 symptomatic tumor enlargement (producing headaches, visual field disturbance) occurred during pregnancy in 5 of 376 women with PRL-secreting microadenomas treated only with bromocriptine (Table 110-1). The reviewed series included 86 pregnant women with macroadenomas; 20 (23.3%) had symptomatic tumor enlargement. Of 71 women with macroadenomas treated with irradiation or surgery before conception, only 2 (2.8%) had symptomatic tumor enlargement, and none had asymptomatic tumor enlargement during gestation. Twenty-five percent to 50% of patients with symptomatic tumor enlargement require intervention. Bromocriptine therapy usually is successful in reducing the size of the tumor, but transsphenoidal surgery may be necessary.19
EFFECTS OF HYPERPROLACTINEMIA AND ITS TREATMENT ON PREGNANCY
Bromocriptine taken for only the first few weeks of gestation has not been associated with any increase in spontaneous abortions, ectopic pregnancies, trophoblastic disease, multiple pregnancies, or congenital malformations20,21 (Table 110-2).The experience with bromocriptine given throughout pregnancy is limited, however. One malformation (talipes) has been reported in 114 such pregnancies,21 which is not an unexpected frequency. However, because bromocriptine crosses the placenta,22 it should not be used any longer than necessary during pregnancy. The effects of cabergoline usage on fetal outcome has been documented in just over 200 cases; it appears to be safe.23 Because of this relatively limited experience, however, bromocriptine would appear to be the preferred dopamine agonist when fertility is the primary concern of therapy. The effects of transsphenoidal surgery during gestation are not known specifically but would not be expected to be significantly different from the effects of other types of surgery (unless hypopituitarism should ensue).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree