6 T1b Glottic Cancer, Vertical Partial Laryngectomy
Abstract
Tlb glottic cancer is a cancer that has more than one kind of treatment and the results are approximately the same. In some developed countries, the first treatment is radiotherapy and in others, transoral laryngectomies with or without laser. However, both treatments are expensive and need special materials. Despite the popularization of these techniques, vertical partial laryngectomy yields the same results, provides good voice rehabilitation, and does not need special materials. In this chapter, frontolateral (vertical) partial laryngectomy is described step by step, from diagnosis to surgery, with its tips and traps.
6.1 Case Report
A 45-year-old Caucasian male, laborer, presented to our clinic with a history of progressive dysphonia that had started 3 months previously, followed by dyspnea. He stated that he smoked one pack of cigarettes per day for 28 years as well as drinking 700 mL of draft beer during the weekend for the last 5 years. There were no comorbidities.
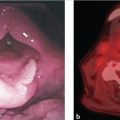
In the first evaluation, the patient presented a good general clinical condition and a 100% Karnofsky performance scale and complained of a 4-month dysphonia. He presented with hoarseness with little vocal range. No abnormalities were noticed during oroscopy and cervical palpation. Laryngoscopy revealed a vegetative mass occupying the entire right vocal fold (VF), up to the anterior commissure (AC). The left VF appeared normal. Both VFs presented normal mobility. The lesion did not extend to the infraglottis, ventricle or ipsilateral arytenoid ( Fig. 6‑1). He underwent a nasofibrolaryngoscopy and biopsy which revealed a squamous cell carcinoma.

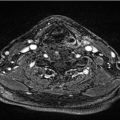
For more detailed evaluation of the extension of the lesion, a CT scan was performed which demonstrated an irregular lesion on the right VF, with heterogeneous contrast enhancement, and no invasion of the paraglottic space or the AC, and, the ipsilateral arytenoid was preserved. There were no signs of extension to the left VF. The patient underwent a frontolateral laryngectomy (FLL), under general anesthesia. Perioperative prophylactic antibiotics were administered. A tracheostomy was performed through a separate incision above the third tracheal ring. A second horizontal incision was made at approximately the level of the thyroid notch ( Fig. 6‑2 a). Skin flaps were elevated above the hyoid and below the cricoid cartilage. The strap muscles were then elevated, exposing the thyroid lamina and external perichondrium. The thyroid cartilage was incised at the midline and a posteriorly based perichondrial flaps were elevated bilaterally ( Fig. 6‑2 b). The extent of the elevation reflected the intended thyroid cartilage resection.
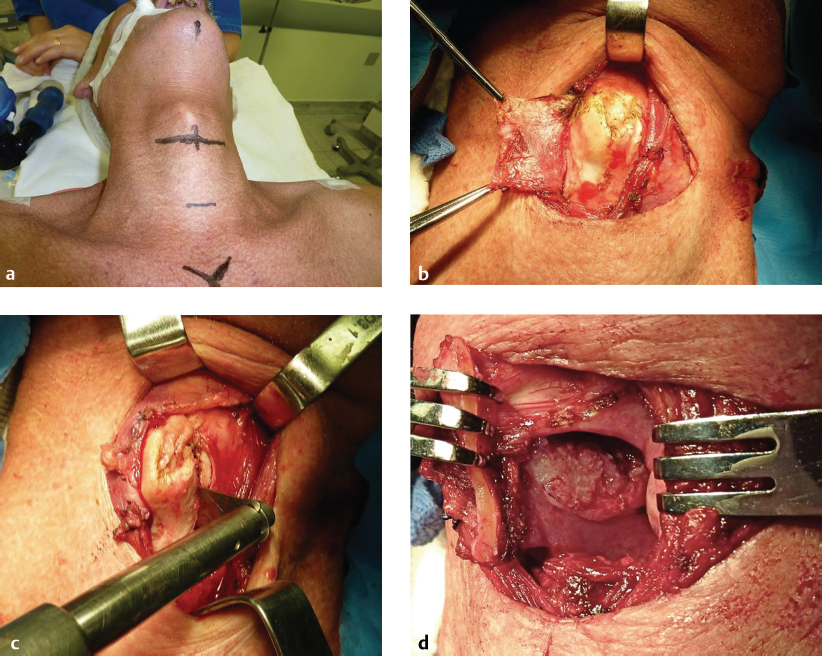
Vertical parallel thyroid cartilage cuts were made approximately 5 mm from each other including the notch ( Fig. 6‑2 c).
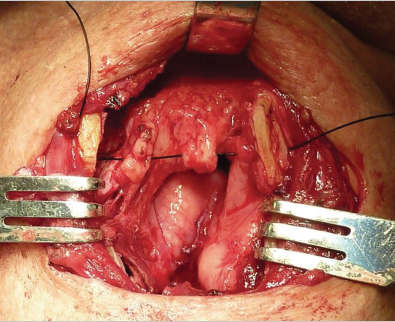
A wide cricothyrotomy allowed access to the subglottis. The tumor occupied the right VF. The thyrotomy was performed extensively on both sides. The left VF was then incised 2 mm laterally from the AC, through the cricothyrotomy. A dissection was made on the right side from the thyroid cartilage and an incision above and below the fold was performed, with the tumor under direct visualization, with approximately 3 mm of margin up to the vocal process of the right arytenoid ( Fig. 6‑3 and Fig. 6‑4).

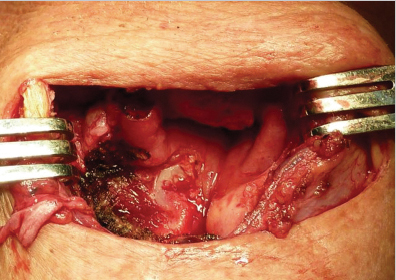
New margins from both sides of the VF were submitted to frozen section assessment and were free of tumor invasion. The left VF was fixed anteriorly to the residual thyroid cartilage and epiglottic residual petiole with a Vicryl suture. Reconstruction of the VF was done with a mucosal flap from the ventricular fold ( Fig. 6‑5 and Fig. 6‑6). The thyroid cartilage was approximated in the midline with nylon suture and the strap muscles were approximated as a second layer. A Penrose drain was then inserted. The skin was reapproximated in layers and a cuffed tracheostomy tube was introduced.

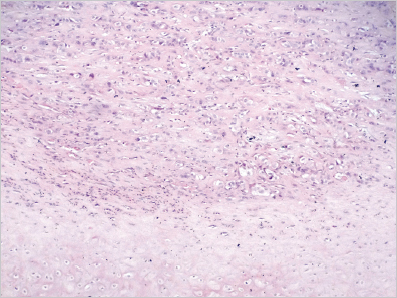
The patient made satisfactory progress and was discharged on the third postoperative day; the tracheostomy was occluded on the seventh day and the cannula was removed 7 days later. The patient was found to be eupneic and the voice was rough. A laryngoscopy 3 months after the surgery showed edema on the right side of the larynx; on the left side, the VF was mobile. A histopathological specimen showed the tumor adjacent to AC cartilage ( Fig. 6‑7).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree