Number of patients
DFS/RFS HR (95 %CI or p value)
OS
Cardiotoxicity
Comments
NSABP B31/N9831 [35]
5,548
0.60 (0.53–0.68)
0.63 (0.54–0.73)
4.1 %
The N9831 also included a sequential trastuzumab arm. Data showed that the sequential arm was inferior to the concomitant arm
HERA [37]
5,102
0.76 (p < 0.0001)
0.76 (p = 0.0005)
4.1 %
The study also showed that there was no difference between 1 year and 2 years of trastuzumab
BCIRG 006 [12]
3,222
AC-DH: 0.64 (p < 0.001)
AC-DH: 0.63 (p < 0.001)
AC-DH: 2 %
Although the study was not powered to
DCarboH: 0.4 %
DCarboH: 0.75 (p = 0.04)
DCarboH: 0.77 (p = 0.04)
compare the two trastuzumab arms, there was no statistical difference between them
FINher [39]
232
0.42 (0.21–0.83)
0.41 (0.16–1.05)
No decrease
This trial included 12 weeks of trastuzumab therapy
PACS 04 [38]
528
0.86 (0.61–1.22)
0.86 (0.61–1.22)
1.7 %
The only adjuvant trial to not show a significant benefit from 1 year of trastuzumab therapy. This could be attributed to the relatively small number of patients it included
PHARE [40]
3,381
1.28 (1.05–1.56)
NA
NA
This trial showed that 6 months of trastuzumab was not non-inferior to 12 months
NSABP B31 and NCCTG 9831 Joint Analysis
Since trastuzumab was effective in improving RR, duration of response, and OS in MBC, large randomized adjuvant trials were initiated [11, 12]. These trials showed that the integration of trastuzumab into adjuvant therapy regimens significantly improved patient outcomes and led to the FDA approval of trastuzumab for HER2+ early-stage breast cancer. The National Surgical Adjuvant Breast and Bowel Project (NSABP)-B31 published a joint analysis with the North Central Cancer Treatment Group (NCCTG) N9831 [11]. These trials were closed prematurely due to the superiority of the trastuzumab arm. The B31 trial enrolled 2,043 node-positive, HER2+ patients with early-stage breast cancer and randomized them to 4 cycles of doxorubicin (A) and cyclophosphamide (C) (A = 60 mg/m2 and C = 600 mg/m2, q 21 days) followed by paclitaxel (T = 125 mg/m2) given every 3 weeks for 4 cycles (Group 1) or the same chemotherapy with weekly trastuzumab (H = 4 mg/kg loading dose, than 2 mg/kg weekly) for 52 weeks starting with the paclitaxel (Group 2). The protocol was later amended to allow weekly paclitaxel similar to the N9831 trial.
The N9831 trial randomized 3,505 HER2+ (IHC 3+ or HER2 amplified by FISH), axillary node-positive (the protocol was amended at a later point to include high-risk node-negative (tumor size greater than 2 cm ER + or >1 cm if ER-)) patients into three groups: The control group, Group A, received 4 cycles of AC followed by weekly T (80 mg/m2) for 12 weeks; Group B received 4 cycles of AC followed by 12 weekly doses of T followed by sequential weekly trastuzumab for 52 weeks; and Group C received 4 cycles of AC, followed by 12 weekly doses of T concomitantly with weekly trastuzumab which would be continued for 40 more weeks after completion of paclitaxel. The combined analysis grouped the control groups (Group 1 and Group A from B31 and N9831, respectively) and compared them to Group 2 and Group C from B31 and N9831, respectively. Since there was no group in the B31 trial that evaluated sequential trastuzumab, N9831’s Group B was not included in the combined analysis.
Patients in both studies were excluded if they had any history of coronary disease, arrhythmias, cardiomegaly, CHF, or cardiomyopathy or required medications for angina pectoris or valvular heart disease. Furthermore, in order to ascertain any compromise in left ventricular ejection fraction (LVEF), multiple-gated acquisition scanning (MUGA) and echocardiography were obtained (B31 used MUGA scanning only) at treatment initiation and every 3 months until completion of the treatment.
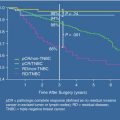
Both trials were terminated early by the independent data-monitoring committee based on the significant benefits trastuzumab added compared to the control arm of chemotherapy. The primary endpoint, DFS, was reached, and at a median follow-up of 2 years, there was a statistically significant reduction in recurrence of 52 % (p < 0.0001) with an absolute distant recurrence in the trastuzumab-containing arm at 3 and 4 years of 8.8 % and 15.9 %, respectively. The OS was improved by a third (HR, 0.67, p = 0.015). The absolute survival difference was 2.5 % (94.3 % versus 91.7 %) at 3 years and 4.8 % (91.4 % versus 86.6 %) at 4 years. Interestingly, brain metastases were more commonly seen as a first site of recurrence in the trastuzumab-treated group compared to the control. Possible explanations for the latter observation include delayed failures at local sites compared to distant sites and the limitation that trastuzumab has in crossing the blood-brain barrier [32, 33].
The incidence of symptomatic CHF (New York Heart Association [NYHA] class III or IV) or other cardiac-related deaths at 3 years in the B31 study was 0.8 % in the control group compared to 4.1 % in the trastuzumab-treated group. Additionally, 14 % of trastuzumab-treated patients had to discontinue therapy secondary to asymptomatic decreases in LVEF, whereas 4 % stopped secondary to symptomatic cardiotoxicity [11]. In the N9831 trial, the 3-year cumulative incidence of NYHA class III or class IV CHF was 2.9 % in the trastuzumab-treated group compared to 0 % in the control group. Interestingly, interstitial pneumonitis, albeit rare, occurred more commonly in the trastuzumab-treated group compared with the control. Patients with stage I–IIA breast cancer who required radiation therapy did not have any increase incidence of radiation adverse events when radiation was given concurrently with trastuzumab [11]. The combined analysis revealed the significant benefit in the reduction of recurrence and death. An unplanned interim analysis revealed that concurrent use of trastuzumab with paclitaxel was more effective than sequential use in both DFS and OS [34].
These two trials were recently updated for a final analysis [35]. At a median follow-up of 8.4 years, DFS was 73.7 % in the trastuzumab arm compared with 62.2 % in the chemotherapy arm (HR, 0.60; p < 0.0001). The OS was again significantly better in the trastuzumab arm (84.0 % versus 75.2 % respectively; HR, 0.63; p < 0.0001), with the survival benefit noted to be of similar magnitude in the ER + and the ER– subgroup of patients.
Herceptin Adjuvant (HERA) Trial
Another large, phase III international, multicenter trial, the HERA trial, conducted by the Breast International Group (BIG), sequenced trastuzumab after primary surgery and after a minimum of 4 cycles of adjuvant or neoadjuvant chemotherapy [36]. A total of 5,102 HER2+ patients with early-stage breast cancer were randomized, to receive trastuzumab for 1 or 2 years versus observation alone. If randomized to receive trastuzumab, patients received an initial dose of 8 mg/kg followed by maintenance doses of 6 mg/kg every 3 weeks for either 1 or 2 years. All eligible patients were required to have node-positive disease or, if node negative, a tumor diameter of >1 cm. Cardiac monitoring via MUGA or ECHO was done at baseline and 3, 6, 12, 18, 24, 30, 36, and 60 months after randomization. Trastuzumab was stopped in any patient with LVEF ≤45 % or who developed a 10 % absolute decrease in their baseline LVEF and below 50 %. Trastuzumab was permanently discontinued if the LVEF did not return to above LLN within 3 weeks.
At a median follow-up of 8 years and 734 DFS events, the final analysis was recently presented [37]. This analysis was complicated by the fact that 885 of the 1698 patients assigned to the observation group elected to cross over to trastuzumab after the initial results of the trial were presented. However, in the intention-to-treat analysis, there was a significant risk reduction of 24 % (HR, 0.76; p < 0.0001) in DFS and an identical reduction in OS (HR, 0.76; p = 0.0005). The benefit of 1 year of trastuzumab was seen in both HR + and HR– patients.
An analysis comparing both trastuzumab arms did not show any additional benefit with 2 years of trastuzumab compared with 1 year. The DFS in the 2-year arm was 75.8 % compared with 76.0 % in the 1-year arm (HR, 0.99; p = 0.86). The lack of benefit was seen in both the HR + and HR– subgroups. Similarly there was no benefit in OS (86.4 % in the 2 year arm versus 87.6 % in the 1 year arm; HR, 1.05; p = 0.63).
The incidence of cardiac toxicity was increased with the use of trastuzumab and was even higher in the 2-year arm. More specifically, the incidence of a significant decrease in the ejection fraction (EF) was 0.9 % in the observation arm, 4.1 % in the 1-year trastuzumab arm, and 7.2 % in the 2-year trastuzumab arm.
The HERA trial evaluated the use of sequential trastuzumab in order to circumvent added cardiotoxicity of combining anthracycline with trastuzumab as well as to determine the optimal duration of trastuzumab therapy. Sequential therapy appears to improve DFS by 24 %. Cardiotoxicity was lower than seen in the joint analysis [11, 36]. There are multiple reasons for the lower incidence of cardiotoxicity including more frequent monitoring, different modalities of monitoring, sequential therapy, as well as fewer patients exposed to anthracycline therapy. The results of the HERA trial clearly confirm the benefit of trastuzumab in patients with HER2+ early-stage breast cancer and demonstrate that durations of trastuzumab beyond 1 year confer no additional clinical benefit.
Breast Cancer International Research Group (BCIRG) 006
The BCIRG initiated a phase III, multicenter trial to evaluate the adjuvant use of trastuzumab concurrently with a non-anthracycline chemotherapy regimen after multiple phase II trials confirmed the feasibility of this approach [12]. The BCIRG 006 is a randomized trial of 3,222 HER2+ patients (FISH only) with axillary lymph node-positive or high-risk lymph node-negative (tumor size >2 cm, ER/PR negative, histologic and/or nuclear grade 2–3, or age <35) breast cancer. The two arms were randomized to adjuvant AC followed by docetaxel (D, 100 mg/m2 q 21 days for 4 cycles) with or without trastuzumab (H, weekly during chemotherapy and then every 21 days), while the third arm included docetaxel and carboplatin (DCarbo) (D, 75 mg/m2; Carbo (AUC of 6 every 3 weeks × 6) with H for 1 year). At a median follow-up of 65 months, the DFS was 75 % in the patients receiving AC-D, 84 % in the patient receiving AC-DH (HR, 0.64; p < 0.001), and 81 % in patients receiving DCarboH (HR, 0.75; p = 0.04). OS was 87 %, 92 % (HR, 0.63; p < 0.001), and 91 % (HR, 0.77; p = 0.04), respectively. Although there was no statistically significant difference between either trastuzumab arms, the study was not powered to detect equivalence between these two regimens.
The BCIRG 006 results were similar to the combined analysis in highlighting the benefit from adjuvant trastuzumab [11], showing that non-anthracycline chemotherapy given concurrently with trastuzumab was effective [12]. The incidence of CHF in the two trastuzumab-containing regimens was higher in the group receiving AC-DH (2.0 %) than in the AC-D group (0.7 %) or the TCH group (0.4 %). The difference in rates of CHF between the two trastuzumab-containing regimens significantly favored DCarboH over AC-D plus trastuzumab (p < 0.001). There was no significant difference in the incidence of leukemia between arms with six cases seen in the AC-D arm and one each for AC-DH and DCarboH.
PACS-04 Trial
This trial evaluated the role of trastuzumab in women with early-stage, HER2+, lymph node-positive breast cancer [38]. A total of 528 patients were randomized to trastuzumab or observation. This trial had a second randomization to chemotherapy with FEC100 for 6 cycles versus epirubicin (75 mg/m2) and docetaxel (75 mg/m2) for 6 cycles. The primary endpoint of the trial was DFS. Trastuzumab started after chemotherapy and radiation therapy. At 47 months of median follow-up, patients on the trastuzumab arm had a nonsignificant 14 % reduction in the risk of relapse (HR, 0.86; p = 0.41), with no significant difference in OS (HR, 1.27). The incidence of CHF was low (1.7 %) in the trastuzumab arm, and the two regimens overall were well tolerated. Although this is the only reported trial that does not show a benefit from adjuvant trastuzumab, the number of patients included is smaller than the other trials and the sequencing of chemotherapy and trastuzumab may be another plausible explanation for the lack of benefit.
FINher Trial
The FINher (FINl and Herceptin) trial examined whether an abbreviated course of trastuzumab was effective [39]. The FINher trial included patients with early-stage breast cancer (axillary node positive or tumor >2 cm with negative axillary nodes and negative PR). A total of 232 HER2+ patients were randomized to receive either adjuvant docetaxel (100 mg/m2) every 3 weeks for 3 cycles or vinorelbine on days 1, 8, and 15 of 21-day cycle for 3 cycles with or without concurrent weekly trastuzumab (4 mg/kg loading dose, then 2 mg/kg weekly) for 9 weeks. All patients then received fluorouracil (600 mg/m2), epirubicin (60 mg/m2), and cyclophosphamide (600 mg/m2) (FEC, q 21 days for 18 weeks for 6 cycles after their initial therapy). After a median follow-up of 3 years, HER2+ patients treated with trastuzumab had a significantly improved relapse-free survival (RFS) (HR, 0.42; p = 0.01) and decreased distant recurrence (HR, 0.29; p = 0.002) compared to HER2+ patients treated without trastuzumab therapy.
Moreover, a nonsignificant improvement in OS was seen in the trastuzumab-treated arm (HR, 0.41; p = 0.07). The HR for recurrence in HER2-amplified, trastuzumab-treated patients did not significantly change with the type of chemotherapy, the number of lymph nodes involved, or the center providing the therapy. The HER2+ patients treated with trastuzumab had a similar survival free of distant DFS at 3 years compared with HER2-negative patients (HR, 1.09; 95 % CI 0.52–2.29; p = 0.82). As expected, HER2+ patients treated without trastuzumab did worse than HER2-negative patients. There was no decline in LVEF in HER2+ patients treated with 9 weeks of trastuzumab. The short course of trastuzumab therapy was effective in this small sample size and raises the possibility that shorter durations of trastuzumab therapy may ultimately prove as effective, and possibly safer, than a standard 1 year regimen.
Protocol of Herceptin Adjuvant with Reduced Exposure (PHARE) Trial
The goal of the PHARE trial was to evaluate the efficacy of 6 months of adjuvant trastuzumab compared with 1 year of therapy [40]. Patients had to have operable, nonmetastatic HER2+ breast cancer and a ≥1 cm tumor and had received at least four cycles of adjuvant chemotherapy for their breast cancer. After the completion of 6 months of adjuvant trastuzumab, eligible patients were randomized to either stop therapy or continue for a total of 1 year. This trial had a non-inferiority design, and a total of 3,381 patients were randomized. In 2010, the trial was suspended after the data-monitoring committee concluded that the 6-month arm had a trend of more DFS events when compared to the 1-year arm. Although this difference was not statistically significant (HR, 1.28; p = 0.29), there was a trend showing that the 6-month arm was inferior to the 1-year arm. When analyzing patients according to tumor types, there was a significant difference in the ER- patients favoring the 1-year trastuzumab arm (HR, 1.34; p = 0.037), whereas there was no significant difference in the ER + patients. These results failed to show that 6 months of trastuzumab is non-inferior to 12 months. Other clinical trials are under way, but until further data is available, the results from the PHARE trial viewed in combination with the HERA trial suggest that the optimal duration of therapy with trastuzumab remains at 1 year.
Neoadjuvant Clinical Trials with Trastuzumab
Baselga et al. reported the results of the NeoALTTO trial, conducted by the Breast International Group [41]. This was an open-label, phase 3 trial in which 455 patients with HER2+, early-stage breast cancer (tumors >2 cm) were randomly assigned to oral lapatinib (1500 mg daily), intravenous trastuzumab (standard dose), or a combination of both agents (lapatinib 1000 mg/day plus standard trastuzumab dosing). Lapatinib is an oral, dual HER2 and EGFR tyrosine kinase inhibitor (TKI) which has demonstrated preclinical and clinical activity in HER2+ breast cancer [42–45]. The anti-HER2 therapy was administered alone for the first 6 weeks at which point weekly paclitaxel was added to the assigned anti-HER2 therapy for an additional 12 weeks followed by definitive surgery.
Following surgery, patients received adjuvant therapy along with the same anti-HER2 therapy as assigned preoperatively for a total of 52 weeks of anti-HER2 therapy. The primary endpoint of the study was the pathologic complete response (pCR) rate in the breast. The pCR rate was significantly higher in the group of patients receiving both lapatinib and trastuzumab (51.3 %) versus trastuzumab alone (29.5 %) or lapatinib alone (24.7 %). Additionally, the difference between trastuzumab alone and lapatinib alone was statistically significant, in favor of trastuzumab. Although there was no difference in cardiac events between the treatment arms, the use of lapatinib alone or in combination with trastuzumab was associated with greater frequency of grade 3 diarrhea and liver enzyme abnormalities than those receiving trastuzumab alone. This study suggests that dual HER2 therapy was superior to either anti-HER2 therapy alone, yet trastuzumab was superior to lapatinib as a monotherapy approach.
The GeparQuinto GBG 44, a German Breast Group study, is a phase 3 trial in which 620 patients with HER2+ operable, or locally advanced, breast cancer were randomized to receive neoadjuvant treatment with 4 cycles of epirubicin/cyclophosphamide (EC), every 3 weeks, followed by 4 cycles of docetaxel (T), every 3 weeks, with either concurrent, standard dose, trastuzumab (H) or lapatinib (L) [46]. The primary endpoint of the study was pCR in both the breast and axillary lymph nodes at the time of surgery. The pCR rate for those patients receiving chemotherapy plus H was 30.3 % versus 22.7 % for those receiving chemotherapy plus L (HR, 0.68, p = 0.04). There was a greater incidence of dyspnea and edema in patients receiving chemotherapy/trastuzumab, while patients receiving chemotherapy/L had a greater incidence of skin rash and diarrhea. A total of 33.1 % of patients receiving chemotherapy/L discontinued treatment due to toxicity compared with 14 % of patients receiving chemotherapy/H.
Another neoadjuvant clinical trial performed by the MD Anderson group incorporated trastuzumab to an epirubicin-based regimen [47]. A total of 64 patients were included in the trial which was conducted in two phases. Patients were randomized to receive 4 cycles of paclitaxel at 225 mg/m2 as a 24-h infusion at 3-week intervals, followed by 4 cycles of FEC therapy, which consisted of 500 mg/m2 fluorouracil on days 1 and 4, 500 mg/m2 i.v. cyclophosphamide on day 1 only, and 75 mg/m2 epirubicin on day 1 only. Patients randomized to receive trastuzumab received 4 mg/kg trastuzumab i.v. over 90 min on day 1 of the first cycle of paclitaxel. These patients received 2 mg/kg trastuzumab weekly, administered i.v. over 30 min during the 24 weeks of chemotherapy. pCR for patients receiving trastuzumab was 60 % and 26.3 % in the non-trastuzumab group. Cardiac safety data suggested that even though trastuzumab was given concurrently with epirubicin, there was no cardiac dysfunction. This study is relatively small compared with other neoadjuvant and adjuvant clinical trials. However, the efficacy of the trastuzumab arm and apparent lack of cardiac toxicity provide good preliminary data for using this combination in the clinical setting.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree