TYPES OF OSTEOMALACIA
Part of “CHAPTER 63 – OSTEOMALACIA AND RICKETS“
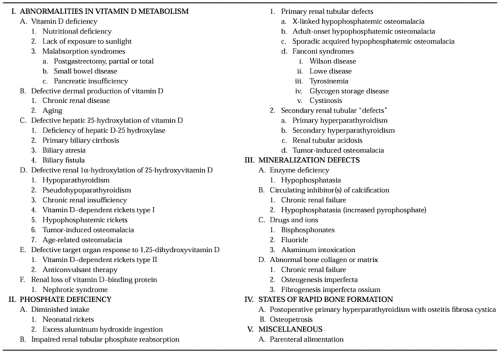
Osteomalacia can result from abnormalities in vitamin D metabolism, phosphate deficiency, various mineralization defects, and states of rapid bone formation (Table 63-1; see Chap. 70).
NUTRITIONAL DEFICIENCY
Normally, vitamin D3 derived by dermal production from 7-dehydrocholesterol is the major source of the vitamin (see Chap. 54). Because exposure to sunlight is adequate and dairy products are fortified with vitamin D, osteomalacia resulting from nutritional deficiency is rarely seen in the United States. When it does occur, lack of exposure to sunlight usually is responsible. Conversely, nutritional deficiency of vitamin D is more common in other parts of the world. In the United Kingdom, osteomalacia occurs in immigrant Indians and Paki-stanis.16,17 and 18 Ethnic traditions and dietary patterns contribute to the development of osteomalacia in the Asian population in England. Endogenous production of vitamin D3 is limited in women who remain indoors and wear traditional clothing, because of diminished exposure to the sun. Chupatti flour, a dietary staple of these population groups, has a high phytate content in the wheat and binds calcium, causing increased fecal excretion. Lignin, a component of wheat fiber, binds to bile acids, preventing their absorption.19 Vitamin D, which normally forms micelles with bile acids, a requirement for its absorption by the intestine, may be bound by the lignin-bile acid complex instead and not be absorbed. Removal of the chupatti flour from the diet corrects abnormal vitamin D and mineral metabolism. In addition, fortification of the diet with vitamin D can correct the deficiency.
In the United States and other countries, rickets occurs in newborns who are breast-fed because the content of vitamin D
and 25-hydroxyvitamin D [25(OH)D] in human milk is not adequate.20 In the northern hemisphere, blacks, Pakistanis, and Asian Indian infants are particularly at risk for rickets because maternal serum vitamin D and 25(OH)D values are low as a consequence of increased skin pigmentation and diminished dermal synthesis of vitamin D. Asian Indians and Pakistanis, but not blacks, are at risk for vitamin D deficiency and osteomalacia in later life.21 However, osteomalacia caused by nutritional vitamin D deficiency does not occur in blacks. In developed countries, osteomalacia occurs in the elderly, who appear to be the population at greatest risk for this disorder. This is especially true for individuals who are housebound or institutionalized. An age-related decline in the dermal synthesis of 7-dehydrocholesterol,22 inadequate intake of vitamin D, and impaired production of 25(OH)D in the liver and 1,25-dihydroxyvitamin D [1,25(OH)2D] in the kidney23 also may be contributing factors.
and 25-hydroxyvitamin D [25(OH)D] in human milk is not adequate.20 In the northern hemisphere, blacks, Pakistanis, and Asian Indian infants are particularly at risk for rickets because maternal serum vitamin D and 25(OH)D values are low as a consequence of increased skin pigmentation and diminished dermal synthesis of vitamin D. Asian Indians and Pakistanis, but not blacks, are at risk for vitamin D deficiency and osteomalacia in later life.21 However, osteomalacia caused by nutritional vitamin D deficiency does not occur in blacks. In developed countries, osteomalacia occurs in the elderly, who appear to be the population at greatest risk for this disorder. This is especially true for individuals who are housebound or institutionalized. An age-related decline in the dermal synthesis of 7-dehydrocholesterol,22 inadequate intake of vitamin D, and impaired production of 25(OH)D in the liver and 1,25-dihydroxyvitamin D [1,25(OH)2D] in the kidney23 also may be contributing factors.
VITAMIN D-25-HYDROXYLASE DEFICIENCY
Rarely, rickets occurs as a consequence of deficiency of vitamin D-25-hydroxylase.24,25 The disease apparently is transmitted genetically as an autosomal recessive trait. Affected children show evidence of rickets during early childhood. Clinical findings include irritability, seizures, growth retardation, and poor motor development. Hypocalcemia of variable degree, hypophosphatemia, elevated serum alkaline phosphatase and serum immunoreactive PTH (iPTH) values, low serum 25(OH)D values, and normal or elevated serum levels of 1,25 dihydroxyvitamin D [1,25(OH)2D] are found. The diagnosis is made as follows: demonstration of a low serum 25(OH)D value; poor response to physiologic doses of vitamin D; correction of biochemical, clinical, and radiographic changes of rickets after treatment with physiologic doses of 25(OH)D; the lack of hepatic, gastrointestinal, or renal disease; and no history of consumption of anticonvulsants.
GASTROINTESTINAL AND HEPATIC DISEASES
Intestinal malabsorption associated with diseases of the small intestine, hepatobiliary tree, and pancreas is the most common cause of vitamin D deficiency in the United States.26 Disorders of the small intestine that may cause malabsorption and osteomalacia include celiac disease or sprue, regional enteritis, scle-roderma, multiple jejunal diverticula, and the blind loop syndrome. In some cases, the bone disease is more evident than the gastrointestinal disease. Impaired absorption of calcium as well as vitamin D may contribute to the development of osteomalacia. Although vitamin D undergoes an enterohepatic circulation, intestinal loss of endogenous vitamin D has not been demonstrated to be important in the pathogenesis of osteomalacia in enteric diseases.
In adults, osteomalacia is a common complication of intestinal bypass surgery for the treatment of morbid obesity. In these patients, histologic changes of osteomalacia are more common than are radiographic changes.27
Osteomalacia is a complication of partial gastrectomy, especially in association with the Billroth II operation, which excludes
the duodenum.28 Deficient intake of vitamin D, postgastrectomy steatorrhea, and diminished exposure to sunlight and calcium absorption are contributing factors. The incidence of postgastrectomy osteomalacia will probably decline with the advent of more effective medical treatment of peptic ulcer disease.
the duodenum.28 Deficient intake of vitamin D, postgastrectomy steatorrhea, and diminished exposure to sunlight and calcium absorption are contributing factors. The incidence of postgastrectomy osteomalacia will probably decline with the advent of more effective medical treatment of peptic ulcer disease.
Osteomalacia occurs as a complication of hepatocellular biliary disorders29 but is infrequent in pancreatic disorders. Biliary obstruction or parenchymal disease of the liver can diminish the synthesis of 25(OH)D and interfere with the intestinal absorption of vitamin D and calcium. In some patients, the defect in vitamin D-25-hydroxylation may be so great that vitamin D is an ineffective means of treatment and 25(OH)D must be administered.
HYPOPARATHYROIDISM
Osteomalacia only rarely occurs in patients with hypoparathyroidism (see Chap. 60). Bone pain suggests the diagnosis, and in some instances, because radiographs of the skeleton may be unremarkable, the diagnosis can be made only by histomorphometric analysis of bone biopsy material.30 Hypocalcemia and low or low-normal serum 1,25(OH)2D usually are present and appear to be important in the pathogenesis of the bone disease. Because PTH is the major regulator of the renal synthesis of 1,25(OH)2D, the low serum 1,25(OH)2D value and hypocalcemia result from its deficiency. Some patients can be treated effectively with vitamin D, whereas others require treatment with 1,25(OH)2D.30
PSEUDOHYPOPARATHYROIDISM
In pseudohypoparathyroidism (see Chap. 60), resistance to PTH results in hypocalcemia, retention of phosphate, and low serum 1,25(OH)2D values.30,31 and 32 Patients with pseudohypoparathyroidism rarely have osteomalacia.30 Hypocalcemia and a low serum 1,25(OH)2D value are important factors in the pathogenesis of the bone disease.30 As in hypoparathyroidism, some patients can be treated with vitamin D and others with 1,25(OH)D.30
CHRONIC RENAL INSUFFICIENCY
Sometimes osteomalacia occurs in patients with chronic renal failure (see Chap. 61). Several factors may contribute. These include low serum 1,25(OH)2D value resulting from loss of renal tissue and the enzyme 25(OH)D–1α-hydroxylase,33 retention of inhibitors of calcification, metabolic acidosis, and formation of abnormal collagen matrix. More commonly, skeletal changes of osteitis fibrosa cystica occur as a consequence of secondary hyperparathyroidism, sometimes in association with osteomalacia.34 Subperiosteal resorption may be present on the medial aspect of the middle phalanges. Resorption also may be evident at other sites, including the medial margins of the femoral necks and the inner aspects of the proximal tibiae. Osteomalacia may develop as a consequence of excessive intake of aluminum-containing phosphate binders,35 as a result of dialysis-induced phosphate depletion36 or renal phosphate wasting after renal transplantation.37
Osteomalacia may be caused by aluminum derived from water that is used for hemodialysis or from aluminum hydroxide gels that are used to bind phosphate (see Chap. 61 and Chap. 131). Aluminum is deposited in bone at the mineralization front and may impair calcification and cause osteomalacia.38 In aluminum-induced osteomalacia, serum iPTH is normal or minimally elevated, and the bone disease does not respond to treatment with vitamin D or its analogs. Long-term treatment with the chelating agent deferoxamine is effective in removing aluminum from bone.39 The osteomalacia can then be treated by calcium together with either 25(OH)D or 1,25(OH)2D.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree