34 Laryngeal Transplantation
Abstract
Laryngeal transplantation is an exciting option for replacing laryngeal function. There have been three human larynx transplants that have been successful and fully reported. The surgical procedure has been well developed and variations have been described that include transplantation of skin, esophagus, and pharynx. Organ transplantation has several known associated risks and side effects including immune suppression–associated malignancies. These become increasingly important for non–life-sustaining transplants, especially in the setting of prior malignancies such as larynx cancer. Understanding these risks and placing them in the context of quality-of-life goals for patients is important. This chapter will describe the current state of the field and summarize the results of the three transplants previously performed.
34.1 Case Report
A 51-year-old female presented with a 10-year history of a tracheotomy-dependent, benign, and complete laryngotracheal stenosis. The stenosis was the result of a prolonged hospitalization for renal failure during which time, she required prolonged intubation and sustained multiple traumatic extubations. She underwent a kidney–pancreas transplantation 4 years prior to her larynx transplant presentation and was maintained on lifelong immunosuppression consisting of tacrolimus and leflunomide. 1
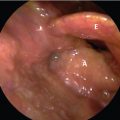
Endoscopic attempts had been unsuccessful in reestablishing an airway. At the time of her presentation, endoscopy demonstrated a fused glottis with absence of any air passage from the trachea through the larynx. CT with 3D reconstruction of her airway demonstrated that the complete stenosis extended from the level of the glottis to below the second ring of the trachea. She was completely aphonic and tracheostomy dependent.
After extensive counseling and testing, the decision was made to offer the patient a larynx transplant. A 2-year preparatory period commenced involving psychological evaluation, technical preparation using a porcine model and cadaveric specimens, team building with transplant support, and patient preparation. 2 , 3 Pretransplant, the patient underwent percutaneous gastrostomy tube placement and botulinum toxin (Allergan, Irvine, CA) injection into her bilateral submandibular and parotid glands in an effort to reduce salivary flow and potential aspiration. The procedure followed closely after the 2001 Cleveland Clinic publication describing the only comprehensively reported transplant. Significant modifications were made in the approach to the vascular and neural anastamoses. 4 In 2010, we performed our transplant at the University of California, Davis (UC Davis) over 18 hours in adjacent operating rooms with simultaneous organ procurement and recipient laryngectomy and transplant preparation occurring simultaneously.
The donor was a healthy, well-matched 38-year-old female who had suffered an anoxic arrest and had only been intubated for 3 days. Pretransplant evaluation included ABO blood group that was compatible with the recipient. Human leukocyte antigen alleles were tested and the recipient expressed a low level of sensitization against human leukocyte antigens (HLAs) despite her prior transplantation. While we avoided donor HLAs that our recipient had antibodies against, we did not limit the donor to minor loci match as we prioritized the donor’s anatomic and functional factors. Of note, a positive cytomegalovirus result was detected on her infectious panel.
The organ retrieval included the larynx, pharynx, esophagus, thyroid, and parathyroid glands, with all of the nourishing great vessels of the neck and mediastinum. After perfusion with University of Wisconsin perfusate, the transplant was procured at the same time as the liver and kidneys for other transplant recipients. The larynx transplant was prepared by isolating the dominant arterial flow that happened to be from the right side, which was prioritized for the first revascularization anastomoses. The mucosa was removed from the esophagus, but the muscular esophagus was opened and used as a secondary blood supply to the membranous trachea. Additionally, the superior laryngeal nerves bilaterally, right recurrent laryngeal nerve, and left adductor branch of the recurrent nerve were isolated. The left adductor branch was divided from the recurrent laryngeal nerve leaving abductor fibers still in continuity with the stump of the recurrent laryngeal nerve.
The transplantation was performed after laryngectomy by anastomosing the right recipient transverse cervical artery to the right inferior thyroid artery of the transplant and the right recipient jugular vein to the donor brachiocephalic vein. Successful reperfusion of the entire transplant was confirmed with an ischemia time of 300 minutes. Additional microvascular anastomoses were made between the recipient right superior thyroid artery and the donor right superior thyroid artery, the recipient left transverse cervical artery to the donor left inferior thyroid artery, and the recipient left internal jugular vein and the recipient left superior thyroid vein. Microneurorrhaphies were performed between the donor and recipient superior laryngeal nerves bilaterally and recurrent laryngeal nerve on the right side. An attempt at selective reinnervation was performed on the left side with an end-to-side microneurorrhaphy from the recipient phrenic nerve to the donor recurrent laryngeal nerve (abductor fibers) and the ansa cervicalis of the recipient to the adductor branch of the donor recurrent laryngeal nerve. Eight rings of transplanted trachea were used to reconstruct the trachea. Pharyngeal anastomoses were performed and the larynx was suspended to the hyoid bone.
Perioperatively, the patient was immunosuppressed with rabbit antithymocyte globulin, methylprednisolone, and mycophenolate. She was ultimately maintained on her renal transplant regimen of tacrolimus and leflunomide. Despite some minor perioperative complications such as transient infections of her trachea, lung and central line, mucosal candidiasis, and diarrhea, she did well postoperatively.
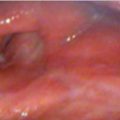
Her function posttransplant has been remarkable. She unequivocally professes a significant improvement in her quality of life and social engagement. While she remains cannulated with a tracheostomy, she has a widely patent airway and a strong voice. Acoustic analysis demonstrated normal parameters except for a lower fundamental frequency for her conversational voice. She is able to take a normal oral diet despite having some delay in initiation of her diet in the posttransplant period and requiring several dilations of an upper esophageal stricture. To date, after several biopsies up to 4 years after her transplant, she has not manifested any signs of rejection and it is now 7 years since the surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree