Withholding and Withdrawing Potentially Life-Sustaining Treatment
Richard J. Ackermann
“I will define what I conceive medicine to be: In general terms, it is to do away with the suffering of the sick, to lessen the violence of their disease, and to refuse to treat those who are overmastered by their disease, realizing that in such cases medicine is powerless.”
–Hippocrates of Cos, 460-380 B.C.
More than 500,000 patients die of cancer in the United States every year. A couple of generations ago, these patients died rather speedily, from cardiopulmonary failure, sepsis, or other causes. Now, a substantial number of patients with cancer find themselves dying over a prolonged period in highly technologic and sometimes impersonal environments, such as the intensive care unit. By the time patients are dying in the intensive care unit, fewer than 10% can participate in the decision-making process, except through advance directives or surrogates. More and more, we are faced with decisions to forego cardiopulmonary resuscitation (CPR) or other forms of life-sustaining treatments. At least 65% of patients with cancer prefer to die at home, but only 30% are successful in doing so (1, 2, 3).
Helping patients and families make decisions about potential life-sustaining treatments is an essential skill for cancer specialists. The oncologist needs to understand the legal and ethical issues, as well as practical issues of implementation. All 50 states have laws and regulations on informed consent and the withdrawal of life-sustaining treatments. In hospitals and other institutions, the general policy is that physicians should provide all available treatment, unless there are specific decisions to the contrary (4). Over 70% of deaths in US intensive care units now occur as a withdrawal of life-sustaining treatments. The General Medical Council of the United Kingdom has produced a practice guideline on the subject (5).
There are at least three reasons why a physician might agree to withhold or withdraw a potentially life-sustaining treatment. First and by far the most important, we do so to comply with the wish of an autonomous patient or their surrogate, assuming that fully informed consent has been obtained. Second, we do so because the therapy cannot meet the overall treatment goal, even if it would have some short-term physiologic effect. And third, we do so because the therapy has failed and is prolonging the dying process (6).
The central issue for patients suffering from advanced malignancy is not when to switch from curative to comfort measures. Appropriate palliation of symptoms is always a goal, from the first diagnosis of cancer through terminal care. Rather, the primary issue is whether continued aggressive care has a realistic chance of working, or whether it is more appropriate to concentrate on comfort, letting the disease take its natural course, and allowing the patient to die (6). Withdrawal of life support should occur when the burdens of treatment outweigh the benefits, as determined by the overall goals of the patient. This is vague but reflects clinical reality. Table 63.1 addresses common concerns oncologists have regarding withholding and withdrawing potentially life-sustaining treatments.
The overall legal and ethical consensus behind withholding and withdrawal is based on patient autonomy. Every competent adult has the right to decide which medical interventions she wants, including the right to refuse treatment, even if that would lead to death. If the patient lacks decision-making capacity, then in all 50 states there is arrangement for a surrogate to be named, who has full legal authority to act. All medical interventions are included, including the decision to use or not use artificial nutrition and hydration (ANH). Patients who die as a result of withdrawal of life-sustaining treatments die of their underlying disease process, not from assisted suicide or euthanasia (8).
There is no moral or legal distinction between withholding and withdrawing a treatment. However, from an emotional and clinical perspective, it is nearly always easier not to begin a treatment rather than to stop it (9).
It is not useful to make a distinction between “ordinary” and “extraordinary” treatments, because these terms can only be defined by each individual. A much better method is to look at the benefits and burdens of the proposed intervention. The “ordinary” treatment of intravenous hydration in a healthy patient with pneumonia may be considered burdensome by another patient who is suffering from end-stage malignancy. Further, the “extraordinary” treatment of hemodialysis and vasopressors can certainly be justified in patients with cancer who experience a complication of cancer or its treatment. Ask this question: what are the benefits and the burdens of the intervention in this particular patient? (1).
Physicians can ensure appropriate care in the hospital, outpatient clinics, and across care settings, even if patients desire not to use certain medical interventions. Unfortunately, studies have documented that too many patients die without attention to these issues. For example, the Study to Understand Prognoses and Preferences for Outcomes and Risks of Treatment (SUPPORT) documented that despite advance directives, many patients underwent invasive medical treatments against previously stated wishes (10).
Table 63.1 Typical Legal and Ethical Concerns Cancer Specialists May Have Regarding the Withholding or Withdrawing of Potentially Life-Sustaining Treatments | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
In the SUPPORT, 316 patients with colon cancer metastatic to liver and 747 patients with stage IV non–small cell lung cancer who died within one year of an index hospitalization were studied. During the last 3–6 months of life, more than 50% of both groups preferred treatment that focused on comfort care, even if this shortened their lives. Despite this preference, >25% were in severe pain in the last 3–6 months and >40% were in severe pain the last three days of life (11).
In some circumstances, oncologists have a long-term relationship with patients in community settings, which may facilitate communication at the end of life. In these settings, end-of-life discussions may occur in small pieces over several months or years. In other circumstances, the cancer specialist may be serving as a consultant and may not have the luxury of a long-term relationship. Consultation with palliative care specialists may improve end-of-life care and reduce use of nonbeneficial resources (12).
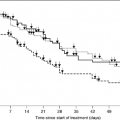
Patients with cancer may consider many life-sustaining treatments, either related to cancer (chemotherapy, radiation, surgery) or not, such as CPR. There are many other choices patients can make, including elective intubation, mechanical ventilation, dialysis, blood transfusion, artificial nutrition and hydration, diagnostic tests, antibiotics, other medications and treatments, as well as admissions to the hospital or to an intensive care unit. The patient’s treatment choices and complexities often increase as the patient becomes overmastered by aggressive malignancy. Many patients who initially want to cure the cancer will have no care restrictions at the beginning of the physician–patient relationship. Patients in whom cancer does not respond to treatment may opt for a do-not-resuscitate status, with progressively more restrictions as the disease progresses. As patients approach the end of life, physicians tend to withdraw life-sustaining treatments in a logical sequence, starting with restricting blood products and progressing through restrictions on dialysis, vasopressors, mechanical ventilation, parenteral nutrition, antibiotics, intravenous fluids, and enteral tube feeding (13).
One reason that physicians (and also patients) may not consider palliative approaches until too late is uncritical acceptance of new technology. Physicians may by seduced by authority—you do something because someone you really respect advocates the procedure, although there is little evidence of its merit. Not only do we accept new technology uncritically, but we also become almost reverent about it. Part of this is that procedures and technology are usually reimbursed well. We also tend to accept unproved dogmas of decades or centuries; some of these turn out to be useless or even harmful. Finally, we sometimes practice medicine based on our last wonderful success or disaster, or ones we have heard about—anecdotal medicine—rather than practicing evidence-based medicine (14).
Generally, medicines such as chemotherapy must have rigorous proof of both efficacy and safety before they are approved for clinical use. However, tests and procedures have no FDA approval. Demand rigorous proof of technologies before incorporating them into practice. Just because a new cancer operation has been invented does not mean it should replace the standard—well-crafted randomized clinical trials should compare the new operation with the old (14).
Oncologists should not only provide general guidelines but also feel free to provide specific advice to patients with cancer and families who are struggling with these difficult decisions. The thoughtful clinician can provide frank advice based on science but also on personal experience. For example, it might be appropriate in one setting to say:
“You have advanced lung cancer. We can’t change that awful fact, but there is much we can still control. Inserting a feeding tube into your stomach may increase the number of days you would live, but the cost may be that the quality of your remaining days would be worse.”
The Education for Physicians on End-of-life Care curriculum, supported by the AMA, suggests a workable 8-step process when deciding whether to withhold or withdraw therapy (Table 63.2). Ideally, these steps occur during routine
office follow-ups, although in many cases, they won’t happen until a crisis such as febrile neutropenia or a mechanical complication of advanced malignancy has occurred (7).
office follow-ups, although in many cases, they won’t happen until a crisis such as febrile neutropenia or a mechanical complication of advanced malignancy has occurred (7).
Table 63.2 Eight-Step Protocol to Discuss Withholding or Withdrawing Therapy | ||
|---|---|---|
|
Patients have different preferences, or styles, in medical decision making. For example, some want all the possible information and then make the decision themselves, while others may want the physician to decide. In a study of 999 women with breast cancer, 18% of women preferred a paternalistic model where the physician makes decisions, 15% wanted the physician to make the decision after hearing her input, 44% wanted a joint physician–patient decision, 14% wanted to make the decision herself after getting the physician’s input, and 9% wanted to make all decisions herself (15).
Physicians should find out what the patient or family knows about the current medical situation. There are often tragic misconceptions or misunderstandings, and patients often seek to blame something in their past or medical treatment for their current predicament. Avoid medical jargon, and judge just how much detail is helpful. Some patients want to know everything, while others simply want an overview such as “your kidney function is stable.” Provide an honest opinion, express doubt if you have it or if physician consultants disagree. Ask if the patient or family want more information or a second (or third) opinion.
The key to the discussion is determining the general goals of care. For example, the physician may summarize like this:
“Let me tell you what I hear you saying.”
If the patient no longer has decision-making capacity, ask the appointed decision maker to articulate the patient’s values and goals of care. Encourage the family to use substituted judgment, where they transmit what they believe their loved one would say, rather than what will reduce their guilt. If family disagreements occur, spend more time on the overall goals of care before proceeding to specific treatment options.
Some patients may ask you to “do everything.” This “everything” is very broad and easily misinterpreted. It implies that the choice is between everything and nothing, which is almost never true. Further, it assumes that the physician has power over the disease, which is also not true. For example, never ask a family:
“Do you want us to do everything?”
Because the obvious answer is:
“Yes, of course we want everything for our mother, whom we love dearly.”
If the patient is terminally ill, establish context by a statement such as:
“Your father is dying from the lung cancer, despite everything we have done to try and treat it. His death will probably occur in the next few days or weeks.”
After establishing the overall goal of care and a context for decision making, talk about specific treatment options. Provide this information in small pieces. For example, if this is the visit when you tell the patient she has cancer, it is likely that nothing else you say at the visit will be heard. Simply say:
“I have some really bad news. The biopsy came back positive for cancer of the pancreas,”
and wait, sitting silently. Stop to assess for reactions and clarify misunderstandings. Most importantly, allow time for emotion. Patients and their families may be profoundly disturbed, especially at key times such as diagnosis, first metastasis, complications, or failure of standard therapies. You made need other colleagues, such as counselors, to assist. Patients are nearly always grateful for the advice and continued presence of the physician, even if the advice is withdrawing an ineffective treatment (7).
Patients deserve a full and clear understanding of proposed therapies. With advanced cancer, especially when the prognosis is doubtful, always include a discussion of palliative options, even if initial curative/remittive therapy has not yet been offered. Patients may wish comfort-based care to take center stage at some point.
Finally, try to establish a plan. If the patient or her decision maker simply can’t do this, then agree to meet again or perhaps convene a family meeting. Ask if a chaplain, social worker, or out-of-town family member should be consulted (7).
Hope for the best, and prepare for the worst
Patients and oncologists often feel they must choose between fighting the disease and preparing for death. The physician may be reluctant to discuss palliative care or withdrawal of ongoing treatment, because the patient will “lose hope.” But hoping for cure and preparing for eventual death need not be exclusive. A recent editorial calls this tension “Hope for the best, and prepare for the worst” (16). These authors give concrete advice on how to talk about chemotherapy and palliative care. Conversations such as these should occur early and often, not just when facing the final weeks of life.
Give time to both hoping and preparing.
Doctor: “I will do everything I can to put your cancer into remission. We are hoping for the best. Still, I think we should prepare for the worst in case the treatment does not work.”
Align the hopes of the patient and physician.
Doctor: “Tell me more about your hopes for your treatment.”
Encourage, but do not impose, the dual agenda of hoping and preparing.
Patient: “When you talk about preparing for the worst, it feels like you’re ready to give up on me.”
Doctor: “The way I think about it, preparing for the worst helps me give you the best medical care, no matter what happens. I want to be your doctor and take care of you. I’m not giving up on you.”
Support this dual agenda of hope and preparation over time, as you develop a trusting relationship with the patient and family.
Patient: “I don’t want to think about preparing for the worst.”
Doctor: “It sounds like this is hard for you to consider. Can you describe what makes it hard to consider?”
Patient: “What if my wife can’t handle the worst?”
Respect hopes and fears, and respond to emotions.
Doctor: “I can see that caring for your family is very important to you. I have some ideas that may help in case the treatment doesn’t go the way you and I want it to” (16).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree