19 Hemicricolaryngectomy with Tracheal Autotransplantation
Abstract
Tracheal autotransplantation is a reconstructive technique that allows for organ-sparing treatment of selected patients with advanced cricoid cartilage chondrosarcoma and T2 or T3 laryngeal squamous cell carcinoma (SCC; unilateral T2 with impaired vocal fold mobility; T3 with subglottic extension and/or arytenoid cartilage fixation). For this particular group of patients, our tracheal autotransplantation technique provides excellent functional results for respiration, speech, and swallowing without compromising the oncologic outcome. This is particularly true for patients younger than 65 years and for those with cricoid chondrosarcoma.
19.1 Case Report
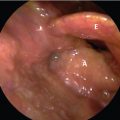
A 54-year-old male patient presented with a T3N0 unilateral glottic squamous cell carcinoma (SCC) with involvement of the arytenoid and with infraglottic tumor extension. The lesion did not extend to the ventricle. Two years earlier, he received radiation therapy for a T1N0 glottic SCC. His pulmonary function test was within the normal range. The patient had no other comorbidities.
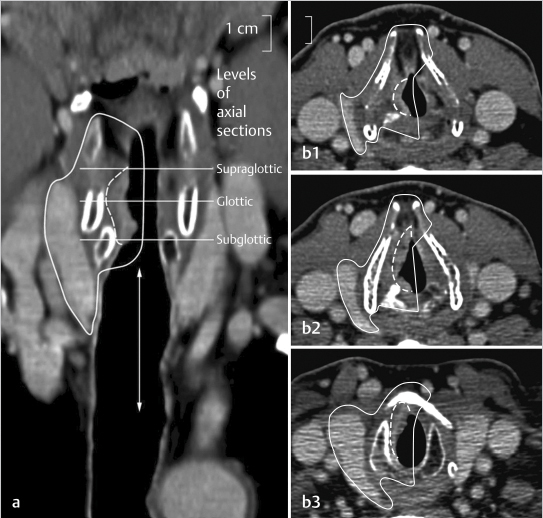
An extended hemicricolaryngectomy with tracheal autotransplantation was performed in this patient. An overview of the tumor extent and the amount of resection is depicted in Fig. 19‑1 .
19.1.1 First Operation
The operation began with a lateral selective neck dissection (levels II–IV) 1 with inclusion of one an ipsilateral thyroidectomy. A hemilaryngectomy with inclusion of half of the cricoid cartilage was performed ( Fig. 19‑2).
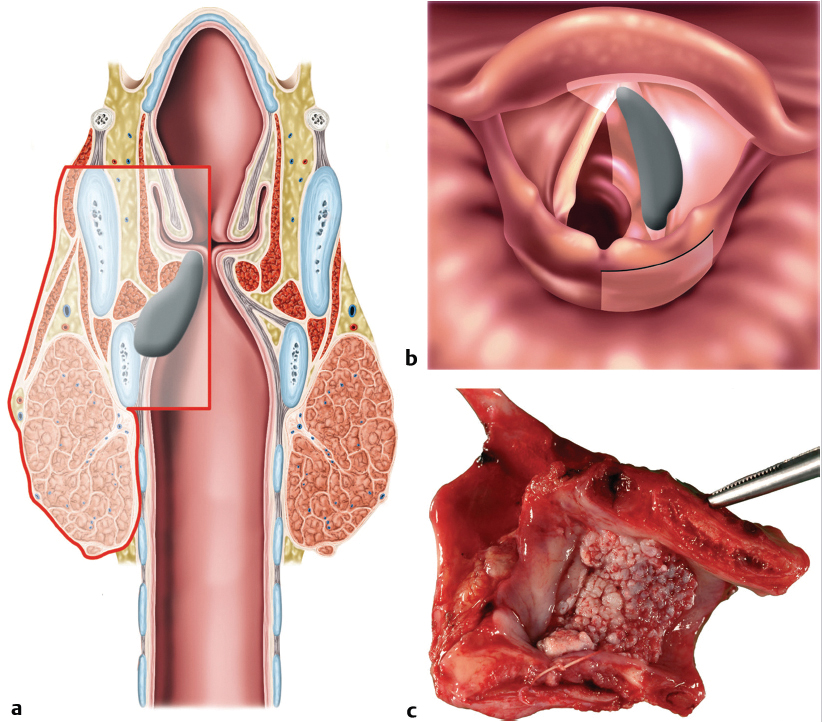
After tumor resecting the cancer, the cervical trachea was wrapped with the radial forearm subcutaneous tissue and fascia with the aim of fabricating a transplantable tracheal patch, axially vascularized by the radial forearm flap (RFF) pedicle. The hemilaryngeal defect was repaired temporarily with the radial forearm skin paddle. A tracheostomy was necessary for respiration ( Fig. 19‑3).
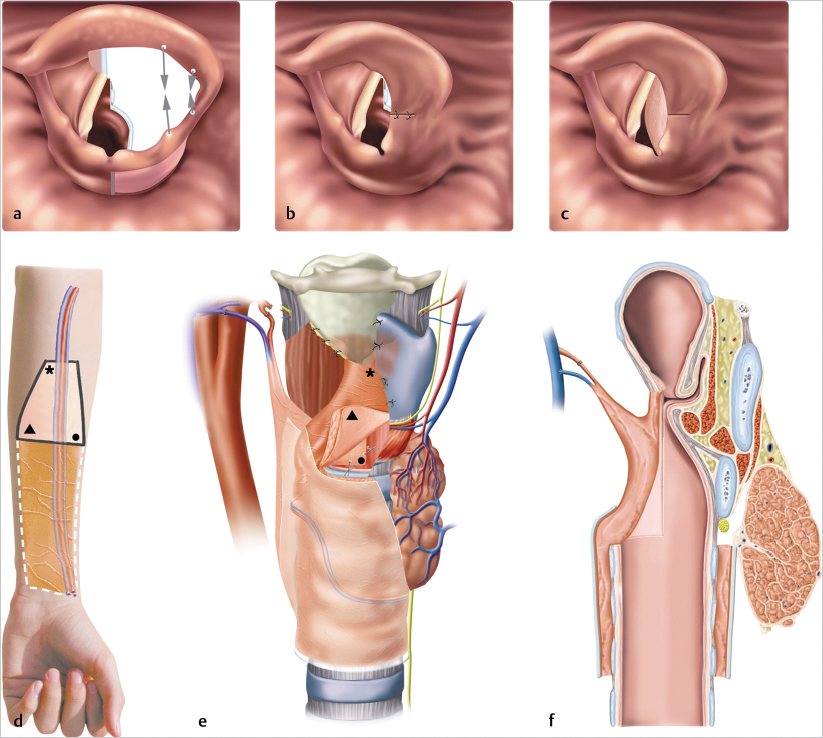
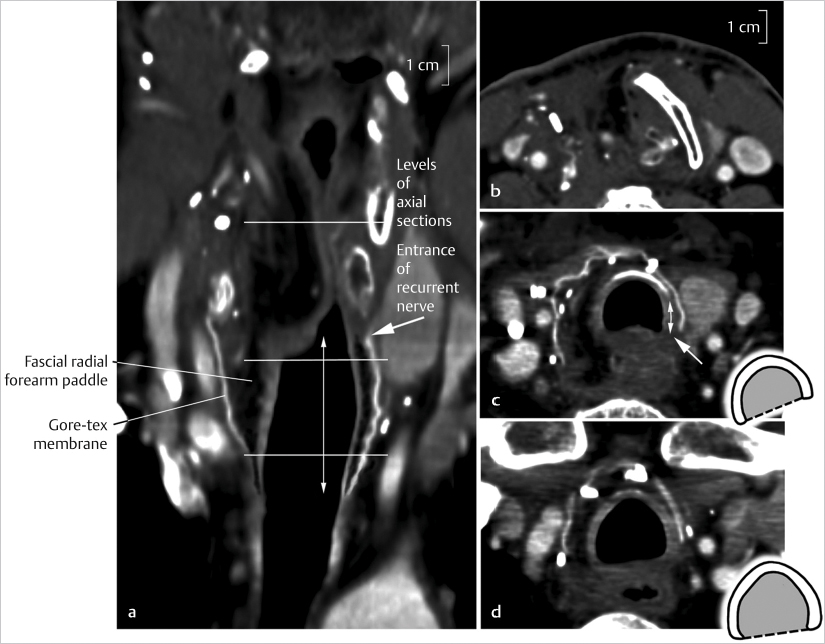
The sphincteric function after resection was restored by closing the gap between preserved aryepiglottic fold and epiglottis at the side of resection and by using the skin paddle of the RFF as a buttress for apposition ( Fig. 19‑3 a). The aryepiglottic fold allowed for a posterior midline reconstruction at the glottic and supraglottic level. After this intervention, the patient could close the glottic chink during speech and swallowing. A CT scan after 2 weeks illustrates the first step in the reconstruction process ( Fig. 19‑4).
At this point, the tracheostomy remains necessary for respiration. In the immediate postoperative period, first the nurses and after a few days the patient aspirated his own secretions using the bedside hospital suction system. Frequent suctioning through the tracheostomy tube was indicated to evacuate pulmonary secretions. Oral alimentation was begun after 1 week.
The histopathological report confirmed a T3N0 SCC. Resection margins were tumor free.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree