17 Locally Intermediate Supraglottic Cancer: Supracricoid Laryngectomy with Cricohyoidopexy
Abstract
The case of a 56-year-old patient with glottic and supraglottic carcinoma is presented as an example of supracricoid laryngectomy with cricohyoidopexy. The surgical technique is outlined, comprising the main steps to execute the procedure correctly. Important a natomical landmarks are presented and correlated with the steps of the technique. The goals of larynx preservation surgery are discussed after a brief introduction remembering the overindication of chemoradiation during the 1980s and 1990s. Indications and contraindications for the procedure are discussed and a series of tips are given, including the indications, limits for this surgery concerning the amount of subglottic extension, the importance in preserving both arytenoid cartilages whenever possible, reconstruction using sutures folding the hypopharyngeal mucosa, and the importance of frozen section intraoperative examination. Possible traps included the indication in patients with chronic obstructive pulmonary disease (COPD), previously irradiated patients, the insertion of the feeding tube before the closure of the pharynx, and the position of the skin incision for the tracheostomy.
17.1 Case Report
A 56-year-old Caucasian male painter, presented with a history of dysphonia for 6 months, followed by cough and odynophagia. He smoked, two packs of cigarettes per day for the last 20 years, and was a moderate alcohol drinker. He had no comorbidities.
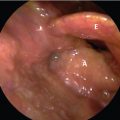
During the consultation the patient appeared to be healthy and had an obvious hoarse voice. No lesions were found in the nasal and oral cavities. Laryngoscopy revealed an ulcerated and infiltrative lesion involving the anterior commissure and the anterior half of both true vocal folds ( Fig. 17‑1). Superiorly, the lesion infiltrated the false vocal cords and the epiglottic petiole. Both vocal cords were mobile and the subglottis were not easily visible. There were no palpable lymph nodes and the laryngeal crepitation was present bilaterally.
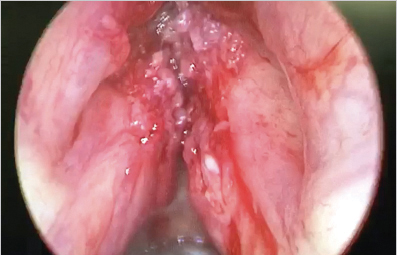
Due to the difficulty in evaluating the subglottis, the patient underwent direct rigid laryngoscopy under general anesthesia for better evaluation of the lesion. This procedure revealed an extension of the tumor with a vegetative characteristic toward the subglottis on the right side ( Fig. 17‑2). Biopsies were taken and the histopathological examination showed a moderately differentiated squamous cell carcinoma.
The therapeutic proposal was a supracricoid laryngectomy (SCL) with cricohyoidopexy (CHP). A large horizontal cervical incision was performed with subplatysmal flaps to provide an operative field with good visualization of the structures. The sternohyoid and omohyoid muscles were transected bilaterally at the superior border of the thyroid cartilage. The sternothyroid muscles were transected at the inferior border of the thyroid cartilage. A bilateral Tapia maneuver was then performed bilaterally by transecting the constrictors of the pharynx which released the pyriform sinuses.
The cricothyroid joint was then disarticulated in a subperichondrial plane being careful to preserve the recurrent laryngeal nerves. The isthmus of the thyroid gland was transected.
The periosteum of the hyoid bone was incised along its inferior aspect bilaterally allowing the release of the thyrohyoid membrane, hyoepiglottic membrane, and the pre-epiglottic space that will be removed with the specimen. The suprahyoid muscles were not transected. Using blunt dissection, the trachea was released along its anterior wall inferiorly to allow its upward motion at the time of the closure.
An entry to the larynx was made on the left side of the cricothyroid membrane (because there was evidence of subglottic extension on the right side). At this time, the orotracheal ventilation tube was removed and another one was inserted in the cricothyrotomy. A transvallecular horizontal approach was performed and the epiglottis was retracted anteriorly. Sections were carefully made along the pharyngoepiglottic and aryepiglottic folds for visualization of the tumor and clear margins.
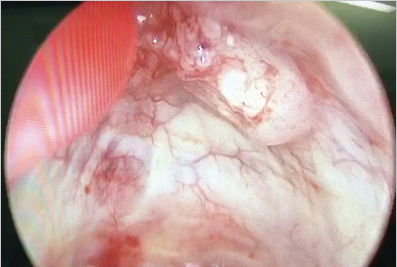
From the superior aspect of the cricoid cartilage, incisions using scissors were made toward the arytenoid cartilages that were preserved by the vocal processes. The entire paraglottic space was then removed with the thyroid cartilage after using scissors were made connecting with the cricothyrotomy previously made and the specimen was removed ( Fig. 17‑3).

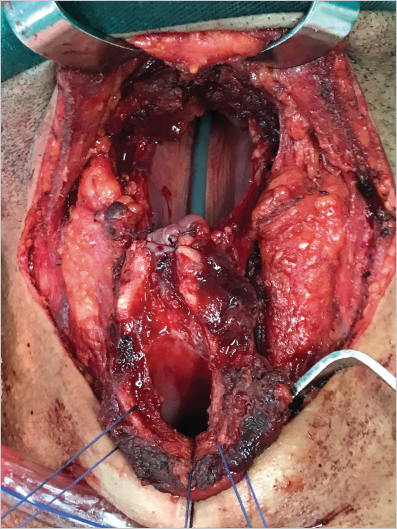
Three sutures of 1 Vicryl were applied between the overlying retrocricoid mucosa to elevate the cricoid cartilage and made a pexy with the hyoid bone ( Fig. 17‑4). The tracheostomy was placed at the level of the skin incision while the assistant tightened the central suture without tying it ( Fig. 17‑5). No sutures were needed to close the pharynx.

The pathology report revealed a moderate differentiated squamous cell carcinoma with clear margins. The patient’s postoperative course was satisfactory and the tracheostomy was plugged on the 20th postoperative day and removed on the 25th day. The nasoenteral feeding tube was removed on the 31st day.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree