The costs of breast cancer care are substantial and growing, and they extend across the spectrum of care. Medical therapies and hospitalizations account for a significant proportion of these costs. Cost-effectiveness analysis (CEA) is the preferred method for assessing the health benefits of medical interventions relative to their costs. Although many CEAs have been conducted for a wide range of breast cancer treatments, these analyses are not used routinely to guide coverage or utilization decisions in the United States. Currently, patients and providers may not consider costs when making most treatment decisions; this is likely to change as payment reform spreads.
Key points
- •
Breast cancer care is costly, and future projections suggest that costs are likely to increase substantially over time.
- •
Medications and hospitalizations account for a significant proportion of breast cancer costs. Payers are beginning to introduce policies to constrain the growth of costs.
- •
Some breast cancer treatments may provide better value than others. Cost-effectiveness analysis is the preferred method for assessing the health benefits of medical interventions relative to their costs.
- •
The pressure for providers and patients to consider costs when making treatment decisions is likely to increase.
Introduction
Breast cancer is the most commonly diagnosed nondermatologic cancer and the second leading cause of cancer death for women in the United States and, thus, is responsible for substantial morbidity and mortality. Advances in screening and treatment have led to significant improvements in outcomes but have required more and more costly interventions. For these reasons, it should come as no surprise that breast cancer now accounts for the greatest share of cancer-related spending in the United States. Although the costs of breast cancer care are substantial and increasing, resources are limited and decisions about which services should and should not be covered are inevitable. In fact, these decisions are already being made; but many people question how these decisions are made and who is making them. In this article, the authors review the magnitude of spending on breast cancer, describe how costs are changing over time, and highlight which treatments and phases of illness have the greatest impact on spending. The authors outline the current efforts to control spending and discuss the role of cost-effectiveness analysis (CEA) as a tool to characterize the value of therapies, facilitate decision making, and set priorities. The authors also explore the roles and responsibilities of providers to determine what breast cancer care is worth.
Introduction
Breast cancer is the most commonly diagnosed nondermatologic cancer and the second leading cause of cancer death for women in the United States and, thus, is responsible for substantial morbidity and mortality. Advances in screening and treatment have led to significant improvements in outcomes but have required more and more costly interventions. For these reasons, it should come as no surprise that breast cancer now accounts for the greatest share of cancer-related spending in the United States. Although the costs of breast cancer care are substantial and increasing, resources are limited and decisions about which services should and should not be covered are inevitable. In fact, these decisions are already being made; but many people question how these decisions are made and who is making them. In this article, the authors review the magnitude of spending on breast cancer, describe how costs are changing over time, and highlight which treatments and phases of illness have the greatest impact on spending. The authors outline the current efforts to control spending and discuss the role of cost-effectiveness analysis (CEA) as a tool to characterize the value of therapies, facilitate decision making, and set priorities. The authors also explore the roles and responsibilities of providers to determine what breast cancer care is worth.
How much we spend and how we spend it
Annual spending on all cancer care in the United States exceeds $125 billion, and forecasts predict that spending will continue to climb in the years to come. Breast cancer is responsible for the largest share of cancer-related spending, an estimated $16.5 billion or 13% of all cancer-related spending in 2010. Past data demonstrate that the rate of growth in spending for breast cancer has exceeded that observed for lung, colorectal, or prostate cancer. Future projections suggest that breast cancer spending will exceed $20 billion in 2020.
Spending on breast cancer is distributed across the continuum of care, with approximately 23% going to evaluation and management in the year after diagnosis, 41% covering continuing care, and 36% being spent during the last year of life. It is not surprising that continuing care accounts for the largest share of lifetime costs, considering the relatively long survival of patients with breast cancer. The only cancer with a larger proportion of spending going to continuing care is prostate cancer. When compared with other cancers, the total spending for the initial phase of breast cancer care ranks fourth, and it ranks first for the continuing and end-of-life phases of care.
Several investigators have described the per-person costs of breast cancer care. A detailed review by Campbell and Ramsey, which included studies conducted through 2006, found estimates of lifetime direct medical costs ranged from $20,000 to $100,000. Although total costs were greatest during the continuing phase of care, the cost per unit of time was greatest during the initial and terminal phases of care. More contemporary estimates have placed the average annualized net costs for breast cancer care among women younger than 65 years at $27,700 per year during the initial phase, $2200 per year during the continuing phase, and $94,300 per year during the last year of life. For patients aged 65 years and older, costs are lower, especially during the last year of life ($62,900 per year).
An analysis of Medicare data demonstrated that the distribution of costs in the year after diagnosis by type of therapy was 25% for breast cancer surgery, 15% for chemotherapy, 11% for radiation therapy, 18% for other hospitalizations, and 31% for other services. The total costs attributable to breast-conserving therapy and radiation therapy are approximately $15,000 to $26,000, to mastectomy $10,000 to $13,000, and to mastectomy with reconstruction $23,000. Newer radiation techniques, such as hyperfractionation and partial-breast irradiation, may be less costly than traditional whole-breast radiation therapy. Intensity-modulated radiation therapy, a particularly expensive form of radiation therapy, is not part of routine care for breast cancer.
The 15% of breast cancer costs that have been attributed to chemotherapy for Medicare patients older than 65 years likely represents an underestimate because chemotherapy utilization in women younger than 65 years is significantly higher. When younger patients are included, chemotherapy for curative intent consistently represents one of the most substantial breast cancer costs, ranging from $23,000 to $31,000 per patient. Unfortunately, these studies did not include newer, costly chemotherapy agents, so it is hard to know the extent to which these estimates can be generalized to patients receiving care today. One year of trastuzumab, for example, adds approximately $50,000 to $65,000 to the cost of therapy. Chemotherapy can also lead to secondary costs from serious adverse effects, such as febrile neutropenia, which amount to between $1000 and $5000 per patient.
Patients with breast cancer experience significant and burdensome direct and indirect medical costs. For example, out-of-pocket medical costs for patients with breast cancer and their caregivers were estimated at approximately $2700 to $7900, respectively. Out-of-pocket costs may be lower in other countries (eg, $1000 in Canada). Although most patients who work before they are diagnosed with breast cancer continue to work after completing therapy, many lose time at work during or after their treatment. Lost wages from time spent on treatment and disability have been estimated at $4300 and $5900, respectively. At a national level, total lost-productivity costs from breast cancer deaths were estimated to be $10.9 billion in 2010; they accounted for 8% of all cancer-related productivity losses, exceeded only by lung and colorectal cancer.
What we get for what we spend
Although the United States spends substantially more on health care ($8000 per capita or 16.2% of the gross domestic product [GDP]) than any other country (<$5500 per capita or <12% of GDP), its outcomes are not necessarily better and are sometimes worse. For example, an international analysis found years of life lost caused by malignant neoplasm was 895 per 100,000 people in the United States, whereas it was 847 in Canada, 800 in Australia, and 725 in Japan. Interestingly, breast cancer 5-year relative survival rates are higher for the United States (90.5%) than for many other developed countries (eg, 87.1% in Canada, 86.1% in Sweden, or 85.2% in the Netherlands).
Studies have demonstrated clear improvements in the outcomes experienced by patients with breast cancer in the United States over the last 2 decades. In 1990, the age-adjusted mortality rate from invasive breast cancer was 33 per 100,000, whereas in 2009 it had fallen to 22 per 100,000. Since 1990, the annual death rate from breast cancer declined by more than 1.8% per year. Simulation studies suggest that half of this improvement is attributable to screening mammography and half is caused by the use of adjuvant systemic therapy (ie, chemotherapy and hormone therapy).
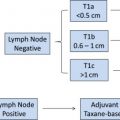
Improvements in survival that have been attributed to adjuvant systemic therapy are the result of 2 parallel trends. First, there have been significant advances in the efficacy of adjuvant therapies. For example, studies have demonstrated improved outcomes for patients treated with taxanes, dose-dense therapy, trastuzumab, and aromatase inhibitors. Second, the rate of utilization of adjuvant therapies has increased over time. Despite these gains and widespread efforts to disseminate treatment recommendations via clinical practice guidelines, many patients with breast cancer still do not receive proven, recommended therapies. The National Cancer Policy Board concluded that “for many Americans with cancer, there is a wide gulf between what could be construed as the ideal and the reality of their experience with cancer care.”
There are different theories regarding how quality-improvement efforts could impact costs. Improving quality could reduce spending by cutting hospitalizations, limiting complications, or other mechanisms. Alternatively, improving quality could increase spending by encouraging the use of recommended services that were not previously being delivered. A recent systematic review of 61 studies of general medical care found that the association between quality and cost was inconsistent. Few studies have evaluated this relationship for patients with cancer. A Surveillance, Epidemiology, and End Results/Medicare–based analysis of chemotherapy for colorectal cancer care found that high-spending regions were more likely to use chemotherapy, regardless of whether it was recommended (stage III), discretionary (stage II), or not recommended (stage I). In an analysis of women with newly diagnosed breast cancer, the authors found that providing recommended therapy was associated with higher cost, whereas avoiding unnecessary therapy was associated with lower cost.
Many of the aforementioned cost estimates focused on treatments provided to patients with local-regional disease. An analysis of women with metastatic disease who were older than 65 years found average spending in the 6 months after diagnosis was approximately $28,000, and the magnitude of spending in the 6 months that preceded death was similar. Although there was significant regional variation in spending, there was not significant regional variation in survival. In the last month of life, the percent of patients who used specific services included the following: more than 1 emergency department visit (40%), more than 1 hospitalization (27%), intensive care unit admission (19%), chemotherapy in the last 14 days of life (17%), and hospice (60%). Inpatient hospitalizations accounted for most of the expenditures and accounted for much of the observed regional variation in spending.
Controlling the costs of cancer care
Medical therapies are one of the major drivers for the growth of the cost of breast cancer care. Many medications are available to treat breast cancer. A compendium compiled by the National Comprehensive Cancer Network lists 36 medications, including 16 cytotoxic agents, 11 hormonal agents, and 9 biologics/antibodies. Five of these agents were approved for breast cancer in the last 3 years (eribulin, denosumab, everolimus, pertuzumab, and ado-trastuzumab emtansine), and many more agents are the focus of ongoing clinical trials (the Web site clinicaltrials.gov listed >1200 open interventional studies for breast cancer as of April 2013).
A review of spending on cancer drugs by Peter Bach describes how monthly median drug costs are greater for recently approved cancer medications compared with those approved in the more distant past. A group of hematology/oncology specialists reported that 11 of 12 cancer drugs approved by the US Food and Drug Administration in 2012 were priced at more than $100,000 per year. Moreover, the monthly costs of some existing cancer drugs have also increased. These changes, together with an increase in the rate of use of these agents, have contributed significantly to the substantial growth in cancer spending outlined earlier. There are several potential explanations for increases in per-unit drug costs: (1) drug development costs have increased; (2) newer drugs are more targeted than older drugs, so they cannot be used in as many patients; (3) drug approval decisions in the United States are not based on cost; (4) laws and regulatory policies limit payers’ ability to negotiate lower drug prices; and (5) there is a general willingness to pay for newer therapies, sometimes without much consideration of the magnitude of clinical benefit they confer.
Several reviewers have outlined the relatively modest incremental benefits associated with new cancer therapies, and some have asserted that costs may be increasing faster than health benefits. In some cases, providers have elected to forgo the use of payer-approved therapies because they offer marginal benefits and confer substantial costs (eg, a prominent cancer network decided not to use ziv-aflibercept after it was approved in 2012 ). Newer therapies may tend to confer smaller marginal benefits than their predecessors because, as outcomes improve, it becomes harder for newer treatments to yield the same magnitude of benefits conferred by older treatments. Also, newer treatments tend to be more targeted, so their impact on population health is potentially smaller; a nonspecific agent, such as paclitaxel, can be used to treat more patients than a targeted agent, such as pertuzumab.
High drug costs are undesirable because they limit access to potentially beneficial drugs for those with limited means, they preclude spending on other goods and services, and they are unsustainable. Health care payers have recognized the substantial contribution of cancer medicines to the growth in cancer spending and have taken several steps to control expenditures :
- 1.
Coverage for specific treatments has been restricted. A decade ago, epoetin alfa and darbepoetin were the most costly clinic drugs for the Medicare program, accounting for more than $5 billion (or 23%) of all clinic drug expenditures. A change in the coverage policy was made in 2007 that restricted the use of these agents to selected patients. Although the need to make a change was prompted by cost, the new coverage decision was based only on what was medically reasonable and necessary for the Medicare population. As a result of the change, many oncologists had reported a substantial reduction in the use of these agents by 2009. Similar efforts to control costs by limiting overuse have been applied to other targeted cancer medications, such as trastuzumab.
- 2.
Reimbursement rates for specific medications have been reduced. In 2003, the Medicare Modernization Act reduced reimbursement for chemotherapy to 106% of the average national sales price over the previous two-quarters. Jacobson and colleagues demonstrated that this resulted in a significant reduction in the use of the agents most affected by this change (eg, paclitaxel and carboplatin) in the months leading up to its implementation. Private payers use several different mechanisms to change reimbursement rates, most often through the contractual arrangements they form with providers.
Hospitalizations are a second major driver for the growth of cancer care costs. Because this issue has a broad impact that extends well beyond patients with cancer, payers have engaged actively in efforts to limit hospitalization-related expenditures. For decades, payers have used bundled payments to reimburse a standardized payment amount for each admission based on the diagnosis, regardless of the length of stay or specific services provided during the hospitalization. Although this may reduce the cost per admission, it does not affect the overall number of admissions. To that end, payers are trying to identify potentially avoidable hospitalizations (eg, readmissions within 30 days or hospitalizations for ambulatory-care sensitive conditions), and they are introducing financial penalties to reduce the frequency of these events. The impact of these efforts on oncology patients and providers remains unclear. Unfortunately, current measures of avoidable hospitalizations have not been validated among patients with cancer. It may be harder to identify avoidable hospitalizations for patients with cancer because admissions are a frequent component of oncology care: for initial evaluation and management, symptoms and complications of the disease, scheduled treatments, and treatment-related adverse effects.
How we assess the value of medical treatments
The increasing costs and sometime marginal benefits of new cancer therapies have led to the assertion that some therapies may not always be worth what they cost. For example, among women with taxane- and anthracycline-resistant metastatic breast cancer, ixabepilone in combination with capecitabine increases progression-free survival by 1.6 months, compared with capecitabine alone. But at a price of more than $4000 per cycle, ixabepilone increases the average cost of treatment by more than $20,000. Is one progression-free month worth $12,000? Is this a good value? In the same population of women with previously treated metastatic breast cancer, eribulin adds as much as $25,000 to the cost of treatment, compared with a single-agent regimen, for an extension of 1.5 months of progression-free survival. If we are willing to pay $12,000 for an additional progression-free month, should we be willing to pay $16,000? How do we decide if these treatments provide value sufficient to justify their additional cost?
The preferred method for assessing the health benefits of medical interventions relative to their costs is CEA. This approach compares the incremental costs and the incremental health benefits of a new treatment with those associated with an older, standard treatment. The result is the incremental cost-effectiveness ratio (ICER), a comparative, standardized, objective description of the value associated with a new treatment. In a CEA, the effectiveness of an intervention is defined in nonmonetary units, such as cases of disease prevented, lives saved, or life-years saved. Survival outcomes may be adjusted to reflect quality of life, yielding a measure of effectiveness known as quality-adjusted life-years (QALYs). QALYs are a preferred metric for CEAs because they reflect the impact of an intervention on both morbidity and mortality and because they are comparable across treatment modalities and disease areas. These factors are important to consider, particularly when CEA results are used to inform policy decisions.
CEA has been applied to numerous interventions throughout the continuum of breast cancer care, from risk reduction and screening interventions to treatment modalities for early stage disease and supportive care for advanced disease. As demonstrated by the wide range of published ICER estimates, some breast cancer interventions offer substantial value, whereas others offer only a modest benefit at a very high cost. For example, adjusting all published estimates to 2012 US dollars, adjuvant tamoxifen for a 45-year-old woman with node-positive, Estrogen receptor (ER)-positive breast cancer is associated with an ICER of $7000 per QALY when compared with no therapy; adjuvant chemotherapy for a 45-year-old woman with node-negative, hormone receptor–negative breast cancer is associated with an ICER of $8000 per QALY when compared with no therapy. In the metastatic setting, adding bevacizumab to paclitaxel costs $245,000 per QALY compared with paclitaxel alone. For patients who have bony disease, denosumab costs $697,000 per QALY compared with zoledronic acid.
Comparing ICERs shows how the cost-effectiveness of an intervention may be strongly influenced by characteristics of the patient population (such as age and risk of recurrence), the way the intervention is applied (selectively or universally), and the treatment setting. For example, the ICER for contralateral prophylactic mastectomy (vs no prophylactic surgery) is about $5000 per QALY in 45-year-old women, but it is more than $100,000 per QALY in 65-year-old women. Targeted bisphosphonate therapy for fracture prevention in postmenopausal women receiving adjuvant aromatase inhibitor therapy has an ICER of approximately $92,000 per QALY, whereas universal bisphosphonate therapy in the same population costs almost $300,000 per QALY. The addition of trastuzumab to an adjuvant chemotherapy regimen for localized disease is associated with an ICER of $47,000 per QALY, whereas HER2 testing and the addition of trastuzumab to chemotherapy for metastatic disease are associated with an ICER of $185,000 per QALY.
CEAs and other methods can provide useful information about the comparative value of different medical interventions, but they do not inherently tell us how much is too much to spend or how much we should be willing to pay for health benefits. We still must decide where to draw the line. The frequently quoted threshold of $50,000 per QALY dates back at least to the early 1980s. This threshold has often been justified because it approximates the estimated ICER for renal dialysis in patients with end-stage renal disease. Following the Medicare program’s decision to cover this service, one could argue that it represents a societal threshold of willingness to pay for gains in population health. However, the persistence of this threshold fails to account for inflation over time. If we were willing to pay $50,000 per QALY in 1982, we should be willing to pay much more 3 decades later. Adjusting for overall inflation, $50,000 in 1982 now has a value that exceeds $115,000; adjusting for inflation based on the cost of medical goods and services specifically, this threshold approaches $200,000 in today’s dollars. By several other measures, societal willingness to pay for health gains in the United States is greater than $100,000 per QALY and is likely in the range of $140,000 to $200,000 per QALY.
Economic evaluations, such as CEAs, have been criticized as a step toward rationing and, therefore, denying care to patients in need. It is the application of a threshold ratio, rather than the method itself, that is, presumably, the cause of concern. However, using systematic approaches, like CEA, to understand the return on investments in health acknowledges the simple, but often ignored, reality that resources are limited. Every dollar spent on health care is a dollar not spent elsewhere. Recent statements from oncologists protesting the high cost of new cancer drugs and a formulary decision at one prominent hospital against a drug that yielded a similar magnitude of benefit at double the price of a competing drug suggest that these realities are becoming more difficult to ignore.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree