10 Cholangiocarcinoma: Ablation and Intra-arterial Therapies
10.1 Introduction
Cholangiocarcinoma is an aggressive neoplasm originating from the bile duct epithelium. Historically, cholangiocarcinomas have been described as rare tumors, but they represent the second most common primary hepatic tumor after hepatocellular carcinoma. A variety of conditions can predispose to the development of cholangiocarcinoma ( Table 10.1 ). The incidence of cholangiocarcinoma appears to be on the rise. 1 Prognosis and treatment options are variable depending on location and tumor biology but have historically been poor, with survival from time of diagnosis ranging from 3 to 11 months in the face of best available therapy. 2 , 3 , 4
Definite predisposing factors | Possible predisposing factors |
Primary sclerosing cholangitis | Hepatitis C |
Chronic liver fluke infection | Cirrhosis |
Toxins | |
Hepatolithiasis | Biliary-enteric anastomotic procedures |
Biliary malformations (choledochal cyst) |
Cholangiocarcinomas are classified by their location; this has important treatment and prognostic implications. They can occur anywhere along the bile tract, from small intrahepatic ductules to the ampulla. The hilar variant or Klatskin tumor is the most common, with extrahepatic and gallbladder variants. Up to 10% of tumors are solely intrahepatic. 5
The mainstay of therapy for cholangiocarcinoma of any type remains surgical resection, with cure rates ranging from 28 to 40%. Unfortunately, many patients are deemed unresectable at presentation, likely owing to the multifocal nature of cholangiocarcinoma and proximity to hilar structures. 6 Transplantation is another surgical option, with a recent series showing a 5-year survival of 38% in transplanted patients, which increased to 68% in those treated with neoadjuvant chemotherapy. These results are tempered by strict patient selection criteria and a limited supply of organs. 7 , 8
Optimal second-line therapy for cholangiocarcinoma has not been determined. Systemic chemotherapy, external beam radiation, localized photodynamic therapy, and brachytherapy have all been used, most with limited success and high levels of toxicity. Given the fact that no single nonsurgical therapy is particularly effective, the intrahepatic variant of cholangiocarcinoma represents an enticing potential target for liver-directed therapy. Furthermore, malignant tumors of the liver and the biliary ducts theoretically derive their blood supply preferentially from the hepatic arterial circulation, in contrast to normal hepatocytes, which are preferentially supplied by the portal vein. Liver-directed therapy is largely limited to treating the intrahepatic variant; however, extrahepatic cholangiocarcinoma metastatic to the liver also represents a potential target. 9
10.2 Indications
The main indications for percutaneous therapy of patients with intrahepatic cholangiocarcinoma fall into a few major categories: primarily unresectable (due to anatomy/location), poor performance status precluding surgery, recurrent disease after resection, or extrahepatic cholangiocarcinoma metastatic to the liver. Palliation of mass symptoms and refractory biliary obstruction are other potential indications for locoregional therapy. An emerging indication for percutaneous treatment is to downstage initially unresectable patients for possible resection or transplantation.
10.3 Contraindications
Absolute contraindications are a life-threatening anaphylaxis to contrast or any other medications used and an uncorrectable coagulopathy. Poor performance status is a strong relative contraindication, because most studies have excluded patients with an Eastern Cooperative Oncology Group (ECOG) score > 2 or a short life expectancy (< 6 months). Poor liver function reserve also represents a relative contraindication to therapy, given the potential of locoregional therapy to damage normal liver. Patients with extrahepatic metastatic disease are unlikely to benefit from treating only some of their metastatic burden. Prior biliary enteric anastomoses or an incompetent sphincter of Oddi are relative contraindications to percutaneous therapy given the high risk of infectious complications. Uncorrected anemia and leukopenia are contraindications to chemotherapy. Platelet levels should be reviewed to insure they are at levels adequate for hemostasis for both arterial and solid organ punctures.
10.4 Patient Consideration and Workup
As in any interventional oncology procedure, initial patient selection is crucial to success. The initial workup and treatment planning process are centered around a meticulous review of the patient’s medical history, oncological history, and diagnostic imaging. Oncological clinical decision making is complex and is best performed in a multidisciplinary setting combining surgical specialists, medical specialists, diagnostic radiologists, interventional radiologists, and radiation therapy specialists.
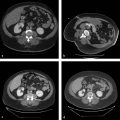
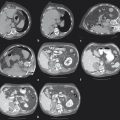
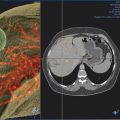
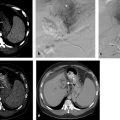
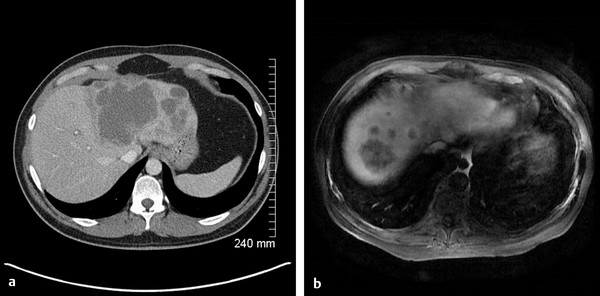
Surgical therapy has demonstrated superior survival benefit with respect to all other treatment modalities in the treatment of intrahepatic cholangiocarcinoma, and the initial concern is whether complete resection can be achieved (i.e., R0 resection). The scope of surgical decision making is beyond the scope of this text, but the imaging findings pertinent to surgical planning significantly overlap those used in locoregional therapy planning. Imaging is reviewed, with specific attention paid to the location of the tumor, proximity to/encasement of adjacent vascular structures, centricity/number of tumors, arterial supply, and possible percutaneous approaches ( Fig. 10.1 a, b). The relative conspicuity of the tumor on imaging modalities can be useful to determine the optimal method of image guidance for ablation. Determination of portal venous and biliary patency is important because these are associated with an increased risk of complication. Lastly, accurate determination of the stage is important given that extrahepatic metastatic disease is a relative contraindication to liver-directed therapy.
Laboratory and clinical data are also reviewed for relevant contraindications. ECOG score is a useful assessment of performance status. Patients appropriate for therapy typically have an ECOG score < 3 because patients with higher scores are less likely to derive benefit from therapy due to coexisting morbidity. Complete blood counts, chemistries, and liver function tests are routinely obtained to evaluate for possible procedural contraindications. Elevated bilirubin values in this population must be interpreted with caution as biliary obstruction may falsely give the impression of poor hepatocyte function. Lastly, baseline tumor markers (usually CA 19–9 and CA-125) are obtained and, if initially elevated in a patient with proven cholangiocarcinoma, they have some value for following the efficacy of therapy. Caution must be used because biliary system infection (sometimes subclinical) can spuriously elevate these values. A complete blood count is obtained to ensure adequate platelet numbers and cell counts prior to the patient receiving any chemotherapy.
10.5 Selection of Therapy
The clinical superiority of one percutaneous treatment modality over another has not been determined in any randomized, controlled clinical trial. Determining which treatment to pursue focuses largely on technical considerations, theoretical considerations, individual patient factors, and operator/institutional experience.
A comparison of patient factors favoring ablative or transarterial therapy is shown in Table 10.2 . Ablative therapy tends to favor smaller, oligocentric disease. The best results have been seen in tumors < 3 cm and intermediate results in tumors < 5 cm, and emerging literature suggests acceptable recurrence rates in tumors up to 7 cm. 10 Central tumors, diffuse/infiltrative morphology, and mutilfocality are more feasibly treated with transarterial therapy. Despite historical concerns over arterial chemoembolic therapy in the presence of portal vein thrombosis, recent data suggest that this is safe. 11 If downstaging to resectability/transplantation is a consideration, consultation with the surgical team may also provide insight into optimal therapy.
Transarterial therapy | Ablation |
Multicentric disease | Focal disease |
Infiltrative tumor type | Mass forming type |
Central location | Peripheral location |
Adjacent to diaphragm |
10.5.11 Technique
Considerable individual and institutional variation exists in the particular techniques used for both hepatic chemoembolization and percutaneous ablation. The techniques described hereafter are given as examples.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree