ADRENALECTOMY
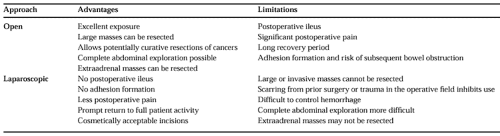
The adrenal glands lie at a central, deep position within the body, and several different surgical approaches have been devised for their safe removal. Either adrenal gland may be resected using an open anterior transperitoneal approach or using minimally invasive laparoscopic methods. Laparoscopic adrenalectomy has essentially replaced the open posterior approach, which provided access to the adrenals through the back. General anesthesia is required for each operation. Several important factors are considered when choosing the surgical approach (Table 89-3). These include preoperative diagnosis, size and location of any adrenal mass, potential for malignancy, involvement of extraadrenal structures, the need to explore the entire abdomen, previous surgery in the planned operative area, and patient factors.
The trend has been increasingly in favor of using a laparoscopic approach for adrenalectomy whenever possible.9a,9b Data that have accrued with laparoscopic adrenalectomy have reproducibly demonstrated efficacy equivalent to that of open surgery in treating certain adrenal conditions and significantly reduced postoperative patient rehabilitation. In addition, ileus does not occur after laparoscopic surgery, and intraperitoneal adhesion formation is avoided, so that the associated risk of subsequent bowel obstruction is eliminated. For the surgeon, the magnification and clarity provided by modern videoscopic systems enable close visualization of deep regions and dissection with fine detail.
Requirements that must be satisfied for laparoscopic adrenalectomy include a benign condition, mass diameter <5 to 6 cm, noninvolvement of adjacent structures, no history of surgery or trauma resulting in scarring in the planned surgical field, surgeon experience in advanced laparoscopy and open adrenalectomy, and acceptable patient factors. Laparoscopic adrenalectomy is the procedure of choice for small functional adenomas causing aldosteronism or Cushing syndrome, small pheochromocytomas, small adrenal incidentalomas, and bilateral hyperfunctioning adrenal glands (e.g.,
primary pigmented micronodular adrenal hyperplasia). Large adrenal masses (>5–6 cm diameter) and those that are thought to be malignant should be resected using an open anterior transperitoneal approach. A thoracoabdominal incision with the patient in a partial lateral decubitus position may be used for open resection of localized large masses. Open surgery enables appropriate exposure for potentially curative cancer resections. In addition, thorough exploration of the entire abdomen, retroperitoneum, and contralateral adrenal gland is easily accomplished with an open anterior approach to accurately identify and resect all disease and to evaluate the extent of disease. Large sporadic pheochromocytomas and adrenocortical carcinomas should be resected with open surgery.
primary pigmented micronodular adrenal hyperplasia). Large adrenal masses (>5–6 cm diameter) and those that are thought to be malignant should be resected using an open anterior transperitoneal approach. A thoracoabdominal incision with the patient in a partial lateral decubitus position may be used for open resection of localized large masses. Open surgery enables appropriate exposure for potentially curative cancer resections. In addition, thorough exploration of the entire abdomen, retroperitoneum, and contralateral adrenal gland is easily accomplished with an open anterior approach to accurately identify and resect all disease and to evaluate the extent of disease. Large sporadic pheochromocytomas and adrenocortical carcinomas should be resected with open surgery.
The inability to complete an adrenalectomy using laparoscopic methods also requires conversion to an open operation. Conditions that technically prevent a laparoscopic approach are large masses (generally >5–6 cm in diameter), involvement of extraadrenal structures, scarring that makes dissection difficult, significant bleeding, poor visualization, inconclusive anatomy, and equipment malfunction. Therefore, every surgeon performing laparoscopic adrenalectomy must be proficient in open abdominal and retroperitoneal surgery. The anatomic perspective with laparoscopic adrenalectomy may be unfamiliar to a surgeon inexperienced with this approach, and the added magnification provided by laparoscopy may lead to misidentification of important structures. Dissection of the vascular adrenal with inadequate hemostasis may cause bleeding that compromises visualization and the ultimate success of a laparoscopic approach. The adrenal glands themselves may be very difficult to locate with laparoscopy because only visualization and not palpation is possible, and the adrenals are embedded in retroperitoneal fat of similar color and consistency. The availability of laparoscopic intraoperative ultrasonography and familiarity with this advanced technique are necessary to locate the adrenal glands in difficult cases without converting to an open procedure. In addition, laparoscopic ultrasonography may be used to identify the location of important vascular structures so that injury is avoided.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree