Adenocarcinoma
Philip T. Cagle
Keith M. Kerr
Adenocarcinomas are defined as carcinomas with gland formation and/or mucin production. Adenocarcinomas are the most frequently occurring cell type of pulmonary carcinoma in the industrialized world, replacing squamous cell carcinomas over the past several decades in North America and Western Europe, possibly because of alterations in smoking exposure caused by modifications in cigarettes, including the use of filters (see Chapter 27). In the 1950s, adenocarcinomas accounted for as few as 5% of lung cancers, but currently adenocarcinomas account for 35% to 50% of lung cancers in most series.1,2,3,4,5,6,7,8,9 and 10 Adenocarcinomas have long been the most frequent cell type in Asian countries. In the past, adenocarcinomas were more frequent in women than in men in North America and Europe, but the general increase in the frequency of adenocarcinoma has been associated with a major shift in cell types in men, so that today adenocarcinoma is the most frequent cell type in both sexes. Although most adenocarcinomas are caused by tobacco smoking, adenocarcinoma is the most frequent cell type in patients who have never smoked.11,12,13,14,15,16 and 17
In this chapter, we review the histopathology of pulmonary adenocarcinoma based on the current 2004 World Health Organization (WHO) classification. Revisions to the current classification are being proposed and these are discussed in Chapter 5. The 2004 WHO classification divides pulmonary adenocarcinomas into acinar, papillary, bronchioloalveolar, solid adenocarcinomas with mucin production, and mixed subtypes and includes several variants (fetal adenocarcinoma, mucinous or colloid carcinoma, mucinous cystadenocarcinoma, signet ring adenocarcinoma, and clear cell carcinoma).18 Since bronchioloalveolar carcinoma is distinct from other forms of adenocarcinoma and by definition is carcinoma-in-situ, which introduces unique issues, it is discussed separately in Chapter 4.19,20 As mentioned above, there are a number of concerns with the 2004 WHO classification and revisions are being proposed, including recognition that most adenocarcinomas have mixed histologic patterns and should be classified according to their predominant subtype,21,22,23,24,25,26 and 27 replacing the term bronchioloalveolar carcinoma with adenocarcinoma-in-situ10 and differentiating adenocarcinoma from squamous cell carcinoma whenever possible, minimizing the use of the term non-small cell carcinoma. These and other proposed revisions are discussed in Chapter 5.
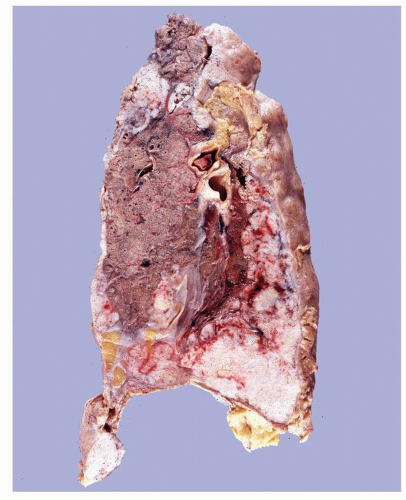
ADENOCARCINOMA, GROSS FEATURES
Most pulmonary adenocarcinomas are peripheral in location, and most peripheral primary carcinomas of the lung are adenocarcinomas, although pulmonary adenocarcinomas may be central in location. Due to their peripheral location, adenocarcinomas may be discovered as an incidental mass, nodule, or “coin lesion” on imaging studies performed for other reasons and may not present with clinical symptoms (Fig. 3-1). Typically, they are gray-white, firm, lobulated masses, often with central scarring and anthracotic pigment (Fig. 3-2). In some cases, part or all of the peripheral margin of the tumor is ill-defined. Subpleural tumors may be associated with pleural puckering (Figs. 3-3 and 3-4). As noted, central desmoplastic reaction, or scar, is common and necrosis may be present, but cavitation is unusual. Not surprisingly, because of their location, adenocarcinomas are the most likely cell type to invade the pleura and extend onto the pleural surface.18,21,22,23 and 24
 FIGURE 3-1 Chest x-ray shows peripheral mass in the right upper lung zone. This mass was diagnosed as a pulmonary adenocarcinoma. (Courtesy of Ronald E. Fisher, M.D., Ph.D.) |
 FIGURE 3-2 Lobectomy specimen containing a bisected subpleural adenocarcinoma. The cut surface of the tumor displays a lobulated firm mass with central scarring and anthracotic pigment. |
 FIGURE 3-3 Pleural surface of lobectomy specimen shows “puckered” pleura with a central depression from a scar associated with a subpleural tumor mass. |
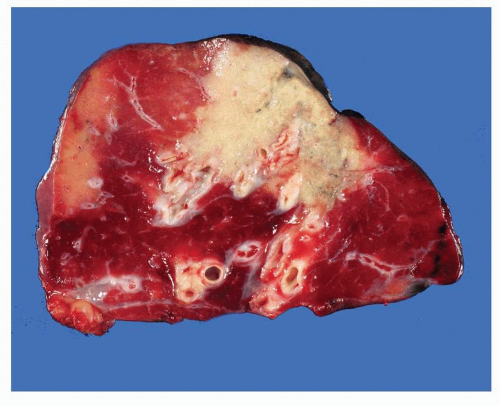 FIGURE 3-4 Cut surface of same specimen as in Figure 3-3 shows subpleural adenocarcinoma with scar causing puckering of overlying pleura. |
The so-called “scar cancers” of the lung were once thought to be adenocarcinomas that arose from a preexisting scar, for example, from a focus of tuberculosis or healed pneumonia. It is now recognized that the vast majority of these tumors are adenocarcinomas with central desmoplastic reaction and the cancer has preceded the “scar” and not vice versa.28,29 and 30 Rarely, carcinomas may grow predominantly on the pleural surface and encase the lung in a gross pattern similar to diffuse malignant mesothelioma and are referred to as “pseudomesotheliomatous carcinomas.” The majority of carcinomas that grow in this “pseudomesotheliomatous” pattern arise as primary subpleural adenocarcinomas of the lung (Fig. 3-5).31,32 and 33
ADENOCARCINOMA, HISTOLOGY
The current WHO classification of pulmonary adenocarcinomas includes several major subtypes: acinar, papillary, bronchioloalveolar, solid adenocarcinoma with mucin production, and mixed. If sampled adequately, virtually all pulmonary adenocarcinomas are of mixed subtype, although one subtype usually predominates.18,21,22,23,24,25,26 and 27 It has been proposed that this long-standing observation should be addressed in a new classification system (see Chapter 5).10
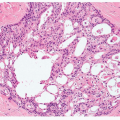
The acinar pattern consists of formation of glands or tubules with malignant epithelial cells lining the central lumens of various shapes, sizes, and complexity ( Figs. 3-6,3-7 and 3-8). The solid pattern consists of sheets or nests of large, polygonal cells with vesicular nuclei, prominent nucleoli, and comparatively abundant eosinophilic cytoplasm (Figs. 3-9 and 3-10). Intracytoplasmic mucin can be demonstrated with periodic acid Schiff with diastase, mucicarmine, and/or Alcian blue stains (Figs. 3-11 and 3-12). Current WHO criteria recommend at least five mucin positive cells in each of two high power fields for classification as a solid adenocarcinoma with mucin. Papillary adenocarcinomas consist of malignant epithelial cells lining the fibrovascular cores or papillae (Figs. 3-13 and 3-14). In contrast to the simple epithelial tufts seen in some bronchioloalveolar carcinomas, papillary adenocarcinomas have secondary and tertiary papillary structures that obliterate the underlying lung architecture. A distinctive type of pulmonary adenocarcinoma
is micropapillary adenocarcinoma. These tumors have simple papillary structures without fibrovascular cores and are associated with an unfavorable prognosis (Figs. 3-15 and 3-16).18,21,22,23,24 and 25,34 It has been proposed that “micropapillary pattern, predominant” be recognized as a subtype under “invasive adenocarcinoma” distinct from “papillary pattern, predominant” (see Chapter 5).10
is micropapillary adenocarcinoma. These tumors have simple papillary structures without fibrovascular cores and are associated with an unfavorable prognosis (Figs. 3-15 and 3-16).18,21,22,23,24 and 25,34 It has been proposed that “micropapillary pattern, predominant” be recognized as a subtype under “invasive adenocarcinoma” distinct from “papillary pattern, predominant” (see Chapter 5).10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree