Regimen
Dose
Cycle duration
No cycles
Notes
Reference
Non-anthracycline containing
Oral CMF
Cyclophosphamide (100 mg/m2, PO) d1 to 14
Methotrexate (40 mg/m2) d1, 8
5-Fluorouracil (500 mg/m2) d1, 8
q4 weeks
6
Nonstandard IV CMF (600/60/600 mg/m2), d1, 8, q4 weeks is occasionally given
TC
Docetaxel (T; 75 mg/m2)
Cyclophosphamide (600 mg/m2)
q3 weeks
4
[10]
Anthracycline containing
AC
Doxorubicin (A; 60 mg/m2)a
Cyclophosphamide (600 mg/m2)
q3 weeks
4
Dose-dense AC is given q2 weeks with dfilgrastim support
FAC
5-Fluorouracil (500 mg/m2)
AC (50/500 mg/m2)b
q3 weeks
6
CAF
Cyclophosphamide (600 mg/m2)
Doxorubicin (A; 30 mg/m2)b d1, 8
5-Fluorouracil (500 mg/m2)
q4 weeks
6
C may be given PO at 100 mg/m2 on d1 to 14 of each cycle
[14]
FEC60 (Canadian)
5-Fluorouracil (500 mg/m2)
Epirubicin (60 mg/m2)c
Cyclophosphamide (75 mg/m2, PO) d1 to14
q4 weeks
6
[15]
FEC100
5- Fluorouracil (500 mg/m2)
Epirubicin (100 mg/m2)c
Cyclophosphamide (500 mg/m2)
q3 weeks
6
Filgrastim support should be considered
[16]
Anthracycline and taxane containing
AC → T
Dose-dense AC a,d → Paclitaxel (T; 175 mg/m2)
AC → Paclitaxel (T; 80 mg/m2)
q2 weeks
q3 weeks → weekly × 12
4 → 4
4 → 12
[17]
[18]
FEC100 → D
FEC 100 → Docetaxel (T; 75 mg/m2)
q3 weeks
3 → 3
Filgrastim support should be considered
[16]
FEC100 → P
FEC 100 → Paclitaxel (P; 100 mg/m2)
q3 weeks → weekly × 8
4 → 8
[19]
TAC
Docetaxel (T; 75 mg/m2)
AC (50/500 mg/m2)a, d
q3 weeks
6
Filgrastim support should be considered
[12]
Commonly used regimens for breast cancer are summarized in Table 23.1 and can broadly be divided into:
1.
Non-anthracycline-containing regimens (i.e., CMF and TC)
2.
Anthracycline-containing regimens (i.e., AC, FAC, FEC)
3.
Anthracycline- and taxane-containing regimens which incorporate both anthracyclines and taxanes (i.e., AC → T, FEC → taxane and TAC)
The Early Breast Cancer Trialists’ Collaborative Group (EBCTCG) has published a large meta-analysis of different polychemotherapy regimens used in over 100,000 women from 123 randomized trials [1]. The most effective adjuvant chemotherapy regimens included both anthracycline and taxanes, but these were also associated with the highest frequency of toxicity. Overall, the addition of adjuvant chemotherapy reduced breast cancer mortality by about one third, and the proportional risk reductions in the trials analyzed were only minimally affected by age, tumor burden (tumor size and nodal status), tumor grade, ER status, or tamoxifen use.
A summary of the key findings are as follows [1]:
Standard AC (4 cycles) and standard CMF (6 cycles) are equivalent.
Anthracycline-based regimens such as FAC or FEC, which have a higher cumulative anthracycline dosage than standard AC (4 cycles), are superior to standard oral CMF (6 cycles).
The addition of 4 cycles of a taxane to a fixed anthracycline-based control regimen reduced breast cancer mortality. However, there was no significant difference in outcomes when the extra 4 taxane cycles were counterbalanced with extra cycles of a non-taxane chemotherapy.
More recently, results from the large phase III randomized National Surgical Adjuvant Breast and Bowel (NSABP) B-38 trial were reported, comparing the three adjuvant chemotherapy regimens, dose-dense AC → T, dose-dense AC → T plus gemcitabine, and TAC, in a large cohort of approximately 5,000 patients (65 % with nodal involvement and 80 % with ER-positive disease) [20]. The 5-year DFS and overall survival (OS) rates were similar in all three groups; however, the incidence of grade 3 or 4 toxicity was the lowest with the AC → T regimen.
Another area of variability is the frequency of administering chemotherapy. Dose-dense chemotherapy typically refers to the administration of chemotherapy over a shorter interval. The best example of this is with AC, which can be administered at the same doses in a standard three-weekly interval or a dose-dense fashion every 2 weeks [9, 11]. With treatment administered every 2 weeks, growth factor support with filgrastim is required. With dose-dense AC regimens, paclitaxel may be given following AC either every 2 weeks for 4 cycles or weekly for 12 weeks (at 175 mg/m2 and 80 mg/m2, respectively), and it is unclear at this point if either approach is associated with improved outcomes. A recent meta-analysis of dose-dense chemotherapy for early breast cancer, which included 10 randomized trials involving over 10,000 patients, reported a better DFS and OS with dose-dense regimens, particularly in women with HR-negative breast cancer [21].
Chemotherapy in Different Breast Cancer Subtypes
Endocrine therapy forms the basis of adjuvant therapy in patients with HR-positive breast cancer, and the addition of chemotherapy benefits a subset of these patients. When given for HR-positive breast cancer, adjuvant chemotherapy usually sequenced ahead of, and completed before endocrine therapy. In patients with HER2/neu-positive tumors, HER2-directed therapy alone has not been tested in large adjuvant trials, and the addition of chemotherapy given concurrently with HER2-directed therapy is considered to be the current standard of care. Finally, for TNBC, there are no targeted therapies recommended for use outside of a clinical trial in the adjuvant setting, and combination chemotherapy remains the standard of care.
Chemotherapy in Hormone Receptor-Positive Breast Cancer
While adjuvant endocrine therapy is the standard of care in patients with tumors that express HRs, the indication for adjuvant chemotherapy in patients with HR-positive disease is undergoing reevaluation. Adjuvant chemotherapy is typically given in sequence with, and prior to, endocrine therapy, as there have been conflicting outcomes with concurrent therapy [22–24]. On average, patients with HR-positive breast cancers derive less benefit from chemotherapy compared to HR-negative tumors [25]. However, there still appears to be a subset of patients with HR-positive tumors that are chemosensitive. The basis for the addition of chemotherapy to adjuvant endocrine therapy is usually guided by the clinician’s estimation of prognosis and assessment of the endocrine- and chemosensitivity of the tumor. Patients for whom systemic chemotherapy should be strongly considered include patients with grade 2 or 3 disease, those with high-risk features based upon the gene signature (such as Oncotype DX and MammaPrint), and patients with a higher disease burden. That said, not every patient with node-positive disease has to be treated with chemotherapy, and multigene signatures are particularly useful in guiding the clinicians in regards to the decision to recommend chemotherapy [26].
The EBCTCG overview reported a benefit in terms of 5-year recurrence-free survival with adjuvant sequential chemoendocrine therapy over endocrine therapy alone with hazard ratios of 0.64 and 0.85 in patients with ER-positive tumors aged <50 and >50 years, respectively [27]. The larger impact of chemotherapy in younger patients may be partially explained by the endocrine effect of chemotherapy on ovarian function [6]. Similar long-term DFS benefits with the addition of chemotherapy to adjuvant endocrine therapy were also noted in the phase III randomized NSABP B-20 and Southwest Oncology Group (SWOG) 8814 trials [26, 28]. The identification of predictors of chemosensitivity in HR-positive tumors has been identified as a key challenge.
There is evidence suggesting an inverse relationship between HR expression and chemotherapy benefit in luminal breast cancers. In a study of postmenopausal women with ER-positive and node-positive cancers from the International Breast Cancer Study Group (IBCSG) Trials VII and 12-93, the addition of adjuvant chemotherapy to endocrine therapy improved the DFS (hazard ratio = 0.81, p = 0.02, median follow-up of 13 years) [29]. Nonparametric subpopulation treatment effect pattern plot (STEPP) analyses demonstrated that this benefit was limited to the patients whose tumors had low to intermediate levels of estrogen expression. The level of ER appears to predict the response to both endocrine and chemotherapies in opposite directions, but these factors may not entirely overlap. It is likely that there are other biological factors that interact with the ER-signaling pathway to determine chemosensitivity. The assumption that chemosensitivity is inversely related to endocrine sensitivity in ER-positive breast cancer is therefore not clearly defined. Tumors that are endocrine sensitive may also be chemosensitive; conversely, endocrine resistant tumors with poor prognostic factors may not always be chemosensitive.
One biomarker that has been examined in chemosensitive ER-positive tumors is Ki67, a marker of cellular proliferation. In an analysis of 1,521 premenopausal and postmenopausal patients with ER-positive tumors from the IBCSG VIII and IX trials, respectively, a high Ki67 index was found to be associated with poorer DFS, but did not predict an OS benefit with the addition of chemotherapy to endocrine therapy [30]. The adjuvant chemotherapy used in these trials was CMF and did not include anthracyclines and taxanes. In contrast, a high Ki67 index was predictive of both outcome and benefit to adjuvant taxane chemotherapy in ER-positive breast cancers in subset analyses of the PACS 01 and Breast Cancer International Research Group (BCIRG) 001 trials [31, 32]. An important caveat of these findings is that these were unplanned subset analyses. At this point, Ki67 should not be used as a basis of recommendation for adjuvant chemotherapy outside of a clinical trial setting, at least in part because the test is not always reliable.
A major advancement in the identification of biomarkers of chemosensitivity in HR-positive breast cancers has been the development of multigene prognostic signatures. These are typically derived from high-throughput analyses of tumor specimens for gene expression patterns and subsequently validated in patient cohorts from clinical trials. These assays have the potential to identify subsets of patients that would benefit from the addition of adjuvant chemotherapy to endocrine therapy. The 21-gene assay, called the Oncotype DX (Genomic Health, Redwood City, CA, USA), provides a recurrence score (RS) that predicts for risk of 10-year distant recurrence. The RS is derived from a complex algorithm calculated on the gene expressions of a preselected list of 16 genes of biological interest, including genes involved in estrogen signaling, cell proliferation, and HER2/neu signaling and 5 reference genes for normalization purposes [28]. The utility of the RS as a predictor of distant recurrence risk at 10 years was initially assessed in the NSABP B-14 trial, in which patients with ER-positive, node-negative breast cancer were randomized to receive either tamoxifen or placebo. The RS was shown to more accurately predict for distant recurrence than conventional clinicopathologic characteristics in the tamoxifen-treated patients [33].
The utility of the RS to accurately predict 10-year distance recurrences was demonstrated in a retrospective analysis of the NSABP B-20 trial, in which patients with ER-positive, node-negative breast cancer were randomized to either tamoxifen or tamoxifen plus chemotherapy. Patients with a low or intermediate RS (defined as <18, and ≥18 and <31, respectively) were found not to benefit from chemotherapy, while those with a high RS (defined as ≥31) derived a significant benefit from chemotherapy [28]. The absolute difference in the 10-year distant recurrence rates with the addition of chemotherapy in these RS groups was an increase of 1.1 % and 1.8 % and a reduction of 28.6 %, respectively. Similar results were obtained in a retrospective analysis of the SWOG 8814 trial, in which postmenopausal patients with ER-positive, node-positive breast cancer were randomized to receive either tamoxifen or tamoxifen plus anthracycline-based chemotherapy [26]. One of the primary strengths of this assay is that RNA may be extracted from archived formalin-fixed, paraffin-embedded tissue, which is the primary mode of preserving tissue in most pathology departments.
Another multigene signature with prognostic utility is the FDA-approved 70-gene MammaPrint signature (Agendia, Amsterdam, Netherlands). Unlike the Oncotype RS assay where genes are preselected, MammaPrint was developed using an unsupervised hierarchical clustering approach whereby the high-risk gene signature predicted a poor clinical outcome in tumors of all subtypes [34]. A retrospective analysis of pooled patient cohorts with ER-positive, node-negative breast cancer demonstrated that the 70-gene score had prognostic value and predicted improved survival outcomes with the addition of chemotherapy to endocrine therapy only in the subgroup of 70-gene high-risk patients [35].
While both the Oncotype and MammaPrint assays were tested retrospectively, the Oncotype RS was evaluated retrospectively in a prospectively assembled clinical trial. For this reason, there is far greater confidence, at this time, that the Oncotype assay can reliably predict which patients will benefit from chemotherapy, and even more importantly, which ones will not. In addition, unlike the Oncotype assay, MammaPrint is performed on fresh-frozen tissue that may limit its feasibility for routine use. Both of these multigene signatures are currently undergoing prospective validation in large ongoing studies (Oncotype RS, TAILORx and RxPONDER trials; MammaPrint, MINDACT trial), which include over 100,000 patients collectively to definitively address their predictive value for chemosensitivity in ER-positive breast cancer [36, 37].
In considering the benefits of adjuvant chemotherapy in patients with HR-positive tumors, it is important to consider common relapse patterns. Patients with HR-positive tumors are at a continued risk of relapse for many years after initial breast cancer diagnosis [38]. More than half of all recurrences among women treated with adjuvant tamoxifen therapy occur between 6 and 15 years after diagnosis, and the greatest benefit with the addition of chemotherapy in DFS was seen primarily within the first 5 years from diagnosis [27]. The limited benefit from chemotherapy in preventing late relapses is also reflected in the DFS patterns of patients with poor prognosis multigene signatures with both the Oncotype RS and MammaPrint assays [28, 39]. Late recurrences and deaths remain a formidable clinical challenge in HR-positive breast cancer, and chemotherapy is unlikely to be the answer to this problem.
The summary recommendations for adjuvant chemotherapy in hormone receptor-positive breast cancer are as follows:
Adjuvant chemotherapy should be strongly considered in the setting of node-positive disease, high-grade tumors, and high-risk gene multigene signatures.
In regard to the utility of the Oncotype DX Recurrence Score:
The use of Oncotype for node-positive disease is discouraged in poorer prognosis disease, for example, ≥4 positive nodes, or in the setting of high-grade disease, as chemotherapy should routinely be given in these settings.
The use of chemotherapy is strongly encouraged in patients with Oncotype RS ≥31.
In node-positive patients, particularly those with one to three positive nodes, consideration can be given to omitting chemotherapy if the Oncotype RS is low (<18) and there are no other unfavorable features.
Chemotherapy in HER2-Positive Breast Cancer
The advent of HER2-directed therapy has revolutionized the management of HER2/neu-positive, early-stage breast cancer. Based on the results of five randomized clinical trials, 12 months of adjuvant trastuzumab is now an integral part of systemic therapy for these patients [40–42]. In all studies, trastuzumab was added to a chemotherapy backbone, and there is currently no data to support the use of adjuvant trastuzumab monotherapy. Evidence-based chemotherapy backbones in this context include AC → T (NSABP B-31, NCCTG N9831), AC → docetaxel (BCIRG 006) and docetaxel + carboplatin (BCIRG 006). Given the increased cardiotoxicity risk upon administering trastuzumab concurrently with an anthracycline in the metastatic setting [43], trastuzumab is omitted during the period of anthracycline chemotherapy.
There remains controversy about the treatment of small HER2/neu-positive cancers. There are limited data on outcomes for patients with small, stage I HER2/neu-positive breast cancers because the seminal adjuvant trastuzumab trials excluded patients with these tumors. Current guidelines from St. Gallen and the European Society for Medical Oncology (ESMO) do not recommend adjuvant trastuzumab and chemotherapy for node-negative HER2/neu-positive tumors that are <1 cm [44]. In contrast, the National Comprehensive Cancer Network (NCCN) treatment guidelines have factored in the indirect evidence obtained from retrospective and subset analyses of trials and recommend consideration be given to the use of trastuzumab-based therapy in T1bN0 tumors, in particular, in the hormone receptor-negative subset [45].
However, there is a wide variation in clinical practice in this subgroup. Recently, interest has developed in using less intensive, and therefore potentially less toxic, partner chemotherapies with adjuvant trastuzumab for low-risk HER2-positive tumors. In a phase II study in women with HER2/neu-positive metastatic breast cancer, weekly paclitaxel and trastuzumab resulted in a 67–81 % response rate, and a 6 % incidence of grade 3 or 4 neutropenia [46]. The Dana-Farber Cancer Institute led a multicenter, phase II, nonrandomized study of weekly paclitaxel plus trastuzumab for 12 weeks, followed by maintenance trastuzumab for a further 9 months in patients with node-negative, HER2/neu-positive tumors that are <3 cm (information available at ClinicalTrials.gov; identifier NCT00542451). This trial has completed accrual of 410 patients, of whom approximately 50 % had tumors <1 cm. If the 3-year DFS is >95 %, the regimen will be deemed worthy of further investigation. The results of this trial were reported at the San Antonio Breast Cancer Conference in 2013. There was a high disease free survival rate of 98.7% at a median follow up of 4 years in the population studied, and there were very few adverse events associated with this regimen [47]. In light of these findings, the combination of paclitaxel and trastuzumab should be considered for patients with stage 1 breast cancer.
The adjuvant therapy of HER2/neu-positive breast cancer will be discussed in detail in a separate chapter. The summary recommendations for systemic adjuvant chemotherapy in HER2/neu-positive breast cancer are as follows:
Systemic adjuvant chemotherapy should be given in combination with trastuzumab, especially in tumors >0.5 cm.
Trastuzumab is omitted during the period of anthracycline chemotherapy but can be given concurrently with taxanes.
Consideration of less intensive adjuvant chemotherapy regimens such as paclitaxel plus trastuzumab should be considered for T1N0 HER2/neu-positive breast cancers
Preoperative Chemotherapy (Neoadjuvant)
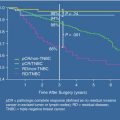
Most early systemic chemotherapy trials for operable breast cancer were conducted in the adjuvant setting, with the use of preoperative (neoadjuvant) chemotherapy limited primarily to inflammatory and locally advanced breast cancer. The original rationale for neoadjuvant chemotherapy (NAC) was to render locally advanced tumors operable by shrinking the diameter of these tumors, thereby reducing the extent of surgery required in operable breast cancer. Studies comparing the adjuvant and NAC approaches have found the survival to be equivalent when using identical systemic agents (Table 23.2). These trials also demonstrated that patients who achieved a pathological complete response (pCR) following NAC had improved clinical outcomes compared to patients who did not.
Table 23.2
Seminal trials comparing neoadjuvant chemotherapy to adjuvant chemotherapy for early-stage breast cancer
Trial | Chemotherapy | pCR rate (%) | pCR vs. non-pCR hazard ratio | Neoadjuvant vs. adjuvant therapy | Reference | ||
|---|---|---|---|---|---|---|---|
BCS rates | DFS HR | OS HR | |||||
NSBAP B-18 | AC × 4 | 13 | OS: 0.32† | 68 % vs. 60 %* | 0.93 | 0.99 | [48] |
EORTC 10902 | FEC60 × 4 | 3.7 | OS: 0.91 | 35 % vs. 22 % | 1.12 | 1.09 | [49] |
ECTO | AP × 4 → CMF × 3 | 20 | RFS: 0.43† | 65 % vs. 34 %* | 1.21 | 1.10 | [50] |
The NAC and adjuvant chemotherapy regimens used clinically are identical. The NAC approach is now increasingly used in smaller, operable TNBC and HER2/neu-positive tumors, although less commonly with HR-positive tumors as they are inherently less chemosensitive [4, 51]. There has also been a trend by many clinicians to evaluate novel therapies in the preoperative setting. A NAC approach allows for the study of the biological impact of systemic therapy on pre- and posttreatment tissue and therefore represents a fertile setting for tissue-intensive correlative research. The goal of biomarker discovery in NAC clinical trials is to identify surrogate end points of clinical outcomes, such as predictive biomarkers of therapeutic response or resistance. The US Food and Drug Administration (FDA) is considering the possibility of using pCR in the NAC setting as a surrogate end point for clinical benefit and as an indication for accelerated drug approval [52].
Practically, NAC should be managed only in a multidisciplinary team setting, with initial assessments made by the breast surgeon and medical and radiation oncologists. Evaluation of treatment response to NAC could potentially allow the treating team to tailor individual treatment based upon tumor response, particularly if there is the suggestion of disease progression. There have been two trials in which patients were randomized mid-treatment to non-cross-resistant chemotherapy regimens according to their mid-treatment response [53, 54]. In both trials, deviating from the initial course of therapy in clinical nonresponders did not increase either the clinical or pathological response rates or improve survival. For operable breast cancer, in the event of disease progression mid-NAC, we would recommend an immediate reevaluation by the breast surgeon in order to assess the feasibility of surgical resection with mastectomy. Decisions about additional chemotherapy can be deferred until the adjuvant setting. For patients with non-resectable disease, radiation or alternative investigational approaches should be considered [55].
Special Clinical Scenarios
Inflammatory and Locally Advanced Breast Cancer
Inflammatory breast cancer (IBC) represents a unique biological entity characterized by distinct clinical and histopathological features, aggressive behavior, and an exceptionally poor prognosis (median survival with current therapy <4 years) [56]. The current standard of care for management of stage 3B IBC is a multimodality approach consisting of NAC followed by surgery and radiotherapy. Achieving a pCR to NAC is the single most important prognostic factor in IBC [57, 58].
Given the relative rarity of IBC, there have been no specific randomized trials examining the optimal NAC regimen, and moreover patients with IBC have historically been excluded from NAC systemic therapy studies due to their poor prognosis. Single-arm studies and retrospective case series show that anthracycline-based regimens are effective (clinical response rates around 70 %) [57] and that their efficacy is enhanced by the subsequent addition of a taxane as evidenced by increased clinical and pCR rates [59, 60]. As such, regimens included in the “Anthracycline and Taxane” section of Table 23.1 are recommended.
Although outside the scope of this chapter, it is noteworthy that approximately 40 % of IBC are HER2/neu positive, and evidence from randomized phase 3 clinical trials strongly supports the routine addition of trastuzumab to NAC in this setting [61].
Elderly Patients
Although the incidence of breast cancer rises sharply with age, there is a lack of quality data discussing the optimal choices regarding adjuvant chemotherapy in the elderly. This is particularly true for patients with advanced comorbidities and frailty, who are generally excluded from phase 3 clinical trials. For this reason, groups such as the International Society of Geriatric Oncology (SIOG) and European Society of Breast Cancer Specialists (EUSOMA) have developed consensus guidelines specific to the issues facing elderly patients with breast cancer [62]. Compared to their younger counterparts, elderly patients are more likely to present with larger primary tumors and positive lymph nodes [63], at least in part attributable to greater delays in initial diagnosis. Breast cancers in the elderly are also more frequently HR positive [64].
Prescribing adjuvant chemotherapy to elderly patients require several unique considerations. First, elderly patients often suffer comorbid illnesses that provide competing mortality risks. As such, determining the potential overall survival gains from adjuvant chemotherapy for an individual patient is more challenging. Groups such as the Cancer and Leukemia Group B (CALGB) have developed tools for pre-chemotherapy geriatric assessment to help address this problem [65]. It is also important to note that despite competing risks, >40 % of patients diagnosed with breast cancer after the age of 80 will die from breast cancer [66].
Second, elderly patients may be more susceptible to certain chemotherapy toxicities. Although there is no evidence to support modifying chemotherapy doses because of age, strict monitoring of renal and hepatic function during treatment is essential. Furthermore, routine assessment of left ventricular ejection fraction is recommended for patients scheduled to receive anthracyclines. Thirdly, data suggests that elderly patients are more likely to experience difficulties with medication compliance [63], particularly oral medications such as antiemetics. It is thus critical to ensure that patients with any degree of cognitive impairment clearly understand their drug regimens and are adequately educated and supervised if necessary.
There is little prospectively collected, randomized trial data to suggest a particular adjuvant chemotherapy regimen for elderly patients beyond the general standards of care. In general terms, adjuvant chemotherapy is feasible in patients over 65–70 years of age, but increasing age, reduced functional status, and presence of comorbidities are associated with more frequent dose reductions and/or delays [67]. A landmark CALGB study compared standard chemotherapy regimens (either AC or CMF) to oral capecitabine in patients >65 years of age with early-stage breast cancer [68]. The study was stopped early after an interim analysis suggested that the capecitabine regimen was inferior, resulting in an almost doubled risk of recurrence or death. This study reinforces the efficacy of standard chemotherapy in an elderly population. Nonrandomized data also suggest tolerability of the TC regimen patients >65 years [69], although elderly patients do seem more prone to taxane-induced hematological toxicities [70].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree