Prognostic Markers and Models in Acute Lymphoblastic Leukemia
University Hospital, Frankfurt am Main, Germany
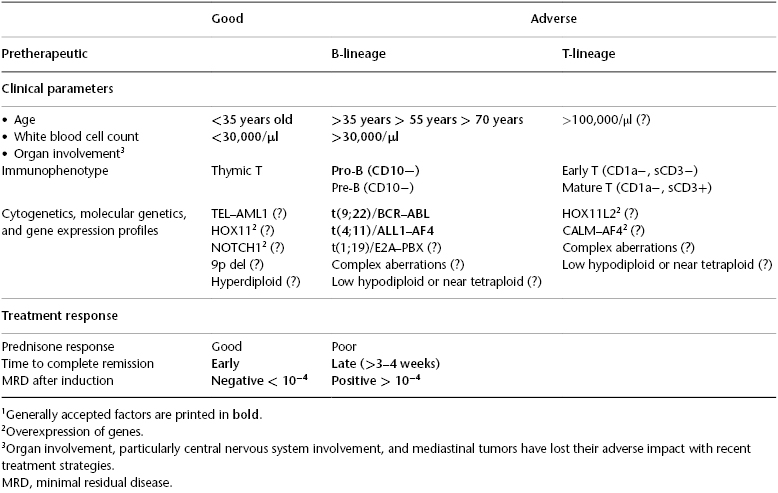
Acute lymphoblastic leukemia (ALL) is not a uniform disease but is characterized by subgroups with different biological and clinical features and cure rates. They have prognostic impact for either the achievement of remission or the remission duration. There are two phases to evaluate prognostic factors: the first are the patient characteristics at diagnosis, and second is the response to treatment (Table 2.1). Pretherapeutic prognostic features are age, initial white blood cell count (WBC), immunophenotype, and abnormal cytogenetics or molecular genetics. Response parameters are achievement of complete remission (CR), now molecular remission (MolCR), and time to achieve a CR and MolCR. The aim of evaluating prognostic factors in ALL is to stratify patients into good and poor risk groups and to adapt different treatment strategies accordingly. The most important decision in adult ALL is, thereby, whether a patient should have a stem cell transplantation (SCT) in first remission or not.
Table 2.1 Prognostic factors for risk stratification of adult acute lymphoblastic leukemia (ALL)1.
Pretherapeutic Prognostic Markers
Age
• What is the prognostic value of the age of an adult ALL patient, and what are the therapeutic implications?
• Is there a best age cut-off?
Increasing age is undoubtedly associated with poorer outcome in all studies. The earlier defined age cut-off of 35 years was the best dichotomy in the survival curve, and was oriented on the age limit for allogeneic stem cell transplantation (allo-SCT) at that time. This age limit is still of relevance, but with a different therapeutic consequence; recently applied pediatric-inspired protocols for adolescents and young adults (AYAs) are applicable up to an age of 35 to 40 years, and beyond that are associated with an unacceptable toxicity. Patients older than this age limit have a substantially poorer outcome and an increasing incidence of adverse risk factors.
White Blood Cell Count
• Does WBC at diagnosis still have a prognostic impact?
• Is the WBC still of prognostic relevance with the cytogenetic and genetic markers now available?
Elevated WBC at diagnosis (>30,000–50,000/ml) as a poor prognostic feature has been confirmed in various trials. It was even considered as the most deleterious prognostic factor in B-precursor ALL with overall survival of 19–29%. The biological reason for the highly resistant behavior of B-precursor ALL with high WBC is unclear. Probably in the future, additional molecular markers can help to clarify the underlying mechanisms. Due to the high relapse rate evaluation of minimal residual disease (MRD), the use of experimental drugs and SCT modalities seems particularly important.
Cytogenetic and Genetic Markers
• Are cytogenetic and genetic markers relevant for treatment decisions?
Yes, absolutely. Philadelphia chromosome–positive ALL with the t(9;22) translocation and the BCR–ABL fusion transcript is the most frequent cytogenetic abnormality in adults, which accounts for 25% of all adult B-lineage ALLs, with a strong age-related incidence, increasing from <3% in children up to 40–50% in adults aged >50–60 years. Ph+ ALL was so far the poorest ALL subtype, with a CR rate of ∼70% and a survival rate at 5 years of <10% with chemo and <30% with allo-SCT. Targeted therapy with tyrosine kinase inhibitors (TKIs) directed against the BCR–ABL fusion transcript has changed the perspective completely; CR rates are now >90% and survival >50%. This demonstrates convincingly that prognostic factors are changing with therapy, and thus risk group stratifications and treatment algorithms need constant refinement.
Immunophenotype
Immunologic subtypes are not only associated with different clinical presentations but also partly associated with distinct cytogenetic and/or molecular aberrations and with prognosis. The expression of surface antigens is of increasing importance for targeted therapy with monoclonal antibodies.
• Is there a difference in the prognostic impact of B-lineage ALL versus T-lineage ALL, and is it justified to have different treatment approaches?