7 Transoral Laser Microsurgery for Intermediate Supraglottic Cancer
Abstract
Locally intermediate supraglottic squamous cell carcinoma (SCCs) may be managed by a variety of surgical and nonsurgical approaches. First, when planning transoral laser microsurgery (TLM), the surgeon should fully delineate superficial and deep tumor infiltration. This may be done by careful endoscopic examination (using both white light and narrowband imaging) and cross-sectional imaging (CT and/or MR). Furthermore, nodal involvement should be routinely assessed (ideally by ultrasonography) in order to get a comprehensive view of the extension of the disease. TLM resection of each supraglottic subsite is characterized by different outcomes in terms of survival and function. While the quality of the voice is usually not influenced, a varied degree of swallowing impairment and aspiration should be expected temporarily. In general, patient evaluation has a crucial role in determining the optimal treatment and should be aimed at balancing oncologic and functional outcomes. For this reason, when assessing the “ideal” treatment for a given clinical scenario, it is mandatory to tailor the therapeutic choice in consideration of both patient- and tumor-related factors. The main limiting factors influencing the treatment choice when considering TLM in locally intermediate supraglottic carcinomas will be presented and discussed in the text, with particular emphasis on preoperative evaluation and planning.
7.1 Case Report
A 67-year-old male, with a long history of cigarette smoking, presented to our office complaining of progressive dysphagia, hoarseness, and loss of appetite lasting 2 months. In this period, he noticed some difficulties in swallowing solid foods that progressively worsened. He did not report any chronic comorbidities.
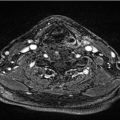
A transnasal videoendoscopic evaluation of the upper aerodigestive tract (UADT) was performed. This procedure was carried out in the office under topical anesthesia using a flexible ENF-V2 videoendoscope connected to an EvisExera II CLV-180B light source (Visera Elite OTV-S190, Olympus Medical Systems Corporation, Tokyo, Japan), integrated with a high-definition television (HDTV) and narrowband imaging (NBI) column. Videolaryngoscopic examination showed an exophytic lesion on the laryngeal aspect of the epigilottis at the junction between the suprahyoid and infrahyoid epiglottis. The lesion was irregular, ulcerated, and bled easily touched, characterized by an abnormal vascular pattern suspicious for malignancy at the HDTV-NBI examination ( Fig. 7‑1). 1 Physical examination did not reveal any suspicious lymph nodes in the neck.
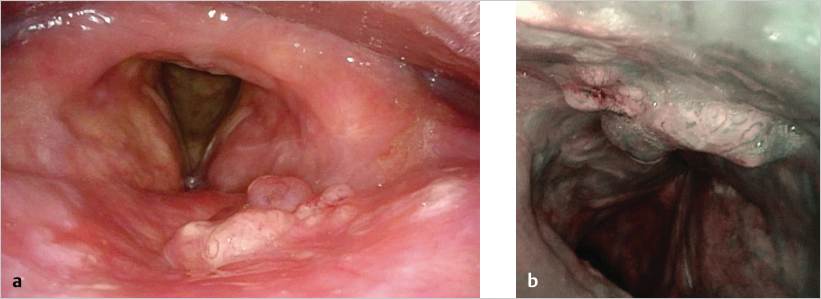
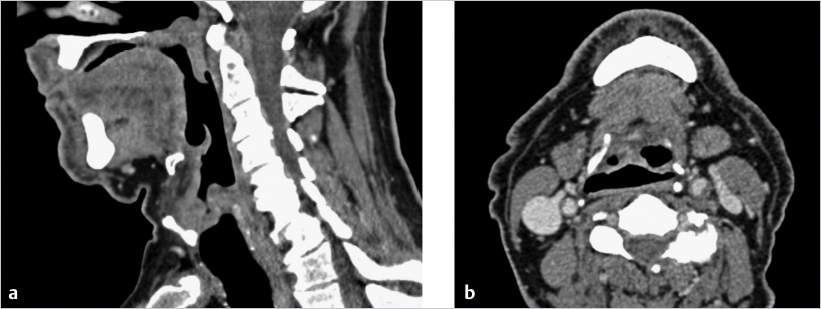
Contrast-enhanced computed tomography (CT) confirmed the presence of an exophytic lesion of the epiglottis without invasion of the pre-epiglottic space (PES) fat pad or extension in other adjacent laryngeal subsites ( Fig. 7‑2). No suspicious lateral neck lymph nodes were detected by imaging. Clinical staging was therefore confirmed to be supraglottic cT2N0.
The case was discussed at the Multidisciplinary Tumor Board and transoral laser microsurgery (TLM) was proposed as the treatment of choice.
The patient was intubated transorally with a laser-safe endotracheal tube (Mallinckrodt Laser Oral Tracheal Tube, Codivien, Mansfield, Ireland). Adequate laryngeal exposure was obtained by a “vallecular laryngoscope” (Microfrance Laryngoscope 124, Medtronic ENT, Jacksonville, FL), allowing visualization of the entire epiglottis and valleculae. The diagnostic evaluation was integrated by an intraoperative rigid endoscopy by 0- and 70-degree telescopes (Olympus 5-mm telescopes, Hamburg, Germany) to get a more precise three-dimensional assessment of the boundaries of the cancer. Before starting resection of the cancer, a biopsy was carried out for histopathological confirmation.
TLM was accomplished with a carbon dioxide laser (Ultrapulse Laser CO2, Lumenis, Yokneam, Israel), set on an ultrapulse mode, at 3 W of delivered power and at 400 mm of working distance.
Resection of the cancer was performed with a “multibloc technique” (i.e., progressively disassembling the lesion in an ordinated fashion without any attempt to perform an “en bloc” procedure), performing a transoral supraglottic laryngectomy (type IIb according to the European Laryngological Society classification). 2 The resection included the entire epiglottis, and the anterior line of resection went through the PES fat pad to provide complete tumor resection with free surgical margins. Vascular clips were applied on the superior laryngeal pedicles bilaterally, at the level of the pharyngoepiglottic folds. Frozen sections were performed to check the lateral, cranial, and distal (mucosal) margins of resection. No tracheostomy was carried out. A nasogastric feeding tube was positioned at the end of the surgical procedure. The patient was extubated at the end of surgery and sent to the Department of Head and Neck Surgery. Prophylactic antibiotic therapy (sulbactam and penicillin 1.5 g twice a day) was started at the end of surgery and prolonged for 10 days. Nonopioid analgesics were also prescribed.
On the first postoperative day (POD), videoendoscopy did not evidence any local edema and/or bleeding. On the third POD, videoendoscopic swallowing examination was performed, confirming the absence of dysphagia and/or aspiration. The nasogastric feeding tube was therefore removed and the patient gradually resumed oral feeding without significant issues. He was discharged on the fourth POD without complications.
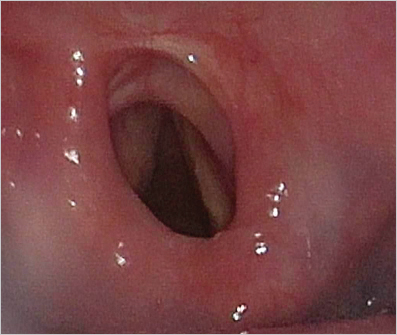
Clinical evaluation of swallowing and EAT-10 score 3 was normal and the patient received a score of 1 on the penetration–aspiration scale. 4 During follow-up, the patient gradually developed a supraglottic circular synechia with no sign of dyspnea ( Fig. 7‑3).
The histopathologic report confirmed the lesion to be a moderately differentiated (G2) squamous cell carcinoma (SCC) of the epiglottis. No signs of perineural and/or lymphovascular invasion were found. No involvement of the PES fat pad was detected. All superficial and deep resection margins were confirmed to be negative. Pathological staging was therefore defined as pT2NxG2R0. The patient had no indication for adjuvant treatments after discussion at the Multidisciplinary Tumor Board. Follow-up was performed by periodic transnasal flexible videoendoscopic examination in the office every 2 months and imaging (CT every year and neck ultrasonography every 4 months in the first year and every 6 months in the second). The patient is without evidence of locoregional or distant disease at 28 months after surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree