1 T1a Glottic Carcinoma Undergoing Transoral Laser Surgery
Abstract
In this chapter we discuss the case of a T1a squamous cell carcinoma of the glottis treated with transoral laser microsurgery with complete removal of the cancer that showed no signs of recurrence for 3 years of follow-up. The first symptom of cancer of the glottis is usually hoarseness, and early diagnosis is extremely important. Laryngoscopy is the most important examination for diagnosing and staging of the disease; however, in cases which may not be possible to identify all the limits of the lesion during laryngoscopy, an imaging examination (CT or MRI) must be performed, which may help evaluate the tumor extension. Treatment goals are cure of the cancer and preservation of laryngeal function, such as voice and swallowing. Some of the most suitable treatment options are transoral laser microsurgery, radiotherapy, and open partial laryngectomy. The transoral laser microsurgery approach has been associated with good oncological and functional results, low complication rates and less severe complications when compared to the other techniques, including cases involving the anterior commissure. This technique also results in lower management costs and reduced hospitalization time. Patient selection, laryngeal exposure, and type of cordectomy are major points of surgical success, and there is still much controversy about free margins as a predictor of recurrence. While using CO2 laser, potentially dangerous complications of the procedure must be avoided with appropriate protection of the endotracheal tube and the patient’s eyes and face while using a CO2 laser.
1.1 Case Report
A 58-year-old female physician, was admitted to our service complaining of progressive dysphonia that had developed in the past 3 months. She denied dyspnea, dysphagia, and dyspeptic symptoms. She admitted to cigarette smoking, (40 pack-years) and alcohol consumption socially. No comorbidities were identified and family history was negative for cancer.
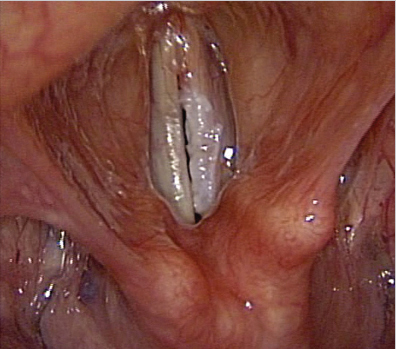
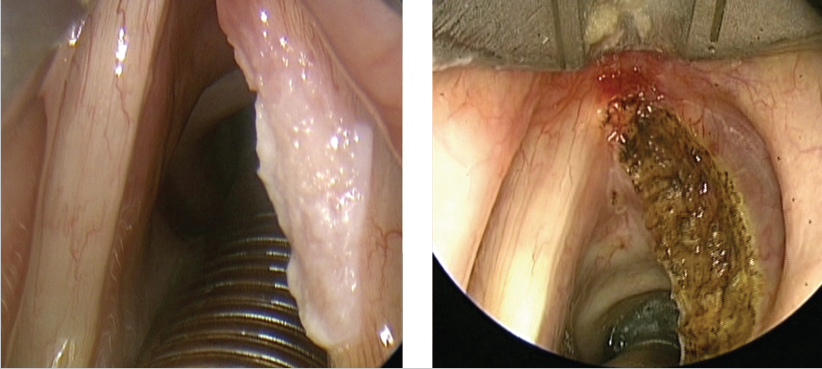
Her voice was moderately rough and the video-laryngoscopy revealed extensive leukoplakia affecting the entire anteroposterior extension of the right vocal fold, without involvement of the anterior commissure ( Fig. 1‑1 ). The neck was clinically negative.
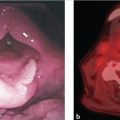
After treatment options were discussed with the patient a transoral laser microsurgery technique was performed, with complete excision of the lesion. Intraoperative frozen section biopsy revealed a high-grade intraepithelial lesion without evidence of infiltration of the basement membrane (carcinoma in situ). A type II cordectomy with complete removal of the tumor was performed ( Fig. 1‑2). Pathological examination revealed a superficially invasive, moderately differentiated squamous cell carcinoma (SCC) of the right vocal fold, with free margins.
This patient has been followed up regularly for 3 years, with no signs of recurrence. Laryngoscopy showed complete glottic closure. Voice quality was good and the patient was satisfied with it.
1.2 Discussion
Cancer of the larynx accounts for 2 to 4.5% of all malignant neoplasms and 25% of the head and neck tumors, with 50% of these cancers involving the vocal folds. In males, the incidence is highest in Southern Europe, some countries of Central and Eastern Europe and of South America, and in the African-American population of the United States. In these populations, standardized incidence was 10/100.000. In females, the highest rate is found in the African American population, at around 3/100.000. 1
Early cancer of the glottis refers to a cancer that has not spread to adjacent spaces of the larynx and corresponds to the stages Tis, T1, and T2 (AJCC/UICC TNM, 8th edition). 2 The first symptom of cancer of glottis is usually hoarseness and the early diagnosis is quite relevant, since advanced lesions require more aggressive treatment modalities. The use of imaging examinations, such as computed tomography (CT) and magnetic resonance imaging (MRI), may help evaluate the extent of the neoplasm, particularly in cases in which all limits cannot be determined with direct laryngoscopy. However, laryngoscopy is the most important examination for diagnosing and staging of early cancer of the glottis.
Treatment goals are cure of the cancer and preservation of laryngeal function such, as voice and swallowing, and minimizing the risk of serious complications. Different types of procedures can be used, such as transoral laser microsurgery (TLM), radiotherapy (RT), or open partial laryngectomy (OPL). Since the survival rates are almost equivalent, treatment choice is usually decided based on voice outcomes, treatment duration, and the patients’ condition and preference. 3 , 4
Recent studies about cost-effectiveness compared the main treatment modalities of early glottic cancer and revealed best results with TLM because of its low management costs, reduced hospitalization time, and good oncological and functional results, with low complication rates and less severe complications when compared to the other techniques. 5 , 6 The OPL is associated with longer hospitalization time, higher rate of complications (postoperative pain, edema, emphysema, and the required tracheotomy), high costs, and worse functional results, although it allows obtaining larger free margins and the possibility of treating the neck when required. 7 On the other hand, RT offers good oncological and voice outcomes, but higher costs, prolonged time of treatment, mucosal damage, and long-term side effects such as xerostomia. 8
Although there is no current consensus, recent meta-analysis showed no significant difference in voice quality comparing laser cordectomy and RT in the treatment of T1 glottic carcinoma. 9 Longitudinal voice evaluation of patients treated with CO2 laser cordectomy revealed immediate worsening of voice quality (< 3 months), followed by recovery and stabilization (> 6 months), and results comparable to preoperative patterns, especially in cases related to less extensive cordectomy, unilateral and without anterior commissure involvement. 10 , 11 , 12
Despite the good oncologic and functional results of TLM in early cancer of the glottis, there has been ongoing debate regarding its application in patients with involvement of the anterior commissure. Although primary RT has been considered as an effective and voice-preserving treatment modality for cancer of the glottis, it has demonstrated worse results in cases involving the anterior commissure, but there is still no consensus regarding this matter. Some authors have advocated OPL due to the achievement of better local control (86–91%) compared to those treated with RT (56–76%). 13 , 14 However, considering the duration and possible complications of RT and open surgery, TLM may be the preferred treatment modality with shorter hospitalization, minimal morbidity, and comparable local control (79–92.8%). 15 , 16
Surgical margins are also a major concern. Some authors have considered positive margins as a factor of bad prognosis. 16 , 17 However, others did not demonstrate the association of the margin status and patient’s outcomes. 15 , 18 A resection margin of 2 mm is often considered as sufficient in cancer of the glottis, as opposed to other sites in the head and neck. 19 With resection artifacts and specimen shrinkage and carbonization around this tiny margin, pathological assessment could be hampered leading to false interpretation of tumor edges. Therefore, results of positive margins do not necessarily represent inadequate tumor removal. 17 Furthermore, the recent introduction of new endoscopic devices, namely, the use of narrow band imaging (NBI) has demonstrated enormous value in defining superficial extension of the cancer and delineating its margins of resection. This “biologic endoscopy” concept revealed a great reduction of superficial positive margins from 23.7 to 3.6%. 20
Even though frozen section is reliable in laser-assisted cordectomies, 21 this procedure seems difficult to implement in a regular basis given that it is time-consuming and requires an available and experienced pathology team. On the other hand, biopsy of the tissue remaining in and around the tumor removal ground has been recommended. 17
Besides, in an attempt to improve local control, some authors also suggest a routine second-look laryngoscopy to detect residual glottic cancers. However, while the identification of residual tumor may be beneficial for oncologic control, the routine practice second-look laryngoscopy is of questionable value due to the low rate of findings and high cost. 21 , 22
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree