6 Administration Setting Up a Lymphedema Clinic Suggested Materials to Start Up a Lymphedema Program Reducing the size of a lymphedematous extremity back to a normal or near normal volume is rewarding for both the patient and the therapist. This rewarding and clinically challenging experience is payback for the hardship the patient has had to endure and any obstacles a health care professional may have had to overcome prior to establishing a lymphedema clinic. This chapter focuses on some key points in the establishment of a lymphedema clinic, whether it is a free-standing treatment center or part of an existing clinic or department. Among the factors influencing the establishment of a well-run lymphedema clinic are the selection of personnel, the determination of required space and equipment, and marketing issues in promoting the clinic. A high level of competency and skill is needed to master all components of complete decongestive therapy and to provide patients with the proper degree of intervention. The quality of training will have a great impact on the level of care the patients receive. To provide a high standard of care, it is necessary that the therapists are specifically educated and trained in lymphedema management. It is highly recommended that therapists complete a training program in CDT, consisting of 135 classroom hours attained from one training program. The training should consist of one-third theoretical instruction and two-thirds practical hands-on work. Successful lymphedema management requires daily treatments in the intensive phase; it is therefore desirable to employ two lymphedema therapists to cover for absence and for professional exchange and support. In a freestanding treatment center, it is also necessary to have at least one more person covering the phone and reception area, as well as dealing with insurance and billing issues. Regulations concerning minimum space and design requirements for health care facilities (health centers, suites, or clinics) may vary from state to state. Regulations can be obtained from professional associations. It is desirable to have two treatment rooms per therapist, two bathrooms, a shower, an exercise room, a reception area (to include a waiting room), and a storage room. Treatment room: ~80–100 square feet (~7–9 square meters) per room with the following equipment: treatment table (adjustable in height and able to support patients’ weight), chair, clothes hanger, rolling stool, shelf with bandaging and padding materials, and patient education materials The best patient scheduling is achieved by having two therapy rooms per therapist. If you allow ample time between patients, you may be able to function well with one room per therapist. Bathroom/shower: ~50 square feet (~5 square meters) per bathroom, wheelchair accessible. For appropriate patient hygiene, a shower within the treatment center is desirable. Patients have to wear the compression bandages between the daily treatment sessions and often remove the bandages at home before taking a shower. It is imperative for treatment success that the bandages are not removed at the patient’s home (except if they cause pain or numbness in the extremity). Patients taking a shower at their home should protect the bandaged extremity with either a cast shield or a large trash bag. If a shower is not available in the treatment facility, patients should shower at home with the covered bandages in place, remove the bandages in the clinic, and wash the extremity with a washcloth at the clinic’s sink. Exercise room: ~300–500 square feet (~28–46 square meters) to accommodate exercise mats. For group exercises or support group meetings, a room size of ~1000 square feet (~305 square meters) is appropriate. Reception area: ~400 square feet (~37 square meters) to accommodate patient waiting room, record storage, documentation space, and other materials Storage room: ~50 square feet (~5 square meters) to accommodate bandaging materials and other items The basic equipment needed for a well-run lymphedema clinic includes the following: • Furniture for the reception area and treatment rooms • Adjustable treatment tables • Compression materials (see Suggested Materials to Start Up a Lymphedema Program later in this chapter) • Audiovisual equipment and other materials for patient education • Computer(s) and software (limb measurement program) • Digital camera(s) • Measuring tape(s) and documentation forms • Manual sphygmomanometer(s) • Exercise equipment (soft balls, sticks, therabands, etc.) • Basic office supplies Whether the lymphedema treatment center is freestanding or part of an existing clinic or department, referral sources must be developed to ensure success. The following suggestions should be considered to make the clinic’s presence known to the lymphedema community and to physicians. Direct mailings or visits to physicians in the community: The information source should contain a brochure outlining the clinic’s services. When designing the brochure, it should be kept in mind that physicians are busy and prefer information that is precise, short, and to the point. A photo depicting a lymphedema patient before and after treatment with manual lymph drainage and complete de-congestive therapy on the cover page of the brochure is always helpful to bring the point across. Certified therapist listing on websites: Training centers for CDT generally contain a listing of their graduates on their websites, which can be accessed by patients seeking certified therapists. Certified therapist listings in publications relevant to lymphedema: The National Lymphedema Network distributes a quarterly publication. This publication contains valuable information for lymphedema patients and therapists. For a fee, therapists and clinics may be listed in the resource guide of this publication. Brochures: Brochures outlining the services provided should be distributed at health fairs and breast cancer/lymphedema-related events and at the offices of oncologists and vascular and plastic surgeons. In-service presentations: Presentations can be given at local clinics and health care facilities. It is helpful to bring educational materials (posters, slides) to support each presentation. Advertisements: Local newspapers and other media are appropriate vehicles for advertising services. Insurance companies: The provider relations department of insurance companies offering coverage in the service area should be contacted and be made aware of the services the facility offers. An adequate inventory of supplies should be on hand before the lymphedema program opens. The treatment center should keep a sufficient quantity of compression materials in stock, or the patients themselves should be told to order the materials needed directly from a distributor before the initial treatment. The approximate quantity of compression materials needed for each individual patient during the decongestive phase is determined during the evaluation. A detailed description of the materials used in lymphedema management and a listing of recommended materials used for upper and lower extremity lymphedema bandaging are given in Chapter 5, Required Materials. The initial expense to keep a sufficient amount of lymphedema bandaging supply in stock is approximately $2500–$3000 (this should cover ~10–15 patients). • Short-Stretch Bandages – 10 rolls of 4 cm – 20 rolls of 6 cm – 20 rolls of 8 cm – 40 rolls of 10 cm – 5 rolls of 10 cm × 10 m (double length) – 40 rolls of 12 cm – 5 rolls of 12 cm × 10 m (double length) • Wide-width short-stretch bandages (white bandages) – 5 rolls of 15 cm – 5 rolls of 20 cm • Padding bandages – 30 rolls of 10 cm – 40 rolls of 15 cm – (Best is 0.25 inch [6 mm] and 0.5 inch [12 mm] thickness with a recommended density of ~1.6 pounds [725 g] per cubic foot, one sheet each) • High-density foam – 10 pieces small Komprex kidney (size 0) – 2 pad rolls (8 cm × 2 m × 1 cm) – 4 sheets (100 cm × 50 cm × 1 cm) • Foam padding rolls (Rosidal Soft)—can be used instead of gray foam – 30 rolls of 10 cm – 15 rolls of 15 cm • Gauze bandages (finger and toe bandages) – Mollelast: 10 boxes (200 rolls) of 4 cm × 4 m, or 8 bags of Elastomull 1 inch × 4.1 yards (2.5 cm × 3.7 m) – 10 boxes (200 rolls) of 6 cm × 4 m, or 17 bags of Elastomull 2 inch × 4.1 yd (5 cm × 3.7 m) – Transelast (skin colored): 10 boxes (200 rolls) of 6 cm × 4 m • Stockinettes (tubular gauze) – 2 boxes for small arms or children’s legs (Lohmann size 5 or Tricofix D5) – 2 boxes for “normal” arms and lower legs (Lohmann size 6 or Tricofix E6) – 4 boxes for big arms and “normal” legs (Lohmann size 7 or Tricofix E6) – 5 boxes for very big arms and bigger legs (Lohmann size 9 or Tricofix F7/G9) – 2 boxes for very big legs, small trunk (Lohmann size K1) – 2 boxes for extremely large legs and trunk (Lohmann size K2) • Lotion – 10–15 × 8 ounce (236 ml) bottles, or 5 × 32-ounce (946 ml) bottles (Lymphoderm, Eucerin, etc.) • Other – 5 bandage winders – Educational materials (posters, etc.) Some distributors offer prepacked bandage kits for lymphedema management. These kits are available for either upper or lower extremity lymphedema bandaging and typically contain two complete sets of short-stretch bandages, stockinettes, padding, and gauze bandages. Foam generally is not included and must be ordered separately. Ordering kits instead of separate items may simplify the ordering process, but distributors typically charge an additional amount for the packaging process. If providers work on a private pay basis, a reasonable charge will have to be established, covering all expenses (including bandages, padding materials, etc.), plus profit. A price list detailing all parts of the treatment should be posted in the treatment center. Health care reimbursement is an ever changing and very complex issue. Lymphedema management services are provided by physical therapists, physical therapist assistants, occupational therapists, occupational therapist assistants, massage therapists, and nurses. Insurance reimbursement may vary depending on providers and practice settings. Providers should confer with insurance companies to inquire about reimbursement policies for their individual professional group. It is also advisable to consult respective professional associations for the most current updates and regulations. During the past few years the Women’s Health and Cancer Rights Act of 1998 (WHCRA) has had a positive impact on reimbursement for lymphedema management. This federal law, which became effective on October 21, 1998, requires group health plans (as well as payers providing individual coverage) that provide coverage for mastectomies, to also cover reconstructive surgery and prostheses following mastectomies. The treatment and management of physical complications resulting from mastectomies, such as lymphedema, are also covered under this act. Not included in the statutes of this act is the type of treatment that must be provided. This decision is left to the individual insurance provider to determine. Patients who had problems getting insurance coverage before the WHCRA became effective should contact their insurance company and ask the following questions: 1. Does the Women’s Health and Cancer Rights Act of 1998 affect my coverage for lymphedema treatment? 2. Does my insurance policy cover manual lymph drainage and complete decongestive therapy (Current Procedural Terminology [CPT] code 97140) for the treatment of my lymphedema? 3. Is it necessary that a physical therapist perform the manual lymph drainage/complete decongestive therapy to be reimbursed, or can an occupational therapist, registered nurse, or massage therapist administer the therapy? Patients should also contact their state’s insurance department to find out whether the WHCRA will apply to the coverage if they are part of an insured group plan or individual health insurance. Payers generally do not cover compression bandages and compression garments. Recent improvement has been seen in the coverage for gradient compression garments. Effective as of October 1, 2003, the Centers for Medicare and Medicaid Services (CMS) approved coverage for compression garments in the treatment of venous stasis ulcerations. Coverage may be provided for garments delivering compression between 30 and 50 mmHg and if the patient has an open venous stasis ulcer that has been treated by a physician or another health care professional. The CMS article states in part that compression garments that serve a therapeutic or protective function may be covered if certain requirements are met. Because successful long-term lymphedema management depends on gradient compression garments as well, the lymphedema community should advocate for extended coverage to include lymphedema care. Lymphedema clinics obtain their compression materials from vendors specialized in the distribution of lymphedema management materials. Depending on the individual practice setting, patients may reimburse the providers for materials used or order the necessary supplies directly from vendors. Correct coding is one of the most important, and often one of the most frustrating, aspects of successfully operating a practice for lymphedema management. Correct coding is something of a science, made even more complex by frequent changes in the definitions of the codes and the approved methods of combining them. The five-digit codes apply to medical services or procedures performed by health care providers. The Current Procedural Terminology codes are established by the CPT editorial panel of the American Medical Association and have become the industry’s coding standard for reporting. The following CPT codes are commonly used in billing for lymphedema management; health care providers should be aware that the interpretation of these codes by various payers might vary. • Timed codes When billing Medicare for any of the timed codes, the providers must follow appropriate CMS guidelines regarding unit of service requirements. – Evaluation codes – 97001: Physical therapy evaluation – 97003: Occupational therapy evaluation • Therapy codes – 97140: Manual therapy techniques (e.g., mobilization/manipulation, manual lymphatic drainage, manual traction), one or more regions. Charge is based on 15-minute increments. – Depending on the condition, the MLD portion of the treatment may last between 30 minutes and 1 hour. – 97530: Therapeutic activities, direct (one-on-one) patient contact by the provider (use of dynamic activities to improve functional performance). Based on 15-minute increments. – Can be used with or without bandages on the affected extremity – 97110: Therapeutic procedure, one or more areas. Based on 15-minute increments. Therapeutic exercises to develop strength and endurance, range of motion, and flexibility. – Can be used with or without bandages on the affected extremity (theraband, ball, etc.) – 97535: Self-care/home management training. Self-care management, patient education in self-MLD for home program, self-bandaging, Do’s and Don’ts, and appropriate activity guidelines. Charge is based on 15-minute increments. – 97750: Physical performance test, measurements. Circumferential and/or volumetric measurements, with written report (measurement forms, volume programs). Charge is based on 15-minute increments. – 97504: Orthotics fitting and training. Pressure garment measurements for upper or lower extremity and trunk – 97039: Unlisted therapeutic procedure. Skin care, breathing exercises, deep abdominal techniques, therapist’s application of low-pH skin lotion, antibiotic ointment or other skin treatments on the affected limb prior to bandaging. – ICD-9 codes ICD-9 codes describe medical procedures performed by physicians and other health providers. The ICD-9 codes were developed by the Health Care Financing Administration (now the CMS) to assist in the assignment of reimbursement amounts to providers by Medicare carriers. A large number of managed care and other insurance companies, however, base their reimbursements on the values established by the CMS. – 457.0 Postmastectomy lymphedema – 457.1 Other lymphedema – 757.0 Chronic hereditary lymphedema – 729.81 Swelling of limb (upper and lower extremity) – 629.8 Swelling of female genital organ – 608.86 Swelling of male genital organ – 607.83 Swelling of penis The following is a compilation of sample from that may be helpful in the process of establishing a lymphedema clinic.
Setting Up a Lymphedema Clinic
Personnel
Required Space
Equipment
Marketing Issues
Suggested Materials to Start Up a Lymphedema Program
Reimbursements and Billing
CPT Codes
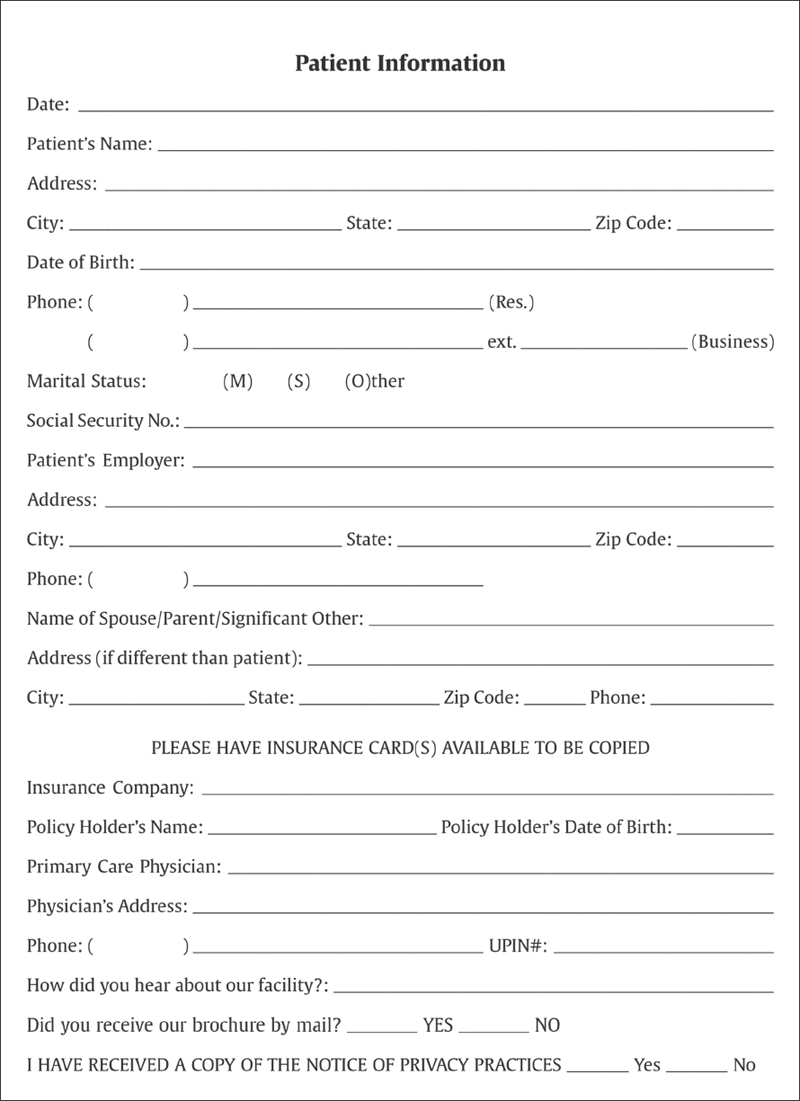
Sample Forms and Templates
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree