25 Salvage Surgery after Radiotherapy: Supracricoid Laryngectomy
Abstract
Conservation surgery in the form of transoral laser microsurgery and open partial laryngectomy is increasingly used for salvage of recurrent cancer of the larynx following radiation therapy in order to avoid the sequelae of total laryngectomy. Supracricoid partial laryngectomy with cricohyoidoepiglottopexy or cricohyoidopexy has been proven to be oncologically sound and to provide satisfactory voice and swallowing function in this setting. Keys to success are correct selection of patients and cancer, experience with this technically demanding surgery, and swallowing rehabilitation with a team of dedicated speech and swallowing therapists. Review of the literature reveals good oncological outcome of supracricoid partial laryngectomy as salvage procedure after failure of radiation in very well selected patient cohorts. Conversion to total laryngectomy either during surgery due to unexpected tumor extension or postoperatively due to failed swallowing rehabilitation has to be discussed with the patient.
25.1 Case Report
A 71-year-old Caucasian male presented with progressive hoarseness over a period of 3 months. The patient denied any pain, swallowing was normal without clinical signs for aspiration, and there was no dyspnea. He stated having stopped smoking cigarettes 10 years ago with an estimated cumulative consumption of 40 pack-years. The patient experienced a myocardial infarction 2 years ago and has been under medication with aspirin since that time.
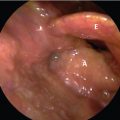
At consultation, the patient presented in good general health, but with a severely hoarse voice. Laryngoscopy revealed an exophytic lesion of the anterior part of both vocal folds with extension to the anterior commissure ( Fig. 25‑1). There was no supraglottic or subglottic extension of the tumor. On videostroboscopy, there was an impaired motility of the right vocal cord. Vocal fold vibration was totally absent.

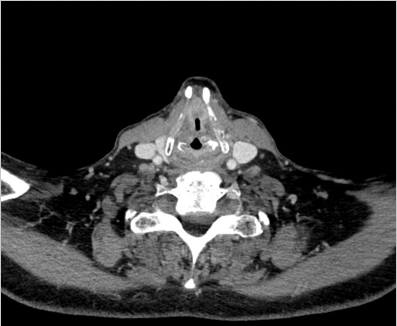
High-resolution computed tomography (CT) of the larynx demonstrated a tumor involving both vocal ligaments anteriorly with invasion of the anterior commissure ( Fig. 25‑2).
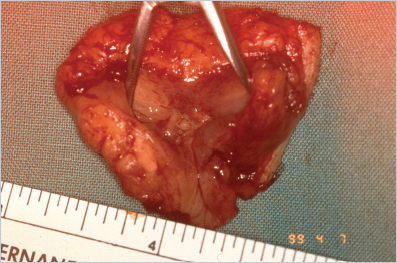
The tumor was staged cT2 cN0. Because of bilateral vocal fold invasion, the patient underwent primary radiation of the larynx. Unfortunately, the tumor recurred within the first year after completion of radiotherapy. The recurrent cancer had almost exactly the same extension as prior to therapy. No subglottic extension was noted on endoscopy. CT revealed no extralaryngeal spread. The cancer was staged rT2 rN0. Due to deep invasion of the anterior commissure and inadequate exposure on endoscopy TLM was judged as not feasible. The patient was in good general health with normal pulmonary function. After thorough discussion with the patient and his family and Multidisciplinary Tumor Board decision, the patient was offered supracricoid partial laryngectomy (SCPL). The patient was also consented for total laryngectomy in case unexpected extension of the cancer was discovered intraoperatively. A percutaneous endoscopic gastrostomy (PEG) tube was placed at the beginning of surgery. The SCPL with cricohyoidoepiglottopexy (CHEP) was uneventful and frozen sections of the margins at the cricoid showed clear resection margins ( Fig. 25‑3). There were no complications during the postoperative course, and the patient was decannulated 4 weeks after surgery. Swallowing rehabilitation was prolonged with PEG removal after 5 months. The patient had a good but hoarse voice. Currently, he is doing well with no evidence of cancer after 3 years.
25.2 Discussion
In the last decades, organ-preservation strategies have been increasingly used in the treatment of cancer of the larynx. The number of total laryngectomies as initial treatment has dramatically decreased in most parts of the world. Progress in radiation technology and the introduction of chemotherapy as an adjunct to radiation has led to the increased use of nonsurgical therapy strategies in laryngeal oncology. The widespread use of transoral laser microsurgery (TLM) and the advances in open partial laryngectomies have diminished the number of total laryngectomies. The ultimate goal of all these achievements was to equal the excellent tumor control provided by total laryngectomy, but to preserve the organ’s function.
Treatment options for residual or recurrent cancer after primary radiation or chemoradiation include total laryngectomy, open partial laryngectomy, and TLM. 1 The primary treatment choice in the radiorecurrent setting in most centers even nowadays is total laryngectomy. In contrast to other head and neck subsites, the larynx yields a favorable outcome after salvage surgery with overall survival rates above 60%. 2 Diagnosis and management of recurrent cancer of the larynx remains challenging due to postradiation chronic inflammation, edema, and fibrosis. Tumor extension is difficult to visualize and even getting a reliable biopsy often proves to be difficult. Larynx sparing surgical procedures for a radiorecurrent cancer have been recently reported with encouraging results. Conservation surgery has been compared to total laryngectomy in a series of 726 salvage patients from the National Cancer Database in the United States. 3 All patients presented with initial T1 or T2 lesions prior to radiation. Slightly more than 7% of patients required salvage surgery, 24% receiving total laryngectomy, 35.1% open partial laryngectomy, and 40.9% TLM. In this selected cohort, conservation surgery by either open partial laryngectomy or TLM yielded comparable outcome to total laryngectomy. In a series from Italy of 71 patients, 31% of patients with recurrence after primary radiation underwent TLM, 21% open partial laryngectomy, and 48% total laryngectomy. 4 There was no statistically significant difference in terms of disease-free survival between the three groups. In a systematic review and meta-analysis evaluating the outcome of TLM for radiorecurrent laryngeal carcinoma, the pooled mean estimates for local control at 24 months were 56.9% after first TLM and 63.8% after repeat TLM and the pooled mean laryngeal preservation 72.3%. 5 The authors conclude that TLM for recurrent laryngeal cancer is an oncologically sound procedure in very well selected patients with earlier stage (rT1/2) lesions. In summary, early-stage recurrences of cancer of the larynx are suitable for conservation surgery in a subset of very well selected patients, either by TLM in case of well-circumscribed lesions with adequate laryngeal exposure or by open partial laryngectomy.
SCPL is an open partial laryngectomy procedure that involves the resection of the entire larynx and impaction of the hyoid bone with the cricoid ring. In case of preservation of the suprahyoid part of the epiglottis, the reconstruction is a CHEP, and in case of total resection of the epiglottis a cricohyoidopexy (CHP). Initially described by Majer and Rieder in 1959 and further developed in France and other European countries, the SCPL was mainly used for initial treatment of glottic and supraglottic cancer avoiding the permanent tracheostoma of a total laryngectomy. 6 The technique proved to be oncologically sound even for advanced (T3) cancer and provided good function with regard to swallowing and voice. 7 , 8 , 9
SCPL has also been advocated in recent years for the management of recurrent laryngeal cancer after primary radiation. The advantages of SCPL over total laryngectomy are the avoidance of a permanent stoma and the preservation of voice. As in the primary setting, SCPL is only suited for a select group of cancers. Subglottic extension to the level of the cricoid, invasion of the hyoid bone, fixation of the arytenoids, and extralaryngeal spread are contraindications. From the patient side, inability to adhere to postoperative rehabilitation of swallowing and speech and compromised respiratory function are factors against a SCPL. In a report by Sperry et al, 96 patients undergoing SCPL for primary laryngeal cancer in 54, and recurrent laryngeal cancer in 42 cases, have been evaluated. 10 Out of the 42 recurrent cases, 23 were staged rT1, 12 rT2, 6 rT3, and 1 rT4. The 5-year local control rate with larynx preservation was 89%, while the ultimate 5-year local control rate with total laryngectomy in case of recurrence 100%. A recent systematic review and meta-analysis of SCPL for radiorecurrent laryngeal cancer revealed promising results. 11 Only patients with tumors staged rT2 and rT3 were included. The pooled local control rate, disease-free survival, and overall survival for all 251 patients out of 11 studies achieved 92, 80, and 79%, respectively. The mean pooled larynx preservation rate was 85.2%, the mean pooled decannulation rate was 92.1%, the pooled mean rate of efficient swallowing was 96.5%, the pooled mean PEG dependence rate was 3.5%, and the pooled mean aspiration pneumonia rate was 6.4%. Total laryngectomy due to chronic aspiration was necessary in only two cases. The authors concluded that SCPL is a valid option in radiorecurrent cancer of the larynx with excellent oncological and functional outcome. Indications include rT1 and rT2 lesions with limited endoscopic exposure and/or invasion of the anterior commissure, rT2 lesions with impaired vocal cord mobility, and rT3 lesions with limited invasion of the paraglottic and pre-epiglottic space and no extralaryngeal extension.
The major concern in SCPL is functional outcome, in particular swallowing function. Swallowing is a fundamental function heavily impacting the patient’s quality of life. Aspiration pneumonia is a potentially life-threatening complication. The reluctance in performing SCPL is even higher in the radiorecurrent setting because of functional concerns and fear from complications. In a comparison of 82 SCPL for radiation failures versus untreated cases, there were no statistical differences with regard to postoperative complications and functional outcomes as assessed for decannulation rate, swallowing, and phonation. 12 A similar comparison in another study in 27 patients confirmed these good results. 13 In contrast to these favorable results, there are also studies in the literature that report on high rates of surgical complications, prolonged swallowing rehabilitation, and frequent aspiration pneumonias. 14 , 15 , 16 , 17 , 18 , 19 In summary, most authors agree on SCPL to be an oncologically sound and also with regard to complications and functional outcome valid option in the setting of a radiorecurrent laryngeal cancer. To select the right patient with the right cancer seems to be the key for success.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree