2 Radiotherapy for T1a Glottic Cancer
Abstracts
Primary radiotherapy (RT) for T1a cancer of the glottis is a highly effective treatment resulting in excellent outcomes. Treatment with primary RT for early-stage vocal cord cancer allows for voice preservation with a tolerable toxicity profile. For T1a cancer of the glottis, the recommended RT dose schedule is 63 Gy at 2.25 Gy per fraction once daily using a three-field technique.
2.1 Case Presentation
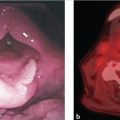
A 68-year-old male with a 40 pack-year history of smoking cigarettes presented for medical attention for persistent hoarseness lasting 5 months. After a course of oral antibiotics did not improve symptoms, he was referred to an otolaryngologist. On physical examination, there was no cervical adenopathy on palpation and examination of the oral cavity did not reveal any abnormal lesions. Flexible laryngoscopy demonstrated a white nodular lesion on the anterior one-third of the right true vocal cord (TVC). The left TVC was mildly edematous but without visible tumor. The TVCs had normal mobility ( Fig. 2‑1).

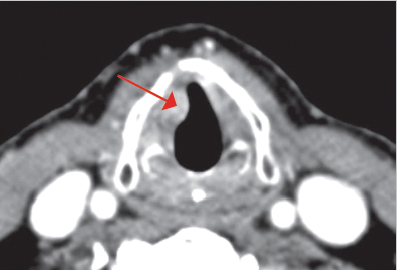
An axial computed tomography (CT) scan, with contrast of the larynx demonstrated an infiltrating mass involving the anterior one-half of the right TVC without extension to the midline at the anterior commissure ( Fig. 2‑2). There was no invasion of the thyroid cartilage and no extension into the subglottic region. No abnormal cervical or supraclavicular adenopathy was present and CT imaging of the chest was negative for pulmonary metastasis. Direct micro laryngoscopy under general anesthesia confirmed the absence of subglottic extension.
A biopsy of the right TVC was performed and the pathology report revealed a moderately differentiated squamous cell carcinoma. As per the eighth edition of the American Joint Committee on Cancer (AJCC) staging system, the disease was staged as a clinical T1a N0 M0 squamous cell carcinoma of the right TVC.
Treatment with primary external-beam radiotherapy (EBRT) was recommended. The patient received a total dose of 63 Gy at 2.25 Gy per fraction once daily. A three-field technique with 6-MV photons was used to deliver approximately 95% of the dose through opposed lateral wedged fields weighted to the side of the lesion; the remaining dose was delivered by an anterior field shifted 0.5 cm toward the side of the lesion. The tumor dose was specified to the 95% normalized isodose line ( Fig. 2‑3).
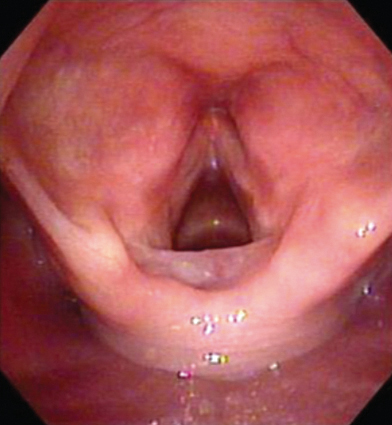
At the time of follow-up 1 year after treatment, examination using the flexible laryngoscope demonstrated bilateral TVCs without edema, lesions, or asymmetry. Bilateral vocal cord mobility was normal. The patient’s voice had returned to normal. There were no late treatment toxicites.
2.2 Discussion
2.2.1 Clinical Presentation, Staging, and Diagnostic Evaluation
Most lesions of the TVC begin on the free margin and superior surface of the vocal cord. When diagnosed, about two-thirds are confined to the cords, typically one cord. Per the eighth edition of the AJCC staging system for primary laryngeal cancer, T1 glottic cancer is defined as a cancer limited to the vocal cord(s) (that may involve the anterior or posterior commissure) with normal mobility. T1 cancers are stratified into those involving one vocal cord (T1a) and those involving both vocal cords (T1b). 1
Cancer arising on the TVC most commonly produces hoarseness at an early stage. Odynophagia, otalgia, pain localized to the thyroid cartilage, and airway obstruction are all features of advanced lesions. Diagnostic evaluation includes the following: a physical examination of the head and neck region, flexible fiberoptic endoscopy to best visualize the larynx, a CT scan with contrast enhancement of the larynx and neck, and a direct laryngoscopy with biopsy performed with the patient under general anesthesia.
2.2.2 Treatment Options
In treating cancer of the vocal cord, the goal is cure with the best functional result and the smallest risk of a serious complication. Patients who have early stage cancer, including those with T1a cancer, should receive larynx-preserving treatment, 2 which includes primary RT or surgery by transoral laser microsurgery (TLM) or transoral robotic surgery (TORS). 3
At many treatment centers, RT is the initial treatment prescribed for T1 cancer of the glottis, with surgery reserved for salvage if there is a local recurrence occurs. 4 , 5 , 6 The major advantage of RT compared with partial laryngectomy is a better quality of voice preservation. However, it is important to note that primary surgery with TLM and TORS has shown comparable cure rates when compared to primary RT. 5 , 7 , 8 The advantages of surgery include avoidance of RT, a single treatment, and potential cost-effectiveness.
Most recurrences appear in the first 2 years after treatment, but late recurrences may appear even after 5 years. However, the latter instance may actually be a second primary cancer. If a patient recurs locally after primary RT, they may be salvaged by cordectomy, hemilaryngectomy, supracricoid partial laryngectomy, or total laryngectomy. Open partial laryngectomy and total laryngectomy are the most commonly used surgical salvage procedures.
If a patient recurs after primary surgery, salvage with RT may be possible. If a patient recurs after a combination of RT and partial laryngectomy, total laryngectomy may still be a successful option for salvage.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree