Transformed Lymphoma
1Centre Hospitalier de l’Université de Montréal (CHUM Hospital), Montreal, QC, Canada
2Robert H. Lurie Comprehensive Cancer Center of Northwestern University, Chicago, IL, USA
Multiple Choice Question
1. Which of the following does not constitute transformation?
- New diagnosis with areas of follicular lymphoma (FL) grade 1–2 and 5% diffuse large B-cell lymphoma (DLBCL)
- Long-standing FL, new mass with biopsy showing DLBCL
- Long-standing FL grade 1–2 with progression in one of the lymph nodes to FL grade 3a
- Long-standing chronic lymphocytic leukemia (CLL) previously untreated with a rapidly increasing cervical mass with a biopsy that shows DLBCL
There is a lack of consensus regarding the definition of histologic transformation (HT). Most experts agree that grade 1–2 follicular lymphoma that progresses to DLBCL or Burkitt lymphoma represents HT (Figure 46.1). The WHO Classification of Tumours of Haematopoietic and Lymphoid Tissues defines HT as “transformation or progression to a high-grade lymphoma usually DLBCL, but occasionally resembling Burkitt lymphoma or with features intermediate between DLBCL and Burkitt lymphoma.” Progression of FL grade 1–2 to FL grade 3 (situation C) is not considered histologic transformation but rather progression. Situation A is perhaps the most controversial. Some authors have considered the presence of both FL and DLBCL in the same lymph node to represent a “composite” lymphoma, and some have referred to it as “transformation at diagnosis.” Others require a defined interval between the diagnosis of FL and the more aggressive histology. The presence of both an indolent and aggressive lymphoma in the same lymph node implies but does not confirm early transformation. The WHO suggests reporting the two disease entities with their respective percentages of involvement. Composite lymphomas were rarely included in the major series of transformed lymphomas (TLs). Rarely, FL may transform to other histologies such as acute B-cell lymphoblastic leukemia or, as recently described elsewhere, to histiocytic or dendritic cell sarcoma.
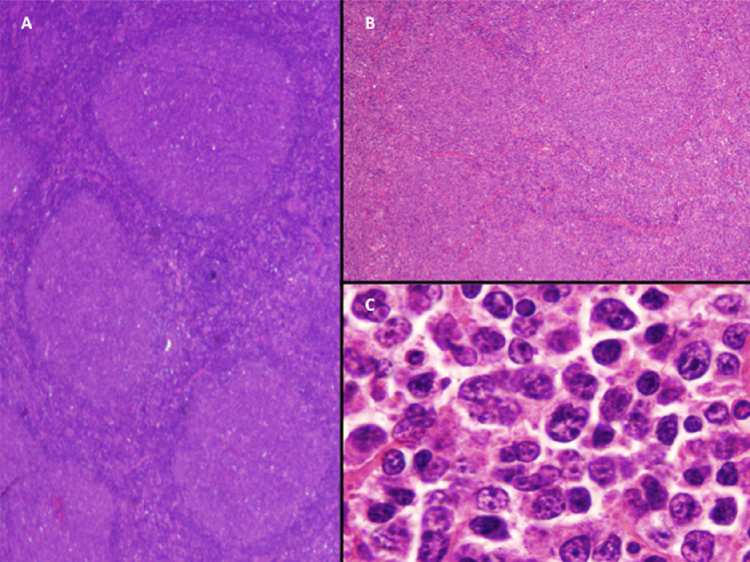
Transformation to DLBCL has been described for all the major subtypes of indolent lymphomas: small lymphocytic lymphoma and chronic lymphocytic leukemia (SLL–CLL), lymphoplasmacytic lymphoma (LPL), and marginal zone lymphoma. The first description of HT in SLL–CLL was made in 1928 by Richter and constitutes situation D. SLL–CLL can rarely transform to Hodgkin lymphoma and uncommonly to B-cell prolymphocytic leukemia.
A more scientifically robust definition of “transformation” requires demonstration of a clonal relationship between the original indolent lymphoma and the subsequent aggressive counterpart. This may be best demonstrated by molecular techniques characterizing the immunoglobulin gene. In the daily clinical setting, proving that the two lymphomas have the same light-chain restriction is usually sufficient to suggest a clonal relationship. The immunophenotype of the TL may differ from the original indolent lymphoma. Loss of CD10 expression occurs in 10% of cases, and a gain of MUM1 or CD30 occurs, each in 25% of cases. A change in phenotype does not preclude a clonal relationship between the two lymphomas. Transformation was diagnosed on clinical grounds in two series because of the association between aggressive clinical behavior and transformation. This association is not absolute and, whenever possible, the diagnosis should be made pathologically.