30 Reconstruction for Advanced Cancer: Latissimus Dorsi Myocutaneous Flap
Abstract
The pedicled myocutaneous latissimus dorsi flap is a versatile flap that is suitable in reconstruction of the head and neck due to its thinness, wide arc of rotation, and possible (large) dimensions. The surgical technique is straightforward and reported complication rates are relatively low. The flap can be used in pharyngeal reconstruction as an alternative to free tissue transfer when primary closure is not feasible. A case is reported of advanced laryngeal cancer reconstructed with a latissimus dorsi flap. The history, background, and possible (contra)indications are mentioned. The surgical technique is meticulously described. Specific subjects are addressed such as the necessity of awareness of the angiosomes and the trajectory and branching of the pedicle. The position of the skin paddle should not be designed too caudal in relation to the muscle to allow proper perfusion of the paddle. It is necessary to ligate the branches to the underlying serratus muscle to achieve adequate mobilization to the head and neck area. Finally, the most important tips and traps are described in order to achieve an optimal result in performing the latissimus dorsi flap in pharyngeal reconstruction.
30.1 Case Report
A 70-year-old male presented with progressive hoarseness and dysphagia over the past 5 months. He had a history of recurrent airway infections and coughing during deglutition suggesting aspiration. His medical history noted a transient ischemic attack and hypercholesterolemia for which he used anticoagulants and statins. The patient was a current cigarette smoker and had a smoking history of 55 pack-years. He never used alcohol.
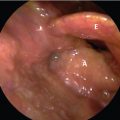
On physical examination, the patient had a hoarse voice and frequent coughing. Direct laryngoscopy revealed a large ulcerating lesion originating from the left supraglottic area and extending to the left hypopharynx. The left vocal cord was immobile. There was evidence of saliva, penetrating the glottis. There were no palpable lymph nodes in the neck.
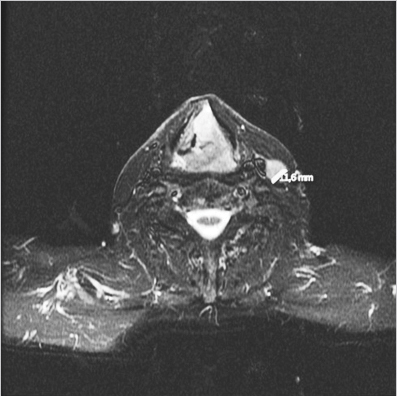
An MR of the larynx was performed showing a left supraglottic cancer with growth to the piriform sinus on the left. There was obvious cartilage invasion ( Fig. 30‑1).
Enlarged ipsilateral cervical nodes in levels II and III were identified for which an ultrasound with fine-needle aspiration cytology was performed.
An examination under general anesthesia was performed for biopsy and to evaluate the exact extent of the cancer. The cancer extended from the left false vocal cord to the laryngeal aspect of the epiglottis and the glottis. There was extension of the lesion to the medial wall of the left hypopharynx without invading the posterior pharyngeal wall. Biopsies were taken.
Histopathology showed a moderately differentiated squamous cell carcinoma. Cytology showed two cancer-positive nodes in the ipsilateral neck in levels II and III. The was staged as a pT4aN2b carcinoma of the supraglottic larynx.
Due to the extent of disease and poor functionality of the larynx, a total laryngectomy with partial pharyngectomy and a left selective neck dissection of levels II to IV was advised by the multidisciplinary head and neck team. A latissimus dorsi (LD) myocutaneous flap was suggested for pharyngeal reconstruction.
The patient underwent the above-mentioned surgery including a hemithyroidectomy on the left. Cricopharyngeal myotomy was performed as well as placement of a voice prosthesis. Pharyngeal closure was achieved using a myocutaneous LD flap from the left.
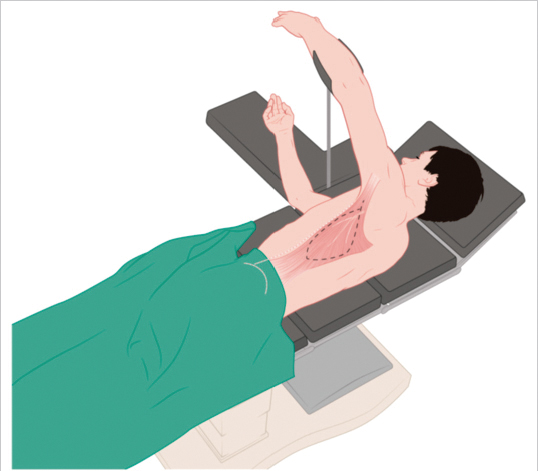
For harvesting of the flap, the patient was placed in the right lateral decubitus position. The shoulder was abducted for exposure of the axillary area by suspension of the forearm. The patient was placed on special cushioning to avoid excessive pressure specifically on the iliac crest. The flap was outlined by measuring the distance from the surgical defect to the pectoral–humeral junction and by assessing the length needed to reach the recipient site. The lateral border of the muscle was outlined running from the midpoint of the axilla to the posterior iliac crest as depicted by the white dotted line in Fig. 30‑2 .
The skin paddle was designed over the second angiosome to ensure proper perfusion ( Fig. 30‑3).
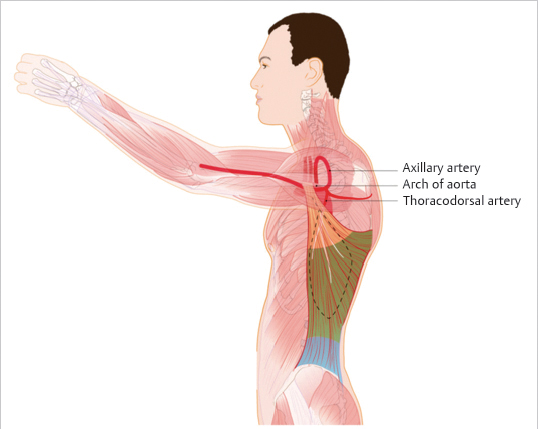
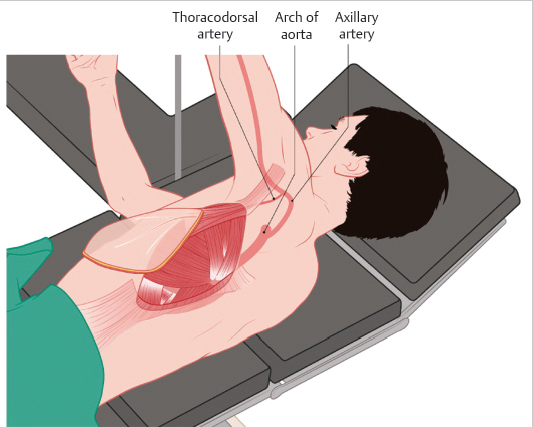
The dimensions of the skin island were determined based on the dimensions of the surgical defect. Incision commenced from the midpoint of the axilla down to the lateral border of the skin paddle. While incising anteriorly of the paddle, the lateral border of the muscle was identified. Once proper attachment of muscle and skin was identified, the muscle was mobilized from the underlying structures by dissecting it in the posterior direction. The serratus anterior muscle was exposed and dissection proceeded in the plane between these muscles. After detaching the distal tip of the skin paddle and transection of the muscle caudally, dissection was started at the medial insertion of the LD muscle for further cranial mobilization. In this area, multiple intercostal arteries were identified and ligated. Mobilizing the muscle upward, the thoracodorsal vessels that constitute the pedicle were carefully identified. Branches to the serratus anterior muscle were ligated and divided as well as the thoracodorsal nerve for adequate mobilization. When the muscle was fully mobilized and only attached to its vascular pedicle, it was delivered to the recipient site via transfer through the axillary fossa and tunneled subcutaneously ( Fig. 30‑4).
Care was taken to make the tunnel wide enough to avoid compression of the pedicle. The skin paddle was trimmed to the correct size to fit the pharyngeal defect. The skin paddle was sutured into the defect using continuous semipermanent sutures ensuring a watertight closure of the neopharynx. The donor site was closed primarily after leaving two suction drain catheters after some undermining and without undue tension. The skin was closed using staples.
The patient remained on a nothing by mouth for 7 days, after which a barium swallow examination was performed. There were no signs of fistula and the patient started uneventful oral intake. He immediately had a clear prosthetic voice. He was discharged from the hospital 12 days after surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree