3 Robotic Surgery for Early-Stage Laryngeal Cancer
Abstract
Surgical management of early-stage laryngeal cancer has evolved in the recent past. Minimally invasive surgical strategies and techniques have gained increasing importance and are now used more frequently. While transoral laser surgery is the most commonly employed technique, robotic surgery is gaining traction. The da Vinci surgical robot is the most established and frequently used surgical robot. However, the size of this system makes access to the larynx/supraglottis challenging. Recently, the Flex system has been approved for transoral surgery. This chapter describes the role of robotic surgery in the management of early-stage laryngeal cancer. We describe a case of an early laryngeal tumor that was treated with transoral robotic resection using the Flex robotic system. We detail the considerations in patient management. The criteria for patient selection, both functional and anatomic, are discussed. We also discuss the important considerations to ensure adequate exposure of the tumor for transoral surgery. The postoperative management of patients treated with robotic surgery is described, along with tips and pitfalls. We also contrast the role of radiation therapy to robotic surgery for the management of this disease.
3.1 Case Report
A 54-year-old Caucasian female patient presented with progressive throat pain that had started 4 months previously, followed by episodes of choking on liquids. She admitted to tobacco use, with a 45 pack-year smoking history, and social alcohol use. The patient was otherwise healthy without significant comorbidities of dyspnea or pulmonary disease.
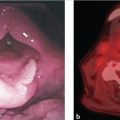
At the time of the consultation, the patient was healthy and presented some mild hoarseness. There was no lymphadenopathy. A direct laryngoscopy revealed an ulcer-infiltrative lesion in the right aryepiglottic fold, without extension to the anterior commissure or the glottis. The mobility of both vocal folds was normal. The lesion did not extend to the infraglottis, ventricle, or ipsilateral arytenoid.
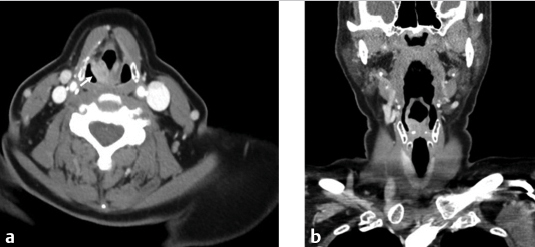
For a better deeper evaluation of the extension of the lesion, and to assess the nodal disease burden, a CT scan with contrast, using fine cuts through the larynx, was performed. There were no signs of extension to the glottis or the paraglottic space ( Fig. 3‑1).
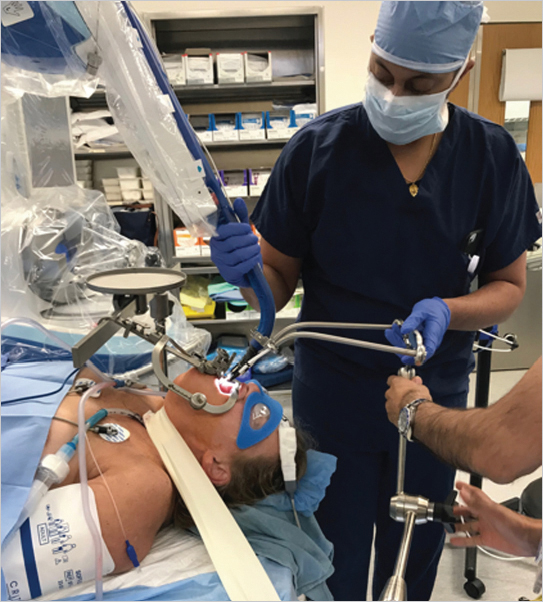
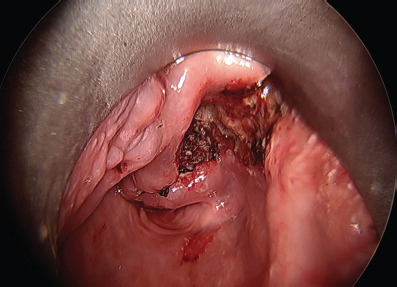
The ease of exposure of the tumor was confirmed with an operative endoscopy. The anatomopathological result showed a moderately differentiated squamous cell carcinoma. In order to facilitate control of the airway and improve surgical access, a tracheotomy was performed. Exposure of the lesion was obtained using a Flex retractor. The tumor was localized to the aryepiglottic region, without extension to the piriform sinuses or the postcricoid area ( Fig. 3‑2).
The patient then underwent a transoral robotic resection of the lesion using the Medrobotics Flex surgical robot. The surgical margins of resection required excision of the aryepiglottic fold, portion of the epiglottis, and mucosal resection for the interarytenoid area. Both arytenoids were preserved. The Flex robot was placed into the mouth and the tumor was exposed and prepared for resection.
For the performance of the surgery, the tumor was exposed using the Flex retractor. This afforded excellent visualization of the tumor and surrounding anatomy. The resection was commenced by identifying the margins of the tumor. These extended anteriorly/medially to involve the hemiepiglottis, laterally to the pharyngoepiglottic fold, and posteriorly to the arytenoid. The dissection was initiated by transecting the epiglottis. The dissection was then carried laterally by incising into the mucosa in the vallecula. This allowed for dissection in the lateral aspect of the tumor. The pharyngoepiglottic fold was then transected. In this area, we encountered the arterial supply to the larynx, the superior laryngeal artery. This vessel was controlled using bipolar cautery and hemostatic clips. The remainder of the dissection is continued posteriorly. The arytenoid mucosa was preserved, but the aryepiglottic fold was completely resected to ensure adequacy of resection. The medial limit of the dissection is the interarytenoid space, which is preserved to avoid posterior glottic stenosis. It is important to note that the deep margin of resection must be assessed intraoperatively, by paying careful attention to the depth of resection. Additionally, the surgical assistant can use suction cannula to palpate the tissues, to ensure adequate resection margins.
Intraoperative pathologic consultation is used to ensure that the surgical margins are free of malignant disease. This is accomplished by submitted representative margins from the main resection specimen ( Fig. 3‑3).
After finishing tumor resection, hemostasis is obtained in the surgical field using vasoconstrictive agents (such as dilute epinephrine or oxymetazoline) in combination with bipolar cautery. The tracheostomy is maintained until the lymphadenectomy is completed. The patient was returned to the operating theater 1 week later. At this time, bilateral neck dissections, levels 2 to 4, were performed.
The histopathological report showed well-differentiated squamous cell carcinoma adjacent to the thyroid cartilage, but with no invasion ( Fig. 3‑4).
The patient progressed satisfactorily; the tracheotomy was occluded and the patient was discharged. The nasoenteral tube was retained for a total of 5 days. The tracheostomy tube was removed after the postoperative visit on postoperative day 10.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree