24 Salvage Surgery after Primary Radiotherapy: Transoral Laser Microsurgery
Abstract
Radiotherapy (RT) is widely used as primary treatment for early-stage cancer of the larynx. In the case of persistent/recurrent cancer of the larynx after RT, different salvage treatments are to be considered: total laryngectomy, open partial laryngectomy, and transoral laser microsurgery (TLM). TLM is the first-line treatment for early and intermediate laryngeal cancer, but it can also be considered as salvage surgery after RT in selected cases. Candidates for salvage surgery should be chosen on the basis of careful clinical and radiological examination. Clinical examination should include detailed laryngoscopy, combined with MRI or CT scan of the larynx, even in the case of a superficial suspicious lesion. The selection criteria for TLM in recurrent cancer of the larynx are very strict. It is important to achieve a good exposure of the larynx with full visualization of the anterior commissure. Minimal cordectomies (e.g., I, II, or III) are not recommended. Hemilaryngectomy (types IV and V) is generally suggested, even for apparently superficial lesions because after RT it is not easy to detect the real boundaries of the tumor. Here we present two clinical cases in which the patients underwent TLM as salvage surgery after RT failure for cancer of the larynx.
24.1 Case Reports
24.1.1 Patient 1
A 77-year-old male patient presented to our clinic because of persistent dysphonia. He is a non-smoker and complains of “rough voice.” Eight months previously, he underwent radiation (66 Gy) for “cT1a” squamous cell carcinoma (SCC) of the larynx. Clinical records reveal type II diabetes, severe renal failure, and hypertension. Videolaryngoscopy shows a leukoerythroblastic lesion of the left vocal fold extending to the laryngeal ventricle; laryngeal mobility is mildly reduced. No lymph nodes are detected on the palpation of the neck.
A biopsy of the lesion was taken and the final histopathological examination was SCC.
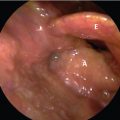
A neck and chest CT scan was performed, demonstrating enhanced areas at the level of the left vocal fold and anterior commissure (AC). The lesion extends to the left ventricle, without infiltration of the left paraglottic space (PGS). No cervical lymphadenopathy was detected. No suspicious pulmonary lesions were noted. The lesion was classified as yT2, N0M0 ( Fig. 24‑1 a).

The patient is intubated with a laser-safe tubing (Laser-Flex Tracheal Tube; Mallinckrodt Inc., St Louis, MO); a direct laryngoscopy evaluation with 30- and 70-degree rigid endoscopes revealed a lesion involving the left vocal fold, extending to the AC and the contralateral vocal fold. The tumor extended superiorly to involve the anterior one-third of the left false vocal fold ( Fig. 24‑1 b).
The exposure of the larynx was achieved by using a large bore laryngoscope. A type V left hemilaryngectomy was performed using a CO2 laser. “En bloc” resection of the cancer includes the left vocal fold, the false vocal fold, the anterior commissure, and the anterior two-thirds of the right vocal fold. The inner perichondrium of the thyroid cartilage was exposed in order to remove completely the PGS. Both arytenoids were preserved. For the procedure, a 25-W carbon dioxide laser (Martin, Tuttlingen, Germany) with an output power of 0.8 to 3.4 W in superpulse mode and with a beam width of 150 μm was used. Specimens are orientated, fixed in 10% buffered formalin for 24 hours, and paraffin embedded. Five-micrometer sections stained with hematoxylin and eosin. Resection margins stained with Indian ink. The final pathological results showed poorly differentiated SCC of the larynx, infiltrating the subepithelial connective tissue near the thyroid cartilage with a “close” (< 1 mm) margin at the level of the deep plane. All margins are free from neoplastic infiltration. After multidisciplinary discussion, the patient was referred to close follow-up and he is currently cancer free after 41 months of follow-up ( Fig. 24‑1 c).
24.1.2 Patient 2
A 72-year-old male patient was referred to our clinic because of persistent mild dysphonia. He is not a smoker and takes no medications. In 1994, he underwent radiation therapy (66 Gy) for a “cT1a” SCC of the right vocal fold. Three years later, he underwent type I cordectomy because of carcinoma in situ of the right vocal fold. Outpatient laryngoscopy reveals mild edema of the larynx. I-scan examination reveals a 4-mm submucosal lesion at the level of the right ventricle. No lymph nodes are detectable on palpation of the neck ( Fig. 24‑2 a).
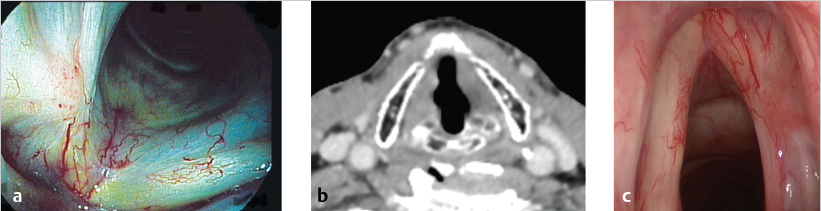
CT scan demonstrates mild asymmetry of the supraglottic region and a 4-mm submucosal lesion of the right ventricle. The PGS is unaltered, and there are no enlarged signs of infiltration of the laryngeal cartilages and lymph nodes were detected ( Fig. 24‑2 b).
The patient underwent microlaryngoscopy under general anesthesia. He was intubated with a laser-safe tubing (Laser-Flex Tracheal Tube; Mallinckrodt Inc.) and a direct laryngoscopy evaluation with 30- and 70-degree rigid endoscopes revealed a small submucosal lesion between the upper surface of the right vocal fold and the floor of the ventricle. Frozen sections on intraoperative biopsy confirms SCC ( Fig. 24‑2 c).
The exposure of the vocal folds and the AC is obtained with a large bore laryngoscope. A type IV right hemilaryngectomy was performed; “en bloc” resection of the cancer includes the right vocal fold and the false vocal fold. The inner perichondrium of thyroid cartilage is exposed in order to remove completely the PGS. Specimens are harvested as previously described in patient one. The final pathological results revealed an in situ SCC with all margins free of cancer. The patient is referred to follow-up and he is currently free from disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree