10 Locally Intermediate Glottic Cancer: Transoral Laser Microsurgery
Abstract
Transoral laser microsurgery (TLM) is strongly recommended for early cancer of the glottis, since this technique is capable of achieving optimal outcomes in terms of recurrence-free survival and disease-specific survival provided by a minimally invasive approach with a low incidence of complications and very good functional results. The management of locally intermediate (T2–T3) glottic cancer is more challenging, because of a higher risk of recurrence, technical difficulty, and a wide range of other available treatment modalities such as TLM, open neck conservation surgery, and nonsurgical organ-preserving protocols. In this group of patients, the choice of treatment options is often guided by the technical facilities of the oncologic center. Some recommendations should be followed if TLM is the strategy chosen. We present the clinical case of a patient affected by a T3 glottic cancer treated by TLM in a highly specialized center as an example of the workflow that should guide the choice of such an approach.
10.1 Case Report
A 69-year-old male reported to our clinic with a history of progressive dysphonia for 4 months; he had never smoked and did not abuse alcohol. He had no chronic comorbidities and he had been treated 5 years earlier with radiotherapy for uveal melanoma of the left eye.
During outpatient consultation, transnasal videoendoscopic evaluation of the upper aerodigestive tract (UADT) was carried out using a flexible ENF-V2 videoendoscope connected to an EvisExera II CLV-180B light source (Visera Elite OTV-S190, Olympus Medical Systems Corporation, Tokyo, Japan), integrated with high-definition television and narrowband imaging (HDTV-NBI).
The examination revealed an exophytic lesion involving the entire true right vocal cord, which did not reach the arytenoid but extended to the anterior commissure, and toward the ipsilateral subglottis and supraglottis. The vocal cord was fixed, but arytenoid mobility was preserved. The lesion was characterized by atypical vascular changes suspicious for malignancy by HDTV-NBI examination ( Fig. 10‑1 a, b). 1 The feasibility of a transoral approach was assessed in the preoperative setting considering a Laryngoscore of 4. 2
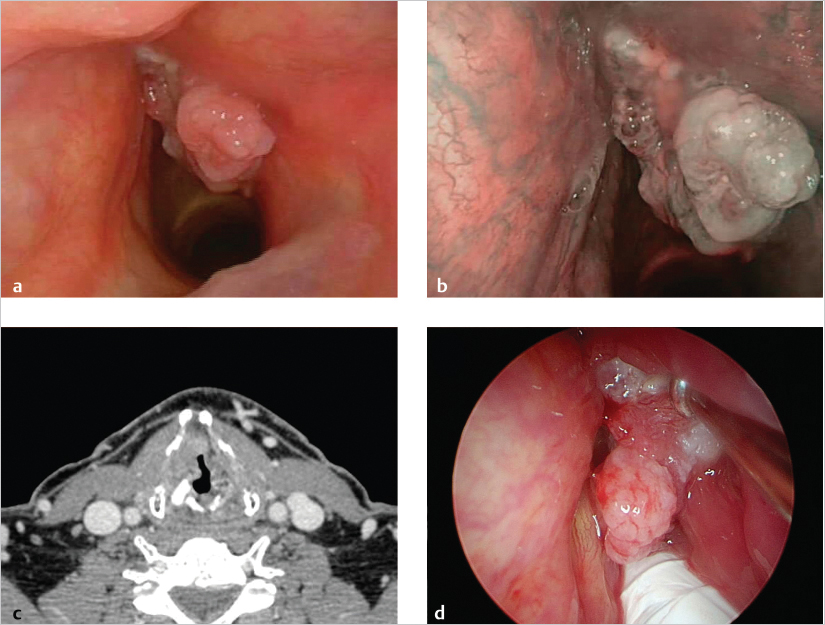
To evaluate deep extension of the tumor and its relationship with the paraglottic space (PGS), pre-epiglottic space (PES), and cartilaginous framework, CT was performed, which revealed deep invasion of the lesion toward both the anterior PGS and subglottis without erosion of the thyroid cartilage. No suspicious cervical lymph nodes were detected ( Fig. 10‑1 c). The clinical staging was a glottic tumor cT3N0M0 C2.
The patient was discussed by the multidisciplinary team and surgical treatment using transoral laser microsurgery (TLM) was proposed.
Laryngeal exposure, was obtained using a large bore laryngoscope (Microfrance Laryngoscopes 121, Medtronic ENT, Jacksonville, FL) which allowed visualization of the anterior commissure with external counterpressure on the neck. The diagnostic evaluation was integrated by intraoperative endoscopy with rigid endoscopes (0- and 70-degree angles). A superficial extension to the contralateral true vocal fold, ipsilateral supraglottis, and subglottis was confirmed ( Fig. 10‑1 d). A biopsy with frozen sections confirmed the diagnoses of squamous cell carcinoma (SCC).
TLM was performed by CO2 laser (Ultrapulse Laser CO2, Lumenis, Yokneam, Israel), set on ultrapulse mode, which 3-W delivered power at 400-mm working distance.
The resection started with, exposing and removing the false vocal cords overlying the cancer. An endoscopic extended cordectomy, type Va–Vd according to European Laryngological Society (ELS) classification, 3 was performed with a “multiblock technique” to excise the entire tumor in five blocks ( Fig. 10‑2 a, b). This technique allowed more precise and accurate assessment of the depth of the and comprehensive dissection of the PGS including the inner perichondrium of the thyroid cartilage. The resection was carried across the cricothyroid membrane as far as the first ring of the trachea. Care was taken not to penetrate the cricothyroid membrane or extend through the tracheal rings ( Fig. 10‑2 c).
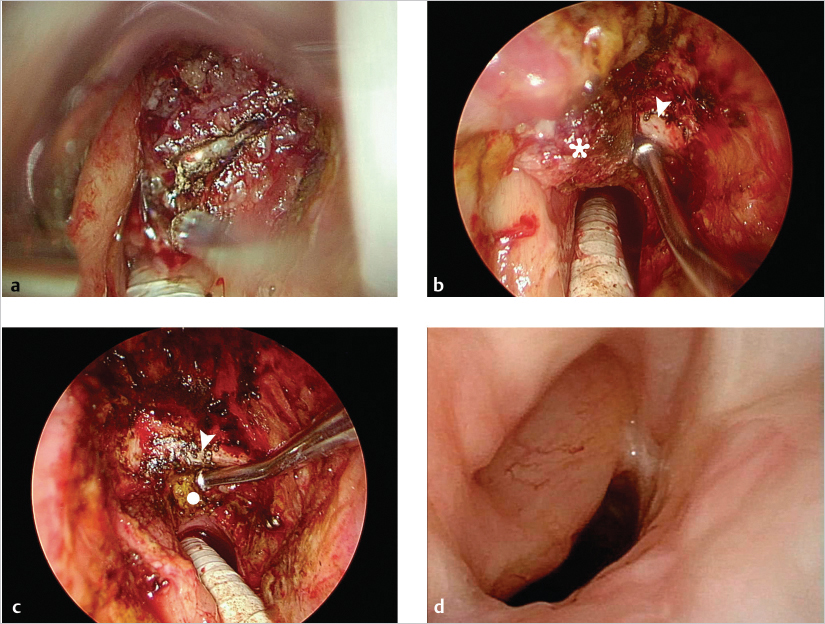
On the first postoperative day, videoendoscopy was performed to evaluate laryngeal mobility. No edema or bleeding was present and after a swallowing examination that confirmed absence of dysphagia or aspiration, the patient started oral feeding without any problems. He was discharged the second day after surgery without the need for tracheostomy.
The histopathological report confirmed a moderately differentiated (G2) SCC of the right vocal cord, extending to the anterior commissure and to the subglottis with invasion of the vocal is muscle and paraglottic space. No evidence of perineural or lymphovascular invasion was found and all superficial and deep margins were negative; the pathologic staging was pT3G2R0 C3 cN0M0 C2. The patient was scheduled for follow-up with imaging (CT and US of the neck) he 6 months and bimonthly endoscopic examinations for the first 2 years. The patient is currently free of 24 months after the surgery with good voice quality.
10.2 Discussion
Locally intermediate glottic cancer encompasses a heterogeneous variety of different lesions with distinct biological behavior and prognosis. Neoplastic pathways of diffusion toward visceral spaces (PGS and PES), invasion of the cartilaginous framework, and fixation of the vocal cord and/or the arytenoid represent critical issues that must be carefully considered during therapeutic planning. 4 , 5
Such cancers are treatable by a wide range of different therapeutic strategies including TLM, open partial horizontal laryngectomy (OPHL), total laryngectomy (TL), and nonsurgical organ-preserving protocols; the choice of treatment should be tailored, taking into account the highest cure rate with least morbidity, most favorable functional outcome, and costs.
In the last decades, increasing numbers of studies have confirmed that TLM has successfully expanded its indications, is reproducible in different oncologic centers, and is even suitable in combination with adjuvant therapy when necessary ( Table 10‑1). However, evidence-based data of its utility in intermediate-advanced tumors are limited to case series performed by expert surgeons from a few institutions. 6 , 7 , 8 , 9 , 10 , 11 , 12 Therefore, its degree of recommendation remains limited. Moreover, several “weak points” of TLM such as inadequate exposure of the larynx, anterior commissure involvement in the craniocaudal direction, infiltration of the PGS with arytenoid fixation, massive invasion of the PES, and erosion of the laryngeal framework are still under debate, thus restricting its application compared with more traditional surgical and nonsurgical options. 13
For intermediate glottic SCC, functional outcomes in terms of voice, swallowing, and preservation of normal airway patency are also critical issues in the decision-making process. These factors may, in fact, dramatically impact the patient’s emotional and physical life. The quality of the voice after TLM is related to the extent of resection and most authors have reported acceptable vocal outcomes, or at least comparable to those obtained after OPHL. 14 , 15
Moreover, in contrast to the OPHL, TLM can better customize the mucosal and deep extension of the resection according to the size and location of the cancer, thus minimizing the removal of uninvolved tissues resulting in preservation of healthy surrounding structures without modifying the physiologic laryngeal elevation. This is an essential aspect in adequate bolus progression, and thus greatly avoiding postoperative swallowing problems.
The negligible rate of aspiration following TLM represents an excellent result, especially when compared with the data reported after OPHL (temporary aspiration ranging from 32 to 89%) and chemoradiation (CRT; up to 84% of patients with temporary aspiration). 15 , 16 , 17 , 18 The same holds true for reduced perioperative and late morbidity, shorter hospitalization time, and fewer side effects. In particular, compared to OPHL and CRT, duration of hospitalization after TLM is significantly shorter (8.3 vs. 20–24 days, according to the specific protocol). Normal swallowing without permanent gastrostomy is achieved in 98% of cases and physiologic breathing without tracheostomy in 100% of patients. 16 , 19 , 20
Another key strength of TLM is its feasibility in fragile elderly patients (older than 70 years) for whom open partial laryngectomies and nonsurgical organ preservation strategies are contraindicated due to associated comorbidities or age limits. 10
A debated issue about management of laryngeal carcinomas is planning of follow-up. MR, in the hands of dedicated and experienced head and neck radiologists, has a higher diagnostic accuracy than CT in detecting recurrence of previously untreated intermediate glottic SCC and in all patients who underwent previous treatments. Therefore, this imaging technique should be always preferred, when available and feasible instead of CT. 21
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree