Case study 53.1
A 51-year-old otherwise healthy man presents with stage IVB PTCL-NOS, with diffuse lymph node and bone marrow involvement.
• What is the standard initial therapeutic approach for advanced-stage (Ann Arbor Stage III–IV) PTCL-NOS?
PTCL-NOS is currently a provisional category in the 2008 World Health Organization classification as a heterogeneous group of nodal and extranodal mature T-cell lymphomas, which do not fit within any of the specifically defined mature T-cell entities. Morphologically, PTCL-NOS demonstrates paracortical or diffuse infiltrates with effacement of normal lymph node architecture, and it is more commonly associated with expression of CD3, CD4, and TCR β-chain, with frequent loss of CD5 and CD7. Variable expression of CD52 has been reported, and CD30 may be present but is most commonly absent. Epstein–Barr virus (EBV) is found in approximately 30% of all PTCL-NOS. Nearly all cases demonstrate clonal rearrangement of TCR genes. Gene expression profiling reveals that up to 20% of cases of PTCL-NOS have a gene expression profile characteristic of AITL, and another subgroup has features of cytotoxic T-cells that may represent a unique entity with a worse prognosis. The genetic heterogeneity portends that PTCL-NOS will eventually be segregated into more defined diseases.
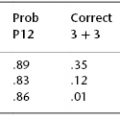
PTCL-NOS represents the most prevalent PTCL subtype in Western countries, affecting mostly older adults with a median age at diagnosis of 60 years and a slight male predilection. Nearly 70% of patients present with advanced-stage disease, frequently with bone marrow involvement. The International Prognostic Index (IPI) is predictive of overall survival (OS) and failure-free survival (FFS) in PTCL-NOS, as is the more recently developed Prognostic Index for PTCL-NOS (PIT), which adds bone marrow involvement in addition to the IPI variables of age, performance status, and lactate dehydrogenase (LDH).
The historical treatment of PTCL has been modeled after that of diffuse large B-cell lymphoma, with conventional-dose, systemic, anthracycline-containing chemotherapy representing standard front-line therapy. However, it is clear that this approach is suboptimal for PTCL, with reported long-term survival rates of only 20–40%, and as low as 10% for those with high IPI scores. Further, the retrospective International T-Cell Lymphoma Project found no survival benefit with the use of anthracycline-containing combination chemotherapy relative to non-anthracycline-containing therapy for all PTCL subtypes, with the exception of ALK-positive ALCL, suggesting that different and more effective approaches are clearly needed.
Despite these poor results, few studies have challenged the front-line use of standard anthracycline-containing combination chemotherapy regimens. Based on promising phase II results, the Groupe Ouest Est d’Etude des Leucemies et Autres Maladies du Sang (GOELAMS) conducted a prospective phase III study in newly diagnosed PTCL comparing an alternating etoposide, ifosfamide, and cisplatin (VIP) and adriamycin, bleomycin, vinblastine, and dacarbazine (ABVD) regimen to cyclophosphamide, doxorubicin, vincristine, and prednisone (CHOP). Sixty-five percent of patients had a confirmed diagnosis of PTCL-NOS. The investigators found that the VIP–ABVD regimen was more toxic and did not significantly improve 2- or 5-year event-free survival (EFS) as compared to CHOP. Additional groups have evaluated more intensive regimens, such as hyperCVAD (cyclophosphamide, vincristine, doxorubicin, and dexamethasone alternating with methotrexate and cytarabine), and have similarly reported no significant improvements relative to outcomes with CHOP. Several phase II studies have tested the use of alemtuzumab in combination with multi-agent chemotherapy in newly diagnosed PTCL, with reported high overall response rates (ORRs) of 60–90%; however, there were significant infectious complications, particularly when alemtuzumab was combined with fludarabine. Despite the infectious complications, the high activity with alemtuzumab-containing regimens prompted two ongoing phase III trials in Europe evaluating alemtuzumab plus CHOP as front-line therapy for PTCL. The Southwest Oncology Group (SWOG) evaluated the use of a gemcitabine-based regimen (platinum, gemcitabine, etoposide, and methylprednisolone (PEGS)) in newly diagnosed PTCL, with nearly one-half of study patients having a diagnosis of PTCL-NOS. Although tolerable, the PEGS regimen was not felt to be promising given the low ORR of 39% and a 2-year OS rate of only 30%. Finally, the German High-Grade Non-Hodgkin Lymphoma Study Group (DSHNHL) retrospectively analyzed 343 patients with PTCL (22% PTCL-NOS) treated on phase II or III clinical trials and found that patients aged 60 and younger without an elevated LDH appeared to benefit from the addition of etoposide to CHOP (CHOEP), with significantly longer EFS and a nonsignificant trend toward improvement in OS. A Dutch trial incorporated CHOEP on a biweekly schedule as induction therapy prior to autologous stem cell transplantation with promising results, as discussed further in this chapter.
Thus, outside of a clinical trial, this 51-year-old with newly diagnosed advanced-stage PTCL-NOS should be offered front-line CHOP chemotherapy, with consideration for the addition of etoposide, as no other regimen has been proven to be more efficacious. However, given the relatively bleak outcomes of this disease with this approach, a clinical trial should always be offered if available.
The patient receives six cycles of CHOEP and enters a complete remission (CR) as evidenced by positron emission tomography and computed tomography (PET–CT) and repeat bone marrow examination.
• Should the treating oncologist recommend consolidation with high-dose chemotherapy and autologous stem cell transplantation (auto-SCT)?
Current data support the use of auto-SCT as consolidation therapy for patients with PTCL demonstrating chemosensitive disease following induction therapy, including PTCL-NOS. Recently, long-term results were reported from the Nordic Lymphoma Group’s NLG-T-01 study, the largest prospective study to date evaluating upfront auto-SCT in PTCL. One hundred and sixty-six patients (mainly advanced stage, 39% with PTCL-NOS) with newly diagnosed PTCL (excluding ALK-positive ALCL, whose outcomes are favorable with conventional chemotherapy) were enrolled onto this multicenter study. Treatment consisted of dose-dense CHOEP (or CHOP for those over 60 years) given on a biweekly schedule, followed by auto-SCT for those achieving a partial remission (PR) or CR following induction. Using intention-to-treat analysis, with median follow-up of 60.5 months, the 3- and 5-year progression-free survival (PFS) rates were 48% and 44%, respectively; 3- and 5-year OS was 56% and 51%, respectively. The most impressive outcomes were seen in those patients with ALK-negative ALCL (5-year OS: 70%; PFS: 61%). Approximately one-fourth of patients experienced induction failure prior to transplant, and another 18% progressed or relapsed within the first 2 years of auto-SCT, with only 8% relapsing more than 2 years following transplant. These outcomes appear superior to the results of CHOP-like chemotherapy alone, which affords long-term survival rates on the order of 20–40% for the most common PTCL histologies. Retrospective analyses have reported even more favorable outcomes with upfront auto-SCT in PTCL, likely secondary to favorable patient selection, with long-term PFS and OS ranging from 59% to 63% and from 62% to 63%, respectively, in several small series of mixed PTCL subtypes.
Clearly there is room for improvement, as substantial induction failures and frequent posttransplant relapses diminish the ability of PTCL patients to both undergo and receive benefit from auto-SCT. Across studies, approximately 25–40% of patients do not respond to induction therapy and thus never qualify for consolidative SCT. More effective induction strategies, as well as studies focused on eradicating minimal residual disease and preventing posttransplant relapse, are greatly needed. There are little data regarding the role of allogeneic stem cell transplantation (allo-SCT) in the frontline setting; however, it may be reasonable to consider allo-SCT for the rare PTCL subtypes, such as hepatosplenic T-cell lymphoma, that do not appear to benefit from conventional therapy or auto-SCT. There does, however, appear to be a long-term survival benefit for patients with the common histologic subtypes (PTCL-NOS, ALK-negative ALCL, and AITL) who undergo auto-SCT in first PR or CR, and this patient should therefore be offered consolidative auto-SCT.
< div class='tao-gold-member'>