23 Locally Advanced Supraglottic Cancer: Organ-Preservation Protocol
Abstract
We describe a case of a man with a supraglottic laryngeal carcinoma stage T2N1 (stage III) treated with induction chemotherapy (cisplatin + paclitaxel), followed by radiation (RT) alone. Treatment goals of patients with limited-stage cancer of the larynx are: curing the cancer, preserving laryngeal functions, and maximizing the patient’s quality of life. Traditionally, primary treatment approaches, with equivalent outcome results, includes primary larynx-preserving surgery, when feasible, followed by RT or chemoradiation in high-risk cases or as an alternative option a combination of chemoradiation and radiation therapy. Treatment choice aim at maximizing in the patient organ function, quality of life, and overall. In this situation, the optimal decision-making requires an experienced multidisciplinary team for initial evaluation, response assessment as well as supportive care, and rehabilitation during and after treatment. In addition to the extent of the tumor, pretreatment laryngeal function, coexisting chronic disease, and patient expectations are critical factors in selecting surgical or nonsurgical primary treatment.
23.1 Case Report
A 67-year-old Caucasian male presented in another hospital with left laterocervical adenopathy where he was followed by hematologists for monoclonal gammopathy of undetermined significance (MGUS) immunoglobulin Mκ (IgMκ). An excisional biopsy of the lymph node was performed. The pathological report described a squamous cell carcinoma (G2). He stated that he was a 45 pack year cigarette smoker, and had a history of alcohol abuse with chronic liver disease (steatosis grade 1).
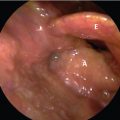
At the time of our consultation, the patient was healthy; he had a transverse scar on the left neck and a new lymph node of 3cm in the left neck. A direct laryngoscopy revealed a vegetant lesion of the lingual surface of the epiglottis that also involved the left glossoepiglottic vallecula. The lesion reached to and infiltrated the right pharyngeal epiglottic fold without vocal cord fixation.
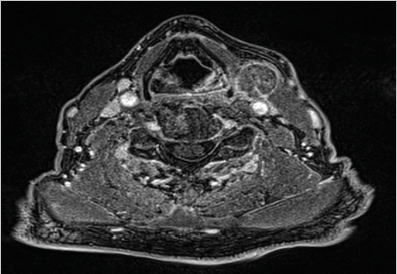
We performed an MRI scan that showed a lesion occupying the left glossoepiglottic vallecula, the lingual surface of the epiglottis without infiltration of the base of tongue, aryepiglottic fold, or piriform sinus. There was a left submandibular lymph node of 23 × 19 mm.
Due to the past smoking history and presence of comorbidities possibly associated with occurrence of secondary primaries, we completed the staging with a PET scan that confirmed the locoregional extension of the tumor and no distinct metastatic disease. We concluded that the tumor was cT2N1M0, stage III, according to the seventh edition of the American Joint Committee on Cancer (AJCC; Fig. 23‑1).
We examined the patient in our multidisciplinary clinic. A surgical conservation approach was excluded due to the extent of the cancer. An organ-preservation protocol was offered to the patient. The patient started chemotherapy with paclitaxel plus cisplatin 3 weekly treatment for three cycles. The treatment well tolerated except for a grade 2 neutropenia after the first cycle and no other side effects.
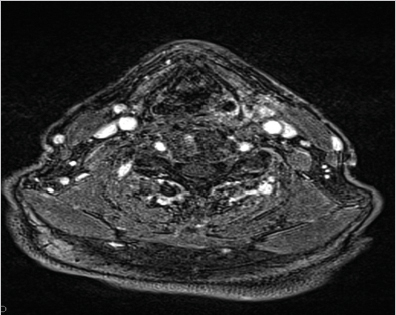
We repeated the MRI scan after two cycles of chemotherapy and with a 70% reduction in the size of the cancer according to Response Evaluation Criteria In Solid Tumors (RECIST) criteria. 1 Vocal cord mobility was maintained. In larynx preservation (LP) trials, a response to induction chemotherapy of more than 50%, along with cord remobilization, was the standardized criterion used for selecting patients for radiation, thus allowing for organ preservation ( Fig. 23‑2).
After the third cycle of chemotherapy, the patient started radiotherapy alone; he received intensity-modulated radiotherapy (IMRT) to a total dose of 69.96 Gy in 33 fractions on tumor and adenopathy (left level II); in particular, supraglottic larynx and left II to III neck level received 61.05 Gy in 33 fractions; larynx plus bilateral neck received 54.45 Gy in 33 fractions.
Radiotherapy was well tolerated. He had grade 2 mucositis and grade 1 dysphagia. The treatment ended in September 2015. After three years, the patient is alive and free of cancer with no report of any late symptoms such as dysphagia and dysphonia. In January 2018, he developed a postradiation hypothyroidism and replacement therapy was started.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree