21 Locally Advanced Glottic Cancer: Total Laryngectomy and Voice Prostheses
Abstract
Patients with advanced cancer of the larynx should be adequately counseled about the different treatment options (radiotherapy, chemoradiotherapy, or a total laryngectomy), in terms of both overall survival and expected quality of life. Patients with a T4 cancer have higher overall survival rates after a primary total laryngectomy, although an increasing number of patients are treated with organ-preservation protocols. Rehabilitation is crucial in obtaining a good voice and quality of life.
21.1 Case Report
A 66-year-old male patient was referred to our outpatient clinic at the Netherlands Cancer Institute in Amsterdam with progressive dysphonia during the previous 3 months. The referring Otolaryngologist identified a lesion suspicious for squamous cell carcinoma, which was proved by biopsy. In the Netherlands, head and neck oncology care is centered in dedicated head and neck centers, so the patient was referred to us. The patient had a history of smoking cigarettes but had stopped 10 years ago. He used alcohol moderately. Besides taking oral medication for his diabetes, he was otherwise healthy and had no prior surgery. Adult Comorbidity Evaluation 27 (ACE-27) comorbidity score was 1.
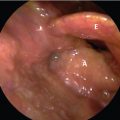
Videolaryngoscopy with stroboscopy revealed a red, irregular right true vocal cord, with no mucosal wave pattern but only slightly diminished mobility ( Fig. 21‑1). The tumor seemed limited to the true vocal cord and was clinically staged as T2N0.
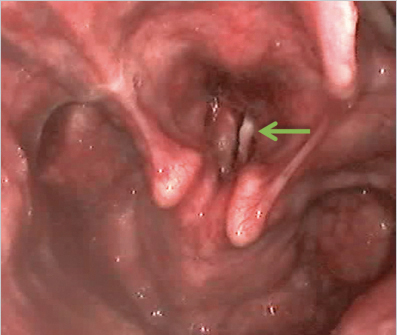
Though clinically thought to be a relatively small cancer, CT scan demonstrated a bulky tumor of the right vocal cord, crossing the anterior commissure to the left vocal cord ( Fig. 21‑2). The tumor expanded outside the thyroid cartilage on both sides and there was obliteration of adipose tissue between the thyroid cartilage and strap muscles. There was no subglottic extension and no suspicious lymph nodes were seen. The maximal diameter was 4.3 cm.
Direct laryngoscopy under anesthesia showed a nonulcerative tumor extending from the anterior commissure toward the anterior two-thirds of the right true vocal cord and anterior first one-third part of the left vocal cord. On the right surface, the cancer grew into the sinus of Morgagni and toward the false vocal cord. Via the anterior commissure, there was extension toward the laryngeal side of the epiglottis. No subglottic extension was noted. The cancer was staged as T4aN0 transglottic.
After discussing the results in our multidisciplinary Tumor Board meeting, the results were shared with the patient. The three options of total laryngectomy (TL) plus adjuvant radiotherapy (RT), concomitant chemoradiotherapy (CRT), and primary RT were discussed, where he was informed that TL + RT was associated with the highest overall survival. Based on the expected higher overall survival after TL, he opted for the surgery.
Two weeks later, he underwent a TL with selective neck dissection of levels II to IV bilateral, sparing the sternocleidomastoid muscle, internal jugular vein, and the spinal accessory nerve. After general anesthesia and perioperative administration of cefazolin and metronidazole, a modified Gluck–Sorenson incision was made and a separate incision for the stoma was created 2 cm beneath the incision line. The dissection was carried deep from the platysma muscle creating cranial and caudal myocutaneous flaps. The right neck dissection was carried out first. The anterior border of the sternocleidomastoid muscle was used as a reference point and the great auricular nerve was found and spared. The sternocleidomastoid muscle was skeletonized and the omohyoid muscle was identified. Dissection proceeded to the posterior edge of the sternocleidomastoid muscle where the deep cervical muscles and the cervical plexus were identified. the deep cervical muscles and the cervical plexus. Carefully dissecting all fatty tissue over the plexus and muscle and over the internal Jugular vein, Carotid artery and Vagal nerve we proceeded in dissecting the specimen towards to the larynx. The internal Jugular vein, the Accessory nerve and Hypoglossal nerve were spared. A similar procedure was performed on the left side. There was some chyle leakage caudally, which stopped after clipping the thoracic duct. The strap muscles were subsequently dissected. The superior thyroid arteries on both sides were dissected and the thyroid gland isthmus was left on the specimen, but both lateral lobes were separated from the larynx and preserved.
The hyoid bone was then skeletonized at the cranial side and the pharyngeal constrictor muscles were seperated from the posterior edge of the thyroid. The trachea was divided in a horizontal plane below the second tracheal ring. The tracheal tube was removed and a new ventilation tube was placed in the trachea. The larynx was then opened in the vallecula and the larynx was removed preserving as much of the mucosa as oncologically safe. The wound was irrigated with distilled water and the patient was re-draped.
The trachea, with an intact third tracheal cartilage ring, was meticulously sutured into the skin, making sure the cartilage was covered with skin. Using the Vega puncture set, a Provox Vega 22.5-Fr-width, 8-mm-long voice prosthesis (VP) was placed. A pharynx protector, puncture needle, and guidewire allowed for an easy placement of the VP. To prevent spasm, a myotomy of the upper esophageal constrictor muscle was performed, as well as a myotomy of the sternal head of the sternocleidomastoid to create a flat stoma in the neck. A nasogastric feeding tube was inserted. The pharynx was closed with absorbable Vicryl 3–0 sutures in two layers in a T-shape. The mucosa was sutured with inversion of the mucosa (Connell type) and subsequently a hemiclosure of the crico- and thyropharyngeal muscles from one side over the suture line was performed, after which fibrin glue was placed on the suture line. The lobes of the thyroid gland were sutured on the neopharynx to model a flat stoma. Two drains were placed through separate incisions, making sure the drains were not lying over the pharyngeal closure. The skin was then closed in two layers. An adhesive with heat and moister exchanger (HME) was placed and no cannula was used postoperatively. The patient was monitored for one night in the intensive care unit.
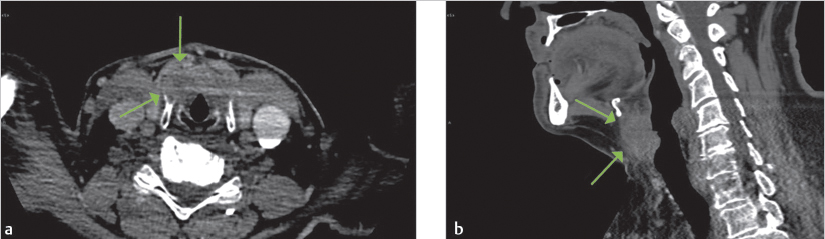
Initially, the patient experienced an uncomplicated recovery; only minor shrinkage of the stoma occurred for which he received a LaryTube silicon cannula. After 24 hours, the patient started drinking water and after 48 hours a liquid diet was started. However, a barium swallow examination on postoperative day 7, revealed extraluminal contrast fluid at the superior suture line. Oral intake was then stopped and antibiotics treatment started. A second barium-swallowing examination on day 14 showed a fistula tract to the stoma ( Fig. 21‑3). The patient was treated conservatively with nothing per mouth and a cuffed cannula. Six days later, the barium swallow examination was repeated that showed only a small sinus tract. After another 6 days, the barium swallow examination showed complete recovery and the patient was able to resume oral intake and start voicing. A few days later, he was able to consume a full diet and produce intelligible sound with his VP and was discharged from the hospital.
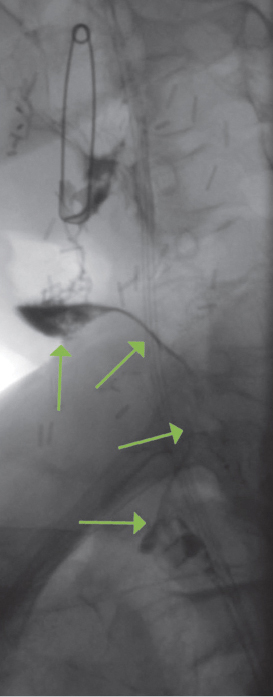
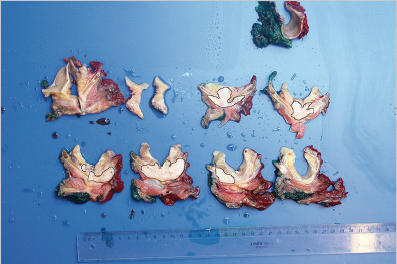
The histopathological report revealed a moderately differentiated squamous cell carcinoma invading the cartilage and extending extralaryngeal but without perineural or vascular invasion growth. Resection margins were free from cancer and no cervical lymph node metastases were found. Staging was pT4N0 according to the TNM-7. Fig. 21‑4 illustrates how only a small portion of the cancer was growing in the laryngeal lumen and the bulk of the cancer is situated in the cartilage and beyond. This explains why the patient had only minor complaints and clinically the cancer was staged as a T2 glottis cancer of the larynx. The patient received adjuvant RT on the larynx using intensity-modulated radiotherapy (IMRT) in 33 fractions of 2 Gy to the laryngeal area and 46 Gy electively to the neck.
21.1.1 Quality of Life
The patient tolerated the RT very well without any toxicities. He maintained oral intake and an adequate voice. Since his surgery, he had five VP replacement for transprosthetic leakage and his median device lifetime was 46 days. Because of this limited lifetime, he was offered an ActiValve light, which is still in situ now counting 261 days. He uses Provox ExtraBase FlexiDerm adhesives that generally stay on for 1 day with an HME ( Fig. 21‑5). He cannot use an automatic speaking valve because the adhesive does not tolerate the pressure.

As part of our standard care, several quality-of-life questionnaires such as the European Quality of Life-5 Dimensions 5 level questionnaire (EQ-5D-5L), 1 the Voice Handicap Index-10 (VHI-10), 2 and the swallowing screening tool (EAT-10) 3 were given to the patient before treatment and 3 months, 6, months, and 1 year after treatment. On the EQ-5D, a standardized measure of health status, he scored a self-rated health status of 80/100 preoperatively, which increased to 100/100 3 months postoperatively. Six months after treatment, he is very independent, still walking on average 2 hours per day. He does have some trouble being fast and witty in big groups but still is satisfied with his voice, physical functioning, and social functioning. His voice was evaluated using the VHI-10, an instrument to quantify patients’ perception on their voice handicap. The scores ranges from 0 (no problems at all) to 40 (having trouble on all aspects all the time). Preoperatively he scored 22/40, which decreased to 3/40, 3 months postoperatively. One year after treatment, his health status scored 100/100 and his VHI-10 decreased to 2/40, only scoring that because sometimes people ask him what is wrong with his voice. The patient did not report any swallowing problems on the EAT-10 questionnaire before treatment nor 1 year after treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree