My ambition is to have this wonderful gift produce practical results for the future of commercial flying and for the women who may want to fly tomorrow’s planes.
—Amelia Earhart
This chapter is primarily concerned with the current state of women’s health as related to aerospace medicine. Although much has been conjectured and written about the training and working of women in the aerospace environment, this chapter addresses the evidence provided in the current state of the literature. Women have made and are making significant contributions across the aerospace spectrum from commercial to military to space flight. As women meet these challenges, the flight surgeon must be aware of issues unique and pertinent to women’s overall health and well-being. Except for possibly the latter stages of pregnancy, women have no restrictions or significant limitations in flight performance. The health care professional can be confident about addressing particular women’s health issues as noted in this chapter in standard manner resulting in sustained high performance by women in all aspects of flight or for women participating only as passengers.
Women’s involvement in aviation begins with its earliest days that continues currently both in air and space travel. Currently in the United States, women comprise 6% of all Federal Aviation Administration (
FAA) pilots with number totaling 36,584 (
1). Within the United States military, women make up roughly 6% of all fixed and rotary wing pilots (
1). Thirty-two percent of National Aeronautics and Space Administration (
NASA) employees are women with approximately 18% serving in scientific or engineering roles. Of the 91 current active astronauts, 18% or 20% are women and of the 15 international astronauts, 2 are women (
2). Reviewing
FAA data, the number of women in all classes decreased over the last 25 years but this is offset by the remarkable 13-fold increase in the first (air transport pilot) and second class (commercial) female pilot population. Women are represented in all aviation support roles from mechanic to flight engineer, but only constitute a majority in the flight attendant category at 80% (
1).
Contributions or firsts for women occurred in every decade since the start of powered flight in 1903 by the Wright brothers and continues through today. The following is a brief overview of the few notable contributions and achievements by women in the aerospace field.
1910—Raymond De Laroche of France is the first woman in the world to receive a pilot license.
1911—Harriet Quimby is the first American woman to earn a pilot certification and fly across the English Channel.
1921—Bessie Coleman is the first African American, man or woman, to receive a pilot license.
1932—Amelia Earhart of the United States is the first woman to cross the Atlantic Ocean solo in an aircraft.
1934—Helen Richey, an American, is the first woman hired as a pilot for a United States Commercial Airline.
1942—Mary Van Segue of the United States is certified as the first female Air Traffic Controller.
1942—The United States Women’s Air Force Service Pilots (WASPs) led by Jackie Cochran are the first American women to pilot U.S. military aircraft.
1953—Jacqueline Cochran is the first woman to break the sound barrier done in a Boeing North American F86 Sabre jet.
1963—Valentina Tereshkova of the United Soviet Socialist Republic is a cosmonaut and the first woman in space aboard the Vostok 6.
1973—Emily Warne, an American, is hired as the first female air transport pilot for a modern, jet-equipped scheduled airline, Frontier Airlines.
1974—Barbara Raines becomes the first woman pilot for the U.S. military.
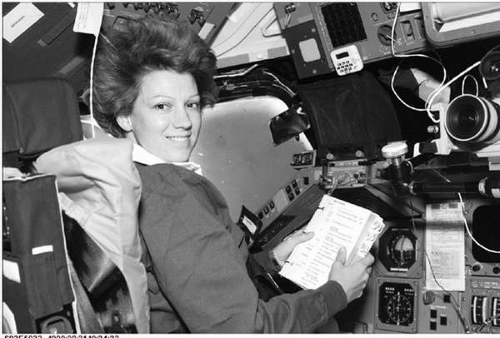
1983—Sally Ride is the first American woman in space as part of the
STS 7 shuttle mission (
Figure 22-1).
1986—Jenna Yeager copilots the Voyager credited with the first around the world, nonstop, nonrefueled flight.
1993—U.S. Department of Defense, through Secretary of Defense, Les Aspin, opens combat aviation to women.
1999—Lt. Col. Eileen Collins of the United States Air Force (
USAF) is the first woman to serve as a space shuttle commander. She previously piloted two Space Transportation System (
STS) missions (
Figure 22-2).
2007—Astronaut Sunita Williams aboard the International Space Station set a record for the number of space walks and total time in space walks for a woman at four walks totaling 29 hours 17 minutes.