28 Reconstruction for Advanced Cancer: Pectoralis Major Myocutaneous Flap
Abstract
In many head and neck surgery services, the pectoralis major myocutaneous flap remains the mainstay reconstructive method because of the lack of availability of a specialized reconstructive surgical team and the costly instrumentation required to perform free flaps. Even in head and neck surgery services in which free flaps are used routinely, pectoralis major fasciocutaneous or myocutaneous flaps can be performed in combination with free flaps to reconstruct larger tridimensional surgical defects, to protect critical vessels at risk for rupture, and to manage or prevent salivary fistulas. Therefore, pectoralis major flaps must be part of the armamentarium of every head and neck surgeon who provides major surgical procedures.
28.1 Introduction
Since Ariyan’s first report in 1979, 1 the pectoralis major myocutaneous flap (PMMF) has been one of the most widely used methods for reconstruction of major defects in head and neck cancer surgery because of its technical ease, versatility, proximity to the head and neck region, and the possibility of carrying well-vascularized tissue to irradiated areas. 2 Even in head and neck centers where free flaps are available, PMMF can be used in association with free flaps for major defect repair, for protection of critical vessels at risk of exposure and rupture, and to avoid or to minimize the occurrence and severity of pharyngocutaneous fistula, especially in patients undergoing salvage surgery after radiotherapy or radiochemotherapy. 3
28.2 Surgical Technique
In our institution, we delimit the island of skin according to the defect to be reconstructed. In most cases, we perform an island flap, partially preserving the upper part of the pectoralis major muscle with a low skin incision, decreasing the functional impairment of the arm, while allowing a possible future use of a Bakamijan deltopectoral flap if necessary. After incision of the skin, the cutaneous flap is elevated laterally to preserve the muscular fascia to reduce bleeding; the section of the muscular fibers of the major pectoralis is performed at the lower border of the flap to facilitate identification of the vascular pedicle, which passes between the fibers of the pectoralis major and pectoralis minor. Rotation of the PMMF to the cervical region can be done through a tunnel on or below the clavicle, which has the advantage of increasing the upper limit of reach of the flap by approximately 2 to 3 cm. We recommend sectioning part of the subclavian muscle in the topography of the passage of the vascular pedicle, to reduce the risk of compression. 4 In obese patients and patients with a bulky pectoralis major, passage of the flap through the subclavicle route may not be feasible.
28.3 Primary Indications in the Treatment of Advanced Laryngeal Tumors
PMMF is widely used for reconstruction in patients undergoing surgical treatment of advanced laryngeal tumors. PMMF can be used for reconstruction of the partial or total defect of the pharynx, for reconstruction of the skin, for protection of the great vessels in patients at high risk for dehiscence and exposure, as well as for the prevention of pharyngocutaneous fistulas in cases of primary closure of the pharynx in salvage surgery, primarily after radiotherapy (with or without associated chemotherapy).
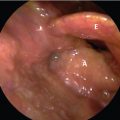
28.3.1 Reconstruction of Pharyngeal Defects
Regarding the reconstruction of defects after total pharyngolaryngectomies, PMMF has been the second option in centers where free flaps are available, and its use is indicated primarily for patients with poor clinical performance. 5 In the study by Chan et al, 202 patients underwent total reconstruction of the pharynx after resection of advanced laryngeal or hypopharyngeal cancer: 92 patients underwent reconstruction with PMMF; 24 patients underwent reconstruction with free anterolateral thigh (ALT) flap; and 24 patients underwent reconstruction with free jejunal flap. The fistula rate in the PMMF group was 23.9%; it was 12.5% in the free ALT group, and just 2.3% in the jejunum flap group. With regard to late stenosis, it was 27.2% in the PMMF group, 12.5% in the ALT group, and 2.3% in the jejunal flap group. Reconstruction of mucosal defects with myocutaneous or fasciocutaneous flaps presents a higher rate of pharyngocutaneous fistulas and late stenosis. Conversely, in total pharyngolaryngectomies extended to the base of the tongue, reconstruction with jejunum may not be feasible. 6
In situations in which reconstruction with the jejunal free flap is impossible, PMMF should be sutured to the prevertebral fascia in the reconstructions after total pharyngolaryngectomy, since it presents a lower complication rate compared with the use of PMMF as a tunnel. Carvalho et al, evaluated the results of 69 patients undergoing total pharyngeal reconstruction, 45 patients underwent reconstruction with PMMF, of which 29 were made with the muscle sutured the prevertebral fascia and 16 were made as a tunnel with PMMF to reconstruct the pharynx. In this subgroup of patients, a general rate of immediate postoperative complications of 51.7% was observed in the group sutured to the prevertebral fascia, and a rate of 62.5% in the muscle in the tunnel. The most common immediate complication in the group of patients with muscle sutured to the fascia was infection of the surgical site (37.9%), whereas in the muscle group with tunnel, the most immediate complication was fistula formation (50%). The most common late complication in the group with muscle sutured to in the fascia was stenosis (21.4%), whereas in the muscle group with tunnel, 37.5% of patients had stenosis. 7
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree