16 Locally Intermediate Supraglottic Cancer: Radiotherapy
Abstract
The present case of T3N0 cancer of the supraglottic larynx highlights some of the issues related to nonsurgical organ-preservation strategies. In particular, we discuss the importance of pretreatment functional evaluation, proper patient staging and, the role of chemotherapy in addition to radiotherapy and its timing, as well as some of the planning/technical issues of radiotherapy. Unfortunately, the majority of clinical data on organ preservation with nonsurgical approaches have been obtained in patients who were candidates for total laryngectomy and without a formal evaluation of pretreatment laryngeal function, limiting their applicability to current practice. Highly destructive/extensive/circumferential cancers, even if still staged as T3, may not be good candidates for laryngeal preservation and patients should be specifically counseled. Regarding the role of chemotherapy, its addition to radiotherapy has been shown to provide improved organ preservation rates over radiotherapy alone, though the timing of the chemotherapy remains controversial. For a T3N0 cancer of the supraglottis, radiotherapy should deliver a definitive dose to the larynx and cover electively the neck at levels II to IV bilaterally. Intensity-modulated radiotherapy allows the dose of radiation to organs outside the target to be minimized and the one on structures that are (even only partially) “embedded” within the target (and its expansion at planning), such as the constrictor muscles and the thyroid gland, to be “controlled.”
16.1 Case Report
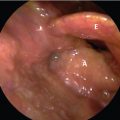
A 71-year-old cigarette smoker without significant comorbidities and with a 6 month history of progressive dysphonia was referred to our clinic. He denied dysphagia, pain, and weight loss. He recently consulted an Otolaryngologist who found an ulcerative lesion in the right supraglottic larynx. Physical examination revealed an approximately 2-cm ulcerative lesion involving the entire right false cord associated with edema and reduced mobility of the right hemilarynx was noted. The glottis and the right piriform sinus was unremarkable. ( Fig. 16‑1).
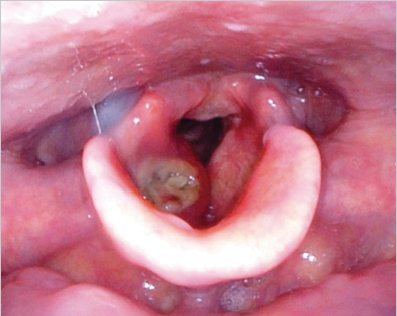
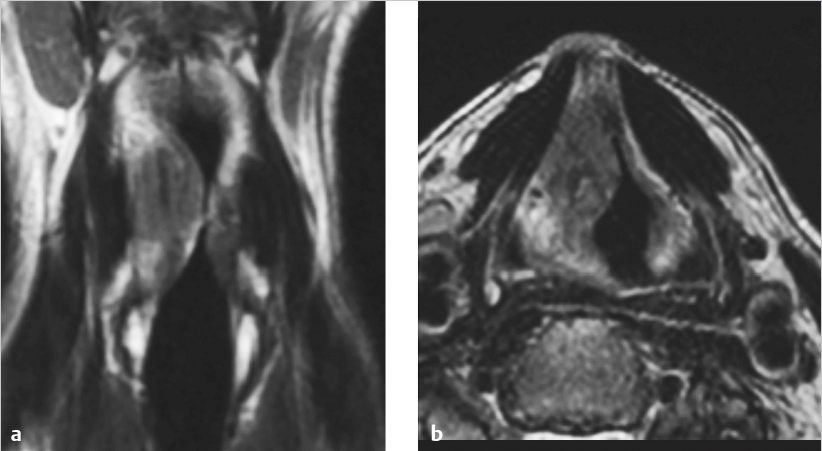
A biopsy was taken, which revealed nonkeratinizing squamous cell carcinoma. He completed the locoregional staging with an MRI, which demonstrated a 3-cm lesion centered in the right false vocal cord, involving the paraglottic space without erasion of the thyroid cartilage erosion. There were no signs of contralateral spread or involvement of either the pre-epiglottic space (PES) or the arytenoid ( Fig. 16‑2).
The neck was negative on both palpation and imaging. The lesion was staged as cT3N0M0 (CT chest). The patient discontinued smoking shortly after the diagnosis was made. Before deciding treatment options, the patient underwent a speech pathologist examination (FEES) that revealed no signs of penetration/aspiration. Moreover, the patient was cleared for both a conservation surgical approach (pulmonary function tests) and chemotherapy. Therefore, after multidisciplinary discussion, the patient was offered two options: supracricoid laryngectomy + bilateral elective neck dissections or definitive chemoradiotherapy. The patient opted for the latter.
A CT scan with the head hyperextended was obtained at simulation. The patient was instructed to breathe quietly and to avoid swallowing. The entire larynx and levels II to IV on both sides were contoured. The prescription doses were 70 and 58.1 Gy for the volume containing macroscopic and microscopic disease, respectively, in 35 fractions ( Fig. 16‑3).
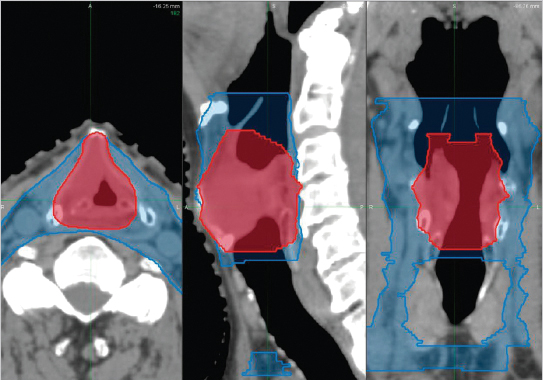
Seven-field intensity-modulated radiotherapy (IMRT) with 6-MV photons were used to deliver at least 95% of the prescription dose to at least 95% of the target volumes expanded isotropically by 5 mm to planning target volumes (PTVs). The resulting dose distribution is reported in Fig. 16‑4 .
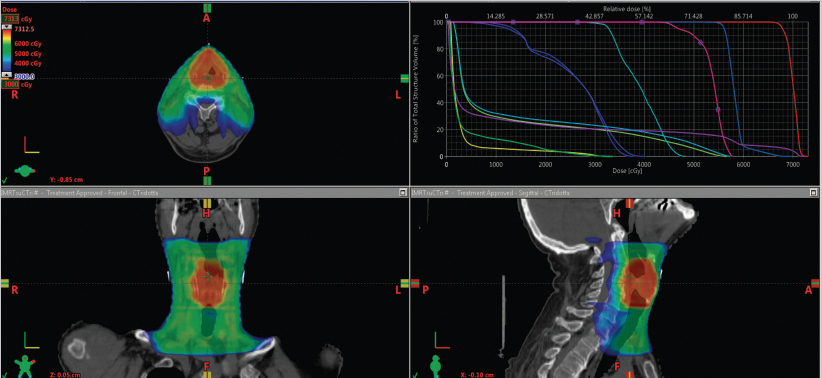
The dose to the following organs was constrained (goal): parotids (V30 < 50%); spinal cord + 2 mm (Dmax 0.1 mL: 44 Gy), brain (Dmax 1 mL: 60 Gy), brainstem (Dmax 0.1 mL: 54 Gy), brachial plexuses (Dmax 0.1 mL: 60 Gy), upper gastrointestinal (GI) mucosa (out-Dmax 1 mL: 30 Gy; in-V66.5 < 64 mL). The right upper panel of Fig. 16‑4 illustrates the achieved dove volume histograms for selected organs at risk.
The treatment was delivered with daily image guidance throughout cone-beam CTs. Concomitant chemotherapy consisted of cisplatin, 100 mg/m2 on days 1, 21, and 42.
The patient completed treatment as planned despite grade 3 (confluent) mucositis and grade 2 skin toxicity. The patient kept eating by mouth and parenteral/enteral feeding was not needed despite an about 8% weight loss from baseline.
A reevaluation physical examination is awaited 6 weeks after treatment end as well as a repeated MRI shortly there after.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree