2 Society for Mucopolysaccharide Diseases, Amersham, UK
3 European Gaucher Alliance, Dursley, UK
Introduction
The arrival of a newborn baby is a time of excitement and change. The first question asked by the new parents is “Is my baby alright?” Fortunately, for the great majority the answer is “Yes”. Sadly, in a small number of cases the answer is “No”, often precipitating a medical emergency during which the needs of the parents may be pushed aside in the rush to intervene; parents are often left feeling marginalised and at a loss.
Advances in screening technologies and improvements in antenatal care mean that, for a growing number of diseases and disorders, a diagnosis can be made during pregnancy. This gives expectant parents the opportunity to find out about the condition detected and make more informed choices among the options available to them. However, despite rapid advances in research, and greatly increased understanding of the care and support women and their (potential) children need to maximise their chances of having a healthy baby, it remains the case that many babies with serious life-limiting conditions remain undetected for considerable periods of time, leaving parents struggling to understand what has happened and how to cope with the consequences. This is particularly the case if the disease in question is rare. In these circumstances, obtaining a timely and accurate diagnosis, accessing appropriate services and receiving adequate support can be a time-consuming and uncertain process.
The scale of the problem
This is not a trivial issue. Families affected by rare diseases can sometimes feel marginalised, almost as if “rare” equates with “unimportant” in terms of the priorities of the health care system. And while it may indeed be the case that, on its own, any one rare disease may only affect a handful of families in the UK, the fact that there are so many different rare diseases [over 6000 identified (and rising) as new diagnostic tools are developed] means that, paradoxically, rare diseases are not actually uncommon.
It has been estimated that rare diseases, as defined throughout the European Union as those with a prevalence of 5 in 10000 or fewer [1], affect up to 1 in 17 of the population. This means that in the UK there are around 3.5 million people who live with the daily consequences that arise from serious, lifelong, often degenerative and sometimes lethal rare conditions. Quite apart from the personal and family impact for those directly affected, this represents a serious public health issue and a significant challenge to health care systems across the globe in terms of resource allocation. However, because those affected by rare diseases are seen in terms of their individual tragedy rather than as a collective need, their impact on the system is rarely appreciated by planners and service providers.
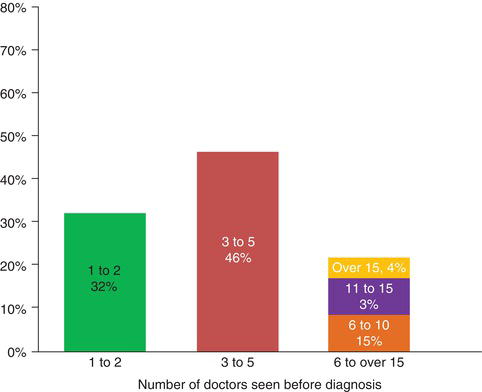
Addressing an issue of this magnitude might reasonably be expected to be seen as a priority by commissioners and those responsible for strategic decisions in health care. A recent survey by Rare Diseases UK of almost 600 families affected by over 100 different rare diseases [2] indicated that this does not seem to be the case. Families reported long delays before establishment of a diagnosis, with a significant minority waiting more than 5 years, and some never receiving a diagnosis at all. Equally disturbing is the fact that many patients receive a wrong diagnosis, sometimes more than once.
Figure 24.1 Chart: “How long did you/your family member have to wait for a final diagnosis following the onset of disease symptoms?” Source: Rare Disease UK survey on patients and family experiences of rare diseases. (http://www.raredisease.org.uk/documents/RDUK-Family-Report.pdf). Reproduced with permission from Genetic Alliance UK.
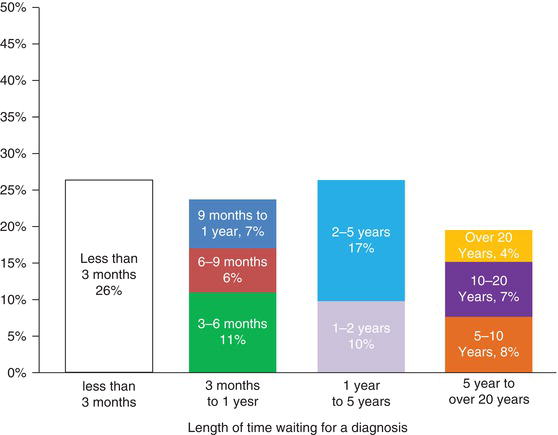
Given that 80% or more of rare diseases are genetic, arising from changes in a specific gene, this is an issue affecting whole families and across generations. Misdiagnosis means that potentially treatable conditions remain untreated, while others may be treated for conditions they do not have. This is unlikely to help alleviate symptoms; it wastes resources and allows potentially avoidable harm to continue.
Even when a correct diagnosis is made, the situation is not straightforward. Families with rare diseases often report significant difficulties in getting access to information about their condition that they can understand, and act upon in ways that will allow them to gain and retain a degree of control over their lives to the extent that they wish and that is possible given the realities of their condition and the wider context in which they live their lives.
Facing the challenges
Most rare diseases are complex. They affect different body systems and often have psychological as well as physical consequences. A small but growing number of rare diseases can be treated. For example, enzyme replacement therapy (ERT) has been developed for a few inborn errors of metabolism, but despite these examples of progress, it remains the case that the vast majority remain untreatable. In such cases, practical help with the day to day management of the different issues that arise can be invaluable in helping families to cope.
Peer to peer support, and the collected experience of what works (and what may not) is usually and effectively channelled through patient support organisations. Many of these have developed from the initial experiences of patients and affected families, and have evolved into highly effective providers of information, advice and support. One area where patient organisations have been particularly effective and influential is the inborn errors of metabolism, including the Lysosomal Storage Disorders (LSDs).
Figure 24.2 Chart: “How many doctors did you/your family member see before the final diagnosis was made?” Source: Rare Disease UK survey on patients and family experiences of rare diseases. (http://www.raredisease.org.uk/documents/RDUK-Family-Report.pdf). Reproduced with permission from Genetic Alliance UK.
The LSD Patient Organisation Collaborative was set up in the UK in 2008 by six founding members, each a pre-existing patient body representing patients with an LSD [Association for Glycogen Storage Disease; Batten Disease Family Association; Gauchers Association; MPS Society; Niemann–Pick Disease Group (UK); Representing Krabbe Leukodystrophy: Save Babies through Screening Foundation (UK)] to undertake joint promotion and a shared understanding of LSDs, to advance standards of care for LSD patients and to enhance the well-being of those affected. Their focus is to stimulate interest and work in partnership where groups can discuss matters of common interest, and establish criteria for the development and dissemination of good practice in looking after patients.
This collaborative effort has built upon the significant experience of individual organisations that have for many years provided specific disease information resources, family conferences, regional conferences, disease-specific expert meetings, focus groups and workshops. Some of the Associations, for example the MPS Society and the Niemann–Pick Disease Group UK, provide an individual advocacy service, which focuses on all aspects of social care and daily living, as well as palliative needs and pre- and post-bereavement.
Access to treatment
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree