Vitamins, Minerals, and Dietary Supplements
1 Richard Stockton College, Galloway, NJ
2 Loma Linda University School of Medicine, San Diego, CA
3 City College of New York, New York, NY
The Need for Vitamins
Vitamins are organic chemical substances required for normal growth, development, and metabolism throughout all stages of life. Although humans mostly rely on exogenous sources of vitamins and minerals, certain intestinal microorganisms produce vitamin K and biotin, while vitamin D and niacin are synthesized from their chemical precursors, cholesterol and tryptophan, respectively.
As the importance of adequate vitamin balance for health and disease prevention has been increasingly discussed in the lay press, the annual expenditure for over-the-counter dietary supplements in the United States has grown to over $16 billion. Often these press articles highlight the findings of recently published research without contextualizing the information, misleading consumers into thinking that a new “magic bullet” for disease prevention has been discovered. Therefore, it is essential for clinicians to assume a role in patient education regarding supplements while simultaneously emphasizing the importance of a varied diet as the best source of most vitamins and minerals.
It is also important to look for those individuals who may have increased vitamin and mineral requirements or inadequate intake. These include, but are not limited to, pregnant and lactating women; growing children; the elderly; those who have suffered severe trauma such as burns, fractures, or major surgery; those who have or are at high risk for infections, such as HIV and malabsorption syndromes; excess consumers of alcohol, cigarettes, or illicit substance abusers; and those taking medications that may interfere with the absorption and/or metabolism of nutrients.
While vitamins are discussed here individually, including their deficiency symptoms and clinical uses, it should be noted that isolated vitamin deficiencies are rare, as are scientifically proven benefits of supplementation. Symptoms described for primary vitamin deficiencies (e.g., pellagra or beriberi) are unlikely to be seen in clinical practice in developed countries (except in rare cases of extreme nutritional depletion), but mild relative deficiencies of individual or multiple vitamins may be more common than we suspect. This is because many of the vitamins work synergistically together making clinical efficacy for individual supplements difficult to establish. For example, folic acid, B6, and B12 have been used together to lower homocysteine levels (with unclear benefits to cardiovascular disease). Riboflavin is involved in pyridoxine, niacin, folate, and vitamin K metabolism. Vitamins C, E, and selenium have been tested as an antioxidant “cocktail” but have not reduced cancer incidence or recurrence. In spite of numerous negative clinical trials, patients continue to optimistically consume supplements in efforts to treat or prevent disease. Many patients feel better taking vitamins, and attempts to convince them of their lack of utility are unlikely to be worth the effort. Even lacking clinical trial data, it is impossible to prove that a specific supplement is not effective in a particular individual. Given our current inability to determine individual vitamin requirements, more specific advice regarding helpful vitamin or mineral supplementation for specific patients awaits the development of individualized medicine (which will continue during the practice lifetime of the student readers of this text).
Vitamin Intake Standards
Vitamin and mineral requirements change throughout the stages of life. The Food and Nutrition Board of the National Research Council established a Recommended Daily Allowance (RDA) for most nutrients based on a review of published scientific data. A considerable body of knowledge exists for certain vitamins and minerals, and RDAs for various gender and age categories have been established. The RDA levels are set at two standard deviations above the mean requirement to cover the needs of practically all healthy persons.
It is important to note two caveats with regard to these recommendations. The first is that suggested levels were established for groups of healthy people. Thus, the requirements of any specific individual or for those with special nutritional needs due to medical conditions are not addressed. Second, the RDAs were developed with prevention of classic nutrient deficiencies in mind, rather than health enhancement or optimization of well-being. Active areas of research include developing vitamin requirements for patients with acute or chronic disease and determining the potential for supplements to improve health.
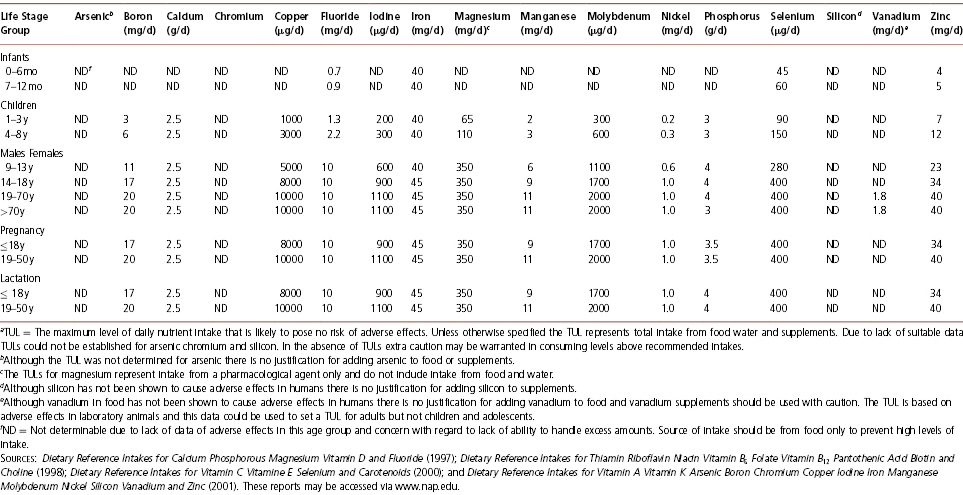
To address the changing needs for information, the Institute of Medicine of the National Academy of Sciences established the first Dietary Reference Intakes (DRIs) in 1997. The new DRIs move beyond the traditional RDAs to focus on the prevention of chronic disease. See Tables 2-1, 2-2, and 2-3. Dietary Reference Intake is a collective term that refers to three nutrient-based dietary reference values for every stage of life and both genders in addition to the conventional RDA: Estimated Average Requirement (EAR), Adequate Intake (AI), and the Tolerable Upper Intake Level (TUL).
Table 2-1 Dietary Reference Intakes (DRIs): Recommended Intakes for Individuals, Vitamins (Food and Nutrition Board, Institute of Medicine, National Academies)
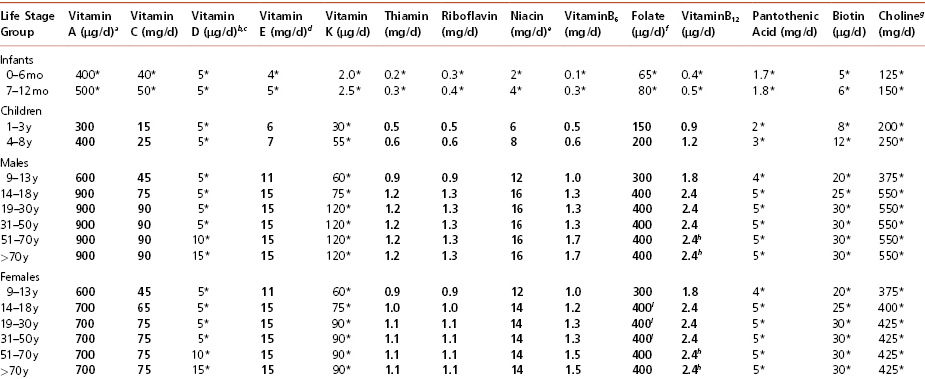
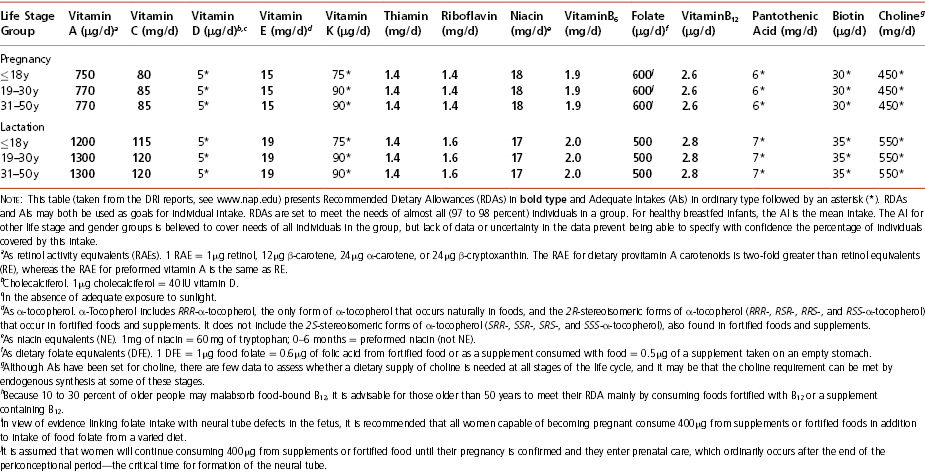
Table 2-2 Dietary Reference Intakes (DRIs): Recommended Intakes for Individuals, Elements (Food and Nutrition Board, Institute of Medicine, National Academies)
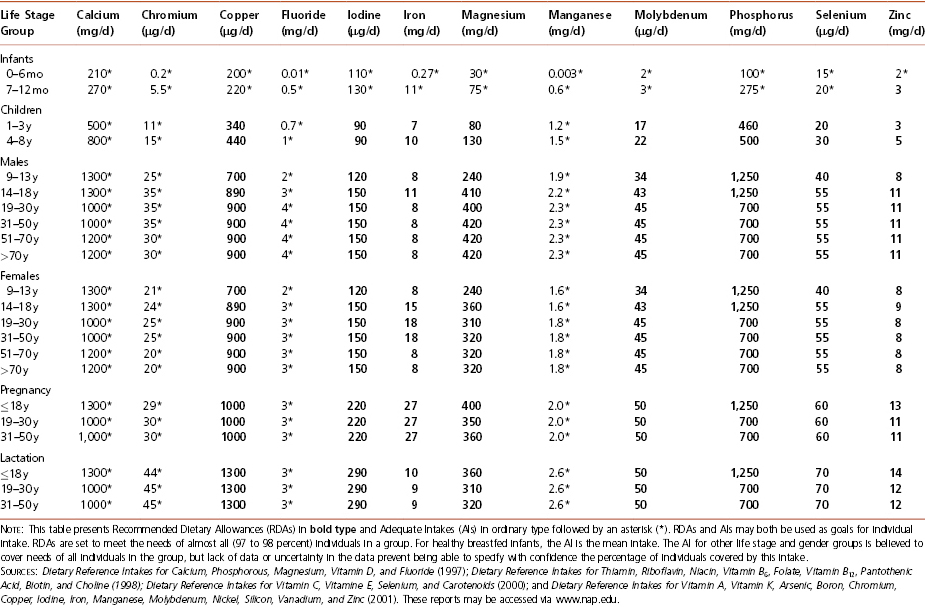
Table 2-3 Dietary Reference Intakes (DRIs): Tolerable Upper Intake Levels (TULa), Vitamins (Food and Nutrition Board, Institute of Medicine, National Academies)
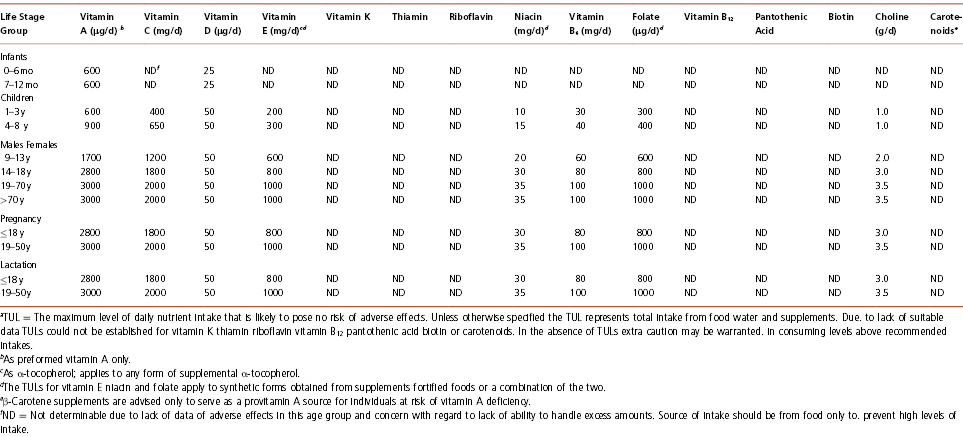
Table 2-3 (continued) Dietary Reference Intakes (DRIs): Tolerable Upper Intake Levels (TULa), Elements (Food and Nutrition Board, Institute of Medicine, National Academies)
Estimated Average Requirement (EAR)
The EAR is the most useful DRI for assessing the nutrient intake of a population. This is the daily intake expected to meet the requirement of 50 percent of individuals in a particular life-stage and gender category. Individuals are advised to take in the EAR plus two standard deviations (the RDA) to ensure that their intake is adequate. An individual whose mean intake is below the EAR is, on average, getting insufficient amounts of that nutrient.
Adequate Intake (AI)
The AI is an approximation of the average nutrient intake by a population or subgroup that seems to be healthy and not at increased risk of a particular chronic disease. The AI is a rough equivalent of the RDA, but is based upon estimation where adequate data for determining an EAR are unavailable.
Tolerable Upper Intake Level (TUL)
The TUL is the level of daily nutrient intake that is unlikely to pose risks of adverse health effects to almost all (97 to 98 percent) individuals in a specified life-stage and gender group. These levels, taken together, allow one to estimate a range of safe levels for supplementation.
The Vitamins
Vitamin A
Vitamin A is a group of fat-soluble compounds that includes retinoic acid, retinol, and carotenoids. Retinol, also known as pre-formed vitamin A, is the most active form and is found mostly in foods of animal origin. Beta-carotene, also known as provitamin A, is the most common of the plant carotenoids, and is converted in the body to retinol.
Forms and Absorption Following ingestion of beta-carotene (or other carotenoids), the body enzymatically cleaves some of these compounds to retinol, which is esterified in the intestinal cell to retinyl esters that, along with the remaining carotenoids, are incorporated into chylomicrons in the enterocytes for transport into the lymphatics and eventually the blood. Dietary retinyl esters follow a similar path and are likewise incorporated into chylomicrons, eventually delivering the retinyl esters and carotenoid pigments to the liver for storage. When a particular part of the body, such as the eyes, requires vitamin A, the liver releases the retinol, bound to retinol binding protein (RBP).
Function Vitamin A plays an essential regulatory role:
- in the development or maintenance of the mucus membranes, cornea, and conjunctiva in the eye,
- in a process known as phototransduction; all-trans retinal is linked to a protein to form rhodopsin in the rod cells and iodopsin in the cone cells of the retina; these cells are required for night vision and the perception of color in bright light,
- in the normal integrity and growth of skin and tissue cells, including the mucus membranes of the mouth, intestinal, respiratory, genitals, and urinary tracts,
- in the production of keratin, a component of skin and epithelia,
- in the form of all-trans retinoic acid, which assists in the functioning of testicles and ovaries and aids in the development of the embryo,
- as an antioxidant (many carotenoids function as antioxidants).
Retinol Equivalents Vitamin A is ingested either as pre-formed vitamin A (retinol or retinyl ester), or a beta-carotene that can be split into retinol in the intestine. Beta-carotene is the most abundant carotenoid present in green, yellow, and orange fruits and vegetables. Due to inefficient conversion, 12 µg of beta-carotene in food yields only about 1 µg retinol, and therefore a serving of food that contains 12 µg of beta-carotene is said to contain 1 µg RAE (retinol activity equivalent; older literature uses a similar concept with the abbreviation RE, for retinol equivalent). Because other carotenoids are even less efficiently converted to retinol, 1 µg RAE equates to 24 µg of these other carotenoid species.
International units (IU) are also used to express the amount of vitamin A in supplements and occasionally in foods; 100 IU of retinol in supplements translates to 30 µg RAE, while 100 IU of beta-carotene equates to 5 µg RAE.
Deficiency Vitamin A deficiency is one of the most common forms of malnutrition worldwide, with infants and young children most affected. Primary deficiency is due to inadequate intake of vitamin A and its precursors, whereas secondary deficiency occurs from poor absorption of fat-soluble vitamins, which may occur in patients with cystic fibrosis, Crohn’s disease, tropical sprue, or liver disease, or in those with excessive alcohol intake.
Clinical problems associated with vitamin A deficiency include perifollicular hyperkeratosis, night blindness, xerophthalmia (which can progress from conjunctival thickening to corneal ulceration and eventual irreversible blindness), and impairment of both humoral and cell-mediated immunity; this latter effect is known to increase mortality from certain infectious diseases, such as measles, in developing countries.
Toxicity Chronic excesses in vitamin A intake of 30 mg/day (100,000 IU/day) or acute doses of 150 mg (500,000 IU) can cause a variety of symptoms ranging from bone and skin changes and liver abnormalities (hepatomegaly) to headache, nausea, vertigo, blurred vision, and lack of muscle coordination. Recently, attention has been directed at elucidating whether chronic vitamin A intake only modestly higher than recommended levels might have adverse effects on bone health and the risk of osteoporosis. Research results have been mixed and complicated by inadequate measures of vitamin A status. However, vitamin A intake tends to be adequate or more than adequate in the United States, and supplementation with preformed vitamin A resulting in total intake which exceeds the RDA should be discouraged. A recent case of hypervitaminosis A which resulted in liver damage, was caused by ingesting a combination of a nutrition shake as a meal replacement and multivitamins over an extended period of time.
Consuming too much vitamin A, especially retinoic acid, during the first trimester of pregnancy can cause birth defects to the developing embryo. Therefore, women who are using vitamin A for the treatment of acne, or for other purposes, require reliable forms of birth control.
Because only limited amounts of carotenoids are converted to vitamin A, excessive intake of beta-carotene has not been shown to produce toxic effects. People who consume large doses of beta-carotene, either through dietary sources or supplements, may develop a yellow tinge to the skin. This carotenosis, commonly seen in babies whose caretakers give them squash and sweet potatoes as their predominant early solid food, has no harmful effects. While many in vivo and in vitro studies have supported a link between vitamin A and the treatment of epithelial cancers, intervention trials have been disappointing.
Supplement Issues Certain forms of vitamin A, specifically the all-trans form of retinoic acid, have proven useful for the treatment of dermatological disease such as acne and psoriasis, presumably because of their effects on gene expression and cell differentiation. Retinoic acid has also been found to be effective in the treatment of acute promyelocytic leukemia; however, studies attempting to establish a role for retinoic acid in the treatment of other cancers have generally been disappointing. Retinol supplementation has been shown to decrease the risk of melanoma in women but there was no reduction in those with a higher dietary intake of retinol or those taking carotenoid supplements. High serum levels of vitamin A have been linked to a lower incidence of non-Hodgkins lymphoma and vitamin A supplements have been shown to decrease the risk of cervical cancer in women. While higher serum levels of carotenoids have been associated with a lower risk of coronary heart disease (CHD), randomized trials of beta-carotene have shown no benefit for the prevention of acute myocardial infarction (AMI). Long-term use of a multivitamin supplement, however, has been linked to a decrease in the rate of heart attacks in women with no history of previous cardiovascular disease.
Vitamin A plays an important role in the health of children. Children with sickle cell disease (SC) have been shown to have lower serum vitamin A levels but supplementation with the recommended daily amount did not improve the vitamin A status. This suggests supplementation at larger than recommended amount may be needed to correct blood levels for those with SC. Vitamin A is commonly prescribed to nursing mothers who might be deficient to improve the health of the baby and reduce morbidity and sickness in parts of the developing world. Vitamin A supplementation has been shown to result in a decrease in hearing loss in children at risk for poor nutrition. Pre-term birth caused by bacterial vaginosis was reduced with vitamin A supplementation. Lung function was improved for children from an undernourished population when the mother had taken a vitamin A supplement during pregnancy.
Vitamin A Food Sources See Appendix A.
Vitamin D
Vitamin D is a fat-soluble vitamin, naturally occurring in two forms: vitamin D2 (ergocalciferol) and vitamin D3 (cholecalciferol). Vitamin D2 is a plant or yeast steroid commonly used to fortify milk, while vitamin D3 is from animal sources or produced in the skin upon exposure to adequate amounts of sunlight. Recent literature reviews indicate that these two forms may not be equivalent; one study concluded that vitamin D2 potency is less than one-third that of vitamin D3. Over the past few years there has been an explosion of research on the importance of vitamin D and the health effects of marginal levels. This has led to a marked increase in healthcare providers measuring and correcting serum vitamin D levels in their patients.
Forms and Absorption Since vitamin D is fat-soluble, some fat is required in the diet for its absorption, and fat malabsorption conditions adversely affect vitamin D absorption. Once absorbed it is transported to the liver as a component of chylomicrons or bound to vitamin D binding protein (DBP), where it undergoes hydroxylation to 25-hydroxy vitamin D [25(OH)D or calcidiol]. Further conversion to its physiologically active form, 1,25-dihydroxy-vitamin D [1,25(OH)2D or calcitriol], takes place in the kidneys or in target tissues. The synthesis and metabolism of vitamin D are closely coupled to calcium homeostasis; therefore, when calcium levels in the blood are low, the body releases parathyroid hormone (PTH), which stimulates the kidney to convert 25(OH)D to 1,25(OH)2D. Elevations in 1,25(OH)2D stimulate the gastrointestinal tract to increase calcium absorption from about 10 to 30 percent and phosphorous absorption from about 60 to 80 percent. Serum 25(OH)D is the best indicator of vitamin D status. It reflects vitamin D produced cutaneously and that obtained from food and supplements, and has a half-life of 15 days.
Units The most common unit reported for vitamin D is International Units (IU). Vitamin D may also be listed in micrograms (µg). Use the following conversion: 1 µg = 40 IU.
Functions Vitamin D plays an essential regulatory role in:
- intestinal absorption of calcium and phosphorus,
- regulation of calcium and phosphorous deposition in the bones, teeth, and cartilage in children and adults,
- maintenance of blood calcium and phosphorus levels,
- a variety of physiological functions, including immunity, neuromuscular functions, blood pressure regulation, insulin production, reduction of inflammation, and apoptosis.
Deficiency Vitamin D deficiency can be due to impaired availability of vitamin D (inadequate dietary intake or fat malabsorptive disorders, coupled with a lack of sun exposure) or impaired metabolism (in the liver, kidney, or end organs). Serum levels less than 20 ng/mL are indicative of low serum vitamin D. Groups with increased risk for low vitamin D levels are breastfed infants, older adults, obese individuals (BMI > 30 kg/m2), people with dark skin, and those with limited sun exposure. Five to 30 minutes of sun exposure between 10 a.m. and 3 p.m. at least twice a week without sunscreen has been suggested to provide sufficient vitamin D synthesis in temperate zones. Studies in healthy college and medical students in Boston have documented deficient serum levels at the end of winter. Strict vegetarians and those who have a milk allergy or lactose intolerance, are also at risk. Older adults and seniors are at increased risk for vitamin D deficiency, especially those who are bed-ridden or who live in nursing homes and so may not have adequate exposure to sunlight coupled with inadequate dietary intake. Reduced levels of vitamin D in the second trimester have been shown to increase the risk of pre-clampsia in pregnant women and have been found in women with breast cancer.
Vitamin D deficiency results in rickets in infants and children and osteomalacia (softening of the bones) in adults. Rickets causes retarded growth, swelling and tenderness at the ends of the bones, and malformation of the joints. Rickets in infants also leads to a delay in the closure of the skull bones, possibly leading to a larger skull (“frontal bossing”), as well as bowed legs, pigeon breast, and beaded ribs (“rachitic rosary”) seen in older children. Osteomalacia may lead to pain in the legs, ribs, hips, and muscles, and easily breakable bones. Osteomalacia may occur when long-term anticonvulsant medications such as phenobarbital or phenytoin are taken because they increase the liver’s breakdown of vitamin D. Individuals with chronic kidney disease often develop osteodystrophy, secondary to the kidney’s inability to convert vitamin D to its active form and hyperparathyroidism aggravated by the lack of activated vitamin D.
Toxicity Chronically elevated doses of vitamin D may lead to kidney stones, nausea, headaches, weakness, anorexia, frequent urination, weight loss, irregular heartbeat, and weak bones and muscles. Excess levels may also lead to an elevation in serum calcium, which can cause calcification of soft tissues such as organs and blood vessels, possibly resulting in irreversible damage. In infants and children, too much vitamin D can lead to retarded growth, rounding of the skull, mental retardation, and death. However, excessive levels of vitamin D are believed to occur only through the use of supplements rather than from food or too much sun exposure. The tolerable upper limit for vitamin D has been established at 50 µg/day (2000 IU/day) but recently, vitamin D researchers have questioned whether this level is set too low.
Supplement Issues Vitamin D supplements are available in two forms: D2 and D3. Vitamin D3 has been shown to be more effective at raising and maintaining serum 25(OH)D levels. A meta-analysis of randomized controlled trials indicated that vitamin D3 supplementation led to a decreased risk of all-cause mortality with a relative risk of 0.93. The mean daily dose was 528 IU (with a range of 300 to 2000 IU). Although the mechanism for this is unclear, studies have suggested that the risk for certain cancers (notably colorectal and breast) may be significantly reduced in individuals with higher than normal serum levels of vitamin D, corresponding to intakes of 1000 to 4000 IU/day. Studies with supplement dosages at the current RDA levels (400 IU/day) showed no benefit, but arguments have been made that the RDA is too low and that the upper limit of 2000 IU/day is too restrictive and could be raised by a factor of five. Compounding the problem is that the vitamin D content of most foods is quite low, and even 8 ounces of milk provides only 100 IU. Five to 30 minutes of sun exposure several times a week yields blood levels of vitamin D much higher than is achievable orally, and is argued to represent the “natural” level for this vitamin. The level of 25(OH)D has been shown to be affected by the types of fat in the diet when vitamin D is taken as a supplement: those high in monounsaturated fats resulted in higher levels than those high in polyunsaturated fats. In 2011, the Food and Drug Administration (FDA) warned consumers to stop taking a vitamin D supplement called Soladek, due to several reported cases of vitamin D toxicity.
Studies of the effect of vitamin D on fractures showed no benefit at the standard dosage of 400 IU/day, but recent meta-analyses of studies using higher vitamin D dosages (800 IU/day or greater), when accompanied by significant calcium supplementation, show significant reductions in hip fractures (18 percent to 24 percent). (See Chapter 4 for current vitamin D recommendations for infants and children.)
Inadequate levels of vitamin D have been associated with a number of prevalent health conditions. Vitamin D has been shown to accelerate the resolution of the inflammatory response in those receiving treatment for tuberculosis. Vitamin D supplements were also shown to decrease the incidence of metabolic syndrome in young adults. Lower levels of vitamin D have been observed in older women with heart disease, hypertension, and those who develop Alzheimer’s disease compared to women of the same age without the disease. Reduced levels of vitamin D also were observed in menopausal women with depression. A recent study that requires confirmation has demonstrated reductions in blood pressure and measures of depression among women with type 2 diabetes.
Vitamin D Food Sources See Appendix B.
Vitamin E
Vitamin E is another fat-soluble vitamin group consisting of alcohol compounds called tocopherols and tocotrienols. Each of these exist in alpha, beta, gamma, and delta forms for a total of eight compounds with vitamin E activity. Each of the eight compounds have two racemic forms “d” and “l,” so supplements are labeled “d-alpha” or “l-alpha.” Of the various tocopherols, alpha-tocopherol has the highest biological activity and only the d-isomer is physiologically effective.
Forms and Absorption Vitamin E is absorbed passively in the ileum, requiring the presence of bile salts and dietary fat, as with all of the fat-soluble vitamins. Once absorbed, vitamin E is incorporated into chylomicrons for delivery to the liver and other tissues.
Functions Vitamin E plays an essential regulatory role in:
- antioxidant activity; protection of polyunsaturated fatty acids within cell membranes from peroxidation,
- inhibition of cell proliferation, platelet aggregation, and monocyte adhesion,
- assisting in the maintenance of fertility.
Alpha-tocopherol has also been shown to inhibit protein kinase C, thereby promoting differentiation of smooth muscle cells and potentially reducing the damage to endothelial cells caused by blood-cell components adhering to them.
Deficiency Vitamin E deficiency is rare, except in people who cannot absorb fat, for example patients with cystic fibrosis or pancreatic insufficiency. Clinical signs include neurologic dysfunction, loss of deep tendon reflexes, and diminished vibratory or position sense. A conditional deficiency may be created in premature infants treated with oxygen who may develop retrolental fibroplasias, leading to visual impairment and possibly blindness. This may be prevented by vitamin E supplements. The National Health and Nutrition Examination Survey (NHANES) studies have documented that most Americans seem to take in less than the RDA of vitamin E but this may be inaccurate because of failure to adequately account for added fats and oils.
Toxicity Vitamin E is considered non-toxic except at very high doses. Reports indicate that very large doses of vitamin E can interfere with the vitamin K formation of functional clotting factors, resulting in hemorrhage. For this reason, large doses of vitamin E should be avoided 2 weeks before and after surgery as well as when taking anticoagulation medications, such as Coumadin. It has also been reported that premature infants may be especially sensitive to excess vitamin E, with overdose resulting in hemorrhage and sepsis. The TUL for vitamin E has been established at 1000 mg/day. Excess levels of vitamin E taken by pregnant women has been linked to an increase in children with congenital heart defects.
Relationship to Disease Prevention Vitamin E is considered to be nature’s most effective lipid-soluble antioxidant, protecting cell membranes from oxidative damage. Promising in vitro and case-control studies led to vitamin E supplements becoming very popular to prevent heart disease, but more recent large clinical trials have failed to demonstrate any benefit from vitamin E in reducing the risk of heart attacks or deaths from heart disease. Despite previous reports, recent studies have shown that vitamin E supplementation has no effect on macrovascular outcomes or mortality in diabetic patients who smoke. Daily supplementation with vitamin E has been reported to increase the risk of prostate cancer in men. With disappointing results from alpha-tocopherol studies, research interest (and speculative supplementation), has shifted to gamma-tocopherol, but no large-scale studies on its efficacy are available. The theory is that alpha-tocopherol supplements may be counter-productive because they cause lower serum levels of gamma-tocopherol.
Vitamin E Food Sources See Appendix C.
Vitamin K
Vitamin K is a fat-soluble vitamin that is obtained from dietary sources and is produced by intestinal bacteria. Phylloquinone is the predominant form of vitamin K from dietary sources while menaquinone is produced by gut micro-flora. The difference between the two forms has to do with the side chain off of the napthoquinone rings.
Forms and Absorption Absorption of vitamin K occurs primarily in the proximal small bowel and requires bile salts. Following intestinal absorption, vitamin K is transported by chylomicrons for storage mostly in the liver.
Function Vitamin K is a required cofactor for enzymes involved in the post-translational carboxylation of glutamate moieties in proteins involved in clotting and bone mineralization. Vitamin K allows the formation of calcium-binding gamma-carboxyglutamate (gla) that binds calcium and is required for the activity of factors VII, IX, X, and prothrombin as well as osteocalcin and gla matrix protein. Additionally, anticoagulant proteins S and C require vitamin K for their activity.
Deficiency Deficiency of vitamin K in otherwise healthy individuals is rare, but may occur in people with fat malabsorption or those on prolonged antibiotic therapy, due to the disruption of the intestinal microbiota that produce vitamin K. Symptoms of vitamin K deficiency include signs of impaired coagulation such as easy bruisability, mucosal bleeding, melena, and hematuria.
A recent observational study suggested that a low plasma level of vitamin K might be associated with a higher prevalence of osteoarthritis of the hands and knees. Also, a meta-analysis of randomized controlled trials suggested that vitamin K supplementation reduced bone loss, with a positive effect on fractures.
Infants are given a vitamin K injection at birth to prevent hemorrhagic disease. Infants’ intestinal tracts lack the necessary bacteria to synthesize vitamin K adequately until approximately 1 week after birth and the newborn liver is therefore unable to produce adequate levels of coagulation factors.
Toxicity Toxicity to phylloquinone or menaquinone is virtually unknown, although allergic reactions to mega doses of vitamin K have been reported. Severe jaundice may occur in infants treated with doses of menadione. There is no tolerable upper level for vitamin K. Patients taking warfarin (Coumadin) as an anticoagulant are cautioned to avoid marked changes in their intake of vitamin K-rich foods or supplements since the dose of Coumadin is titrated to maintain a narrow range of anticoagulation, which may be reversed by increased intake of vitamin K.
Vitamin K and Disease Prevention Studies of elderly patients with osteoporosis have demonstrated greater rates of vitamin K insufficiency, but long-term clinical trials with vitamin K supplements have produced mixed results regarding potential benefits in preventing osteoporosis. There may be differences in obtained results based on the source of vitamin K (dietary vs endogenous). Recent work indicates that very little of the vitamin K produced by intestinal bacteria is absorbed and that fermented foods may be a better source of menaquinone.
Vitamin K Food Sources See Appendix D.
Ascorbic Acid (Vitamin C)
Ascorbic acid is a water-soluble vitamin commonly known as vitamin C. It is the least stable of all the vitamins, and is easily destroyed during cooking and processing.
Form and Absorption The jejunum and ileum efficiently absorb vitamin C. The amount of vitamin C in the blood is modulated by renal excretion, with levels exceeding the reabsorption threshold being excreted in the urine.
Functions Vitamin C plays an essential role in:
- the formation of collagen, which is responsible for strengthening bones and blood vessels, anchoring teeth into the gums, as well as forming the substances necessary for body growth, tissue repair, and wound healing,
- the synthesis of neurotransmitters such as norepinephrine,
- antioxidant activity.
Deficiency Individuals who do not have access to fresh citrus fruits and juices, such as urban or poor older adults, may have insufficient vitamin C intake. Individuals with severe burns, fractures, pneumonia, rheumatic fever, and tuberculosis, as well as those who have recently undergone surgery, have increased requirements for vitamin C. Alcohol decreases absorption and cigarette smoking depletes tissue levels. Thus, alcoholics and smokers should increase their dietary intake or take supplemental vitamin C.
Vitamin C deficiency is characterized by the development of scurvy, in which impaired collagen synthesis results in muscle weakness, joint pain, impaired wound healing, loose teeth, bleeding and swollen gums, bruised skin, fatigue, and depression.
Toxicity Since vitamin C is water-soluble, the body excretes the excess when intake exceeds the body’s requirements. However, because vitamin C is metabolized to oxalic acid, consuming too much may cause increased excretion of oxalate, which suggests that patients with a history of forming oxalate kidney stones should avoid high doses of this vitamin. Doses in excess of the UL (2000 mg/day) can have other side effects including nausea, diarrhea, and abdominal cramps.
Relationship to Disease Prevention Vitamin C is a powerful antioxidant that provides the first line of defense against free radicals in the aqueous compartments of the body. However, to date, studies have been unable to demonstrate a clear protective role for vitamin C. Numerous studies of even mega doses have not proven effective in cancer prevention or treatment or in atherosclerosis prevention. One study of women undergoing breast cancer therapy demonstrated an 18 percent reduction in mortality and a 22 percent reduction in recurrence in women using antioxidants (vitamins E and C), and a multivitamin. The role of vitamin C in the prevention and treatment of the common cold remains controversial with high doses having a mild antihistamine effect, but many patients are convinced of the benefits of daily supplementation. Increased levels of vitamin C from either the diet or from supplements have been associated with lower blood pressure.
Vitamin C Food Sources See Appendix E.
Thiamin (Vitamin B1)
Form and Absorption Thiamin is a water-soluble vitamin. It is primarily absorbed in the jejunum via active transport when intake levels are low and passive transport when intake levels are high. Absorption is significantly reduced in the presence of alcohol and in individuals with folate deficiency. Once absorbed, thiamin is primarily found in skeletal muscles, liver, heart, kidneys, and brain; however, it is not stored in the body to any great extent, so daily intake is required.
Functions Thiamin is an essential prosthetic group in a number of enzymes that play key roles in the production of energy from carbohydrate and protein and is an essential component in the pentose phosphate pathway that generates NADPH and ribose for nucleic acids.
Deficiency Primary thiamin deficiency due to poor intake of thiamin-containing foods, which can lead to beriberi, is rare in the United States because the majority of grain products are fortified with thiamin. However, thiamin deficiency may occur in individuals who abuse alcohol because excessive alcohol intake significantly decreases thiamin absorption and interferes with its metabolism. Early thiamin deficiency is characterized by poor appetite, irritability, apathy, confusion, and weight loss. Clinicians should be aware of low micronutrient intake among patients on weight-loss regimens as the recent A-to-Z study comparing the Atkins, Ornish, LEARN and Zone diets demonstrated decreased intake and blood levels of thiamin in patients following either the Atkins, LEARN or Ornish plans. For this reason, a multivitamin should be advised for patients restricting their diet for weight loss or other reasons. Advanced stages of beriberi are characterized by the system affected: neurologic or cardiovascular systems. Wet beriberi refers to a form characterized primarily by abnormal heart rhythms, cardiomyopathy, heart failure, and edema. The neurological manifestations vary from pain, numbness or tingling of the lower extremities to difficulty walking and loss of deep tendon reflexes, to Wernicke’s encephalopathy or Korsakoff’s psychosis.
Causes and Effects of Toxicity Thiamin toxicity has not been described.
Relationship to Disease Prevention Although thiamin is not generally associated with disease prevention, prompt administration of thiamin is indicated for the alcoholic patient who shows signs of Wernicke’s disease, and is often used presumptively in patients who have acute mental status changes.
Riboflavin (Vitamin B2)
Riboflavin is water soluble. It functions as a precursor to the flavin category of enzyme prosthetic groups – flavin-adenine dinucleotide (FAD) and flavin mononucleotide (FMN) – that participate in oxidation/reduction reactions, many of which are involved with energy production.
Form and Absorption Free riboflavin is released from foods by digestive enzymes and is actively absorbed by an ATP-requiring process in the jejunum. Some of the riboflavin circulating in the blood is loosely bound to albumin, although significant amounts also combine with other serum proteins. Once riboflavin is delivered to a variety of cells, it is converted into FMN or FAD.
Functions Riboflavin plays an essential role in:
- normal growth and development,
- breakdown of glucose to yield energy for all cells,
- facilitation of glycogen production and digestion of fats,
- synthesis of niacin from tryptophan,
- maintenance of normal mucous membranes and protection of the nervous system, skin, and eyes,
- metabolism of vitamin K, folate, and pyridoxine.
Deficiency Riboflavin deficiency can result from inadequate intake, lack of absorption, poor utilization, or increased excretion. Riboflavin deficiency symptoms include inflammation of the oral mucosa or tongue, cheilitis, stomatitis, glossitis, seborrheic dermatitis, and normochromic-normocytic anemia. The eyes may become bloodshot, itchy, watery, and sensitive to bright light. Riboflavin deficiency typically develops in conjunction with deficiencies of other water-soluble (B) vitamins, which are commonly found in the same foods. In those with reduced riboflavin levels, supplementation has been shown to lower total plasma homocysteine. High homocysteine levels are associated with an increased risk of cardiovascular disease (CVD), but B vitamin supplements have not proven successful at lowering CVD in experimental trials.
Toxicity No adverse effects from a high intake of riboflavin have been reported and hence there is no TUL established for this vitamin. Riboflavin in brightly pigmented and causes a very yellow urine in patients taking it.
Relationship to Disease Prevention There are no specific indications for riboflavin supplementation for disease prevention, but at-risk groups include those with high alcohol intake and the elderly, particularly those with limited income who may have poor dietary intake.
Niacin (Vitamin B3)
Niacin is a water-soluble vitamin, found in two common forms: nicotinic acid and nicotinamide. Niacin is the precursor to the coenzymes nicotinamide adenine dinucleotide (NAD) and NAD phosphate (NADP), electron carriers used in synthetic reactions and for ATP production.
Form and Absorption Niacin and nicotinamide are absorbed through the intestine by passive diffusion. Niacin and nicotinamide are metabolized via different pathways.
Functions Niacin plays an essential role in:
- normal enzyme production in at least 200 reactions in the body involved in energy production; most enzymes require niacin to accept electrons (redox) or donate hydrogen molecules (hydrogenase),
- normal production and breakdown of glucose, fats, and amino acids, thereby helping the body to metabolize these substances,
- normal development, maintenance, and function of the skin, gastrointestinal tract, and nervous system,
- synthesizing DNA.
Deficiency Niacin is found primarily in protein-rich foods, and a deficiency is rare in the United States. Because some, but not all, of our niacin requirement can be met by conversion from the amino acid tryptophan, niacin deficiency historically developed in those whose diet mainly consisted of corn, which is both low in niacin and lacks tryptophan. The synthesis of niacin from tryptophan requires riboflavin, pyridoxine, and heme-iron-containing enzymes, therefore vitamin B6 deficiency can also contribute to a niacin deficiency. Individuals who abuse alcohol are also at increased risk of niacin deficiency because alcohol significantly reduces niacin absorption.
The initial signs of niacin deficiency include fatigue, loss of appetite, weakness, mild gastrointestinal disturbance, anxiety, irritability, and depression. A severe deficiency causes pellagra (“rough skin”) showing symptoms of diarrhea, dermatitis (pigmented skin rash, especially to sun-exposed skin), dementia, and if left untreated, death (“4 Ds”). Additional symptoms include inflammation of the mucous membranes of the mouth (magenta tongue), apathy, fatigue, and loss of memory.
Toxicity Niacin toxicity from food sources has not been documented. Pharmacologic doses of niacin used to treat hypercholesterolemia (lowers LDL and raises HDL) commonly cause minor adverse effects, including flushing, nausea, salivation, and dizziness. Based on estimated minimum levels that produce these symptoms, a TUL for niacin has been established at 35 mg/day. Niacin at pharmacological doses (>2000 mg/day) over a long period has been associated with elevated liver enzymes and elevated blood sugar levels in some individuals.
Recently, it has been reported that individuals seeking to “beat” urine drug screening have presented at Emergency Departments with symptoms of niacin toxicity, sometimes life-threatening. This misguided use of niacin at levels exceeding even usual pharmacologic doses have resulted in symptoms ranging from nausea and vomiting to metabolic acidosis and electrocardiogram abnormalities.
Relationship to Disease Prevention In addition to hypercholesterolemia, niacin has been used to treat dizziness and tinnitus, and to prevent premenstrual headaches. Pharmacological doses of nicotinic acid (between 1 and 3 g/day) have demonstrated utility in clinical trials at reducing CVD. Nicotinamide does not have this effect. When applied to the skin, niacin has recently been shown to improve the appearance of wrinkles around the eyes and in combination with N-acetyl glucosamine, has been used to decrease irregular pigmentation of the skin and to decrease the immunosuppression observed with exposure to ultraviolet light. Side effects of mega doses of niacin include flushing, which may be minimized by administering an aspirin prior to ingesting each dose of niacin or by using a sustained release preparation. Both niacin and niacinamide have been used topically but itching and burning of the skin may occur.
Pantothenic Acid
Pantothenic acid is another B-complex vitamin. It is a precursor of coenzyme A (CoA) and the acyl-carrier protein (ACP) moiety of the enzyme fatty acid synthase, both necessary for the metabolism of fats, carbohydrates, and proteins. CoA derived from food is hydrolyzed in the small intestine to form pantothenic acid, which is then absorbed in the jejunum.
Functions Pantothenic acid, as a component of CoA, is essential for:
- synthesis of fatty acids, triglycerides, cholesterol, and acetylcholine,
- metabolism of protein and amino acids, fat, and carbohydrates,
- synthesis of cell membranes.
Deficiency Lack of pantothenic acid in the body is very unlikely and there is no evidence that a deficiency of this vitamin can occur naturally. However, a deficiency created experimentally in test subjects has produced the following symptoms: indigestion, abdominal pain, burning sensation in the feet, arm and leg cramps, insomnia, and nerve inflammation (neuritis). Damage to the adrenal cortex, nervous system, skin, and hair has also been observed. It is thought that alcoholics may exhibit neuritis due to a lack of pantothenic acid; however, further evidence is needed for confirmation.
Toxicity Unknown.
Relationship to Disease Prevention While many people take pantothenic acid supplements as part of “stress” formulas, to treat rheumatoid or osteoarthritis, acne, or as a immune booster due to its role in the synthesis of adrenal hormones, the National Institutes of Health (NIH) has concluded that there is insufficient scientific evidence to determine its effective for these uses.
Biotin
Biotin is also a member of the water-soluble B-complex of vitamins.
Forms and Absorption Biotin is absorbed in the proximal small intestine. Intestinal bacteria also synthesize biotin, which can contribute to body stores.
Functions Biotin is an important prosthetic group in the carboxylase class of enzymes, which use bicarbonate to attach a CO2 group onto various metabolic substrates; as such, biotin plays a key role in glucose synthesis.
Deficiency Biotin deficiency in humans is rare. Experimentally, biotin deficiency has developed in humans who consume large quantities of raw egg whites. The protein avidin in eggs binds to biotin in the intestine preventing absorption. Symptoms of biotin deficiency include inflammation of the skin, hair loss, muscle pain, increased skin sensitivity, loss of appetite, nausea, mental problems, high cholesterol, and decreased hemoglobin levels. Low levels of biotin have been found in some pregnant women, dialysis patients, and people who lack sufficient biotinidase, an enzyme needed for biotin absorption (although the symptoms of biotin deficiency and biotinidase deficiency are not identical).
Toxicity There is no evidence of biotin toxicity.
Relationship to Disease Prevention Because biotin deficiency leads to thinning hair and skin sensitivity, it is included in many “hair support” vitamin products. It has been used successfully in seborrheic dermatitis in infants, but scientific evidence for a role in hair growth is lacking.
Pyridoxine (Vitamin B6)
Vitamin B6 is a water-soluble vitamin that is one of a group of compounds that includes pyridoxine and pyridoxamine, mainly found in plants, and pyridoxal, derived from animal products. All of these compounds are easily converted to pyridoxal phosphate, a coenzyme involved in the metabolism of amino acids.
Forms and Absorption Vitamin B6 and its related compounds are absorbed in the jejunum and widely distributed in the body, primarily in muscle tissue.
Functions Vitamin B6-dependent enzymes perform a number of biochemical functions, such as:
- varied reactions involving amino acids, including transamination,
- synthesis of a variety of biogenic amines, including serotonin, dopamine, norepinephrine, and histamine,
- heme synthesis,
- conversion of the amino acid tryptophan to niacin; breakdown of glycogen to glucose phosphate; and the conversion of homocysteine to cysteine.
Deficiency Vitamin B6 deficiency, while relatively rare, can occur as a consequence of an adverse interaction with the antitubercular drug, isoniazid, or penicillamine. This deficiency is characterized by cheilosis, glossitis, a pellagra-like dermatitis, depression, confusion, and EEG abnormalities.
Asthma, renal disease, Hodgkin’s disease, sickle cell anemia, and diabetes have all been associated with a decrease in the blood levels of pyridoxal phosphate. Low serum vitamin B6 levels have been observed in pregnant women experiencing nausea and supplements have been shown to be safe and effective.
Toxicity The tolerable upper intake level for vitamin B6 has been established at 100 mg/day. Reports of toxicity have been noted in individuals taking 100 to 300 mg/day. Megadoses of 500 mg/day or higher of vitamin B6 for 2 months or more can cause photosensitivity and a polyneuropathy characterized by failure of muscular coordination and sensory nerve damage.
Relationship to Disease Prevention The NIH lists vitamin B6 as “possibly effective” for upset stomach and vomiting in pregnancy, premenstrual syndrome (PMS) symptoms such as breast pain and depression, oxalate kidney stones, movement disorders (tardive dyskinesia) in people taking medicines for mental disorders, behavior disorders in children with low levels of serotonin, reducing lung cancer risk in men who smoke, and macular degeneration (see Chapter 5: Case 2). In addition, B6 in the form of pyridoxine hydrochloride, has been utilized to treat diabetes during pregnancy, carpal tunnel syndrome, asthma, depression, and diabetic neuropathy. Studies have failed to document any decreased risk of myocardial infarction in patients post-coronary artery bypass graft surgery or any decreased risk of cancer incidence in those with prior cardiovascular disease.
Vitamin B12
Vitamin B12 is a water-soluble vitamin that exists in many forms referred to as cobalamins. Cyanocobalamin is the synthetic form used in supplements. Cobalamins are produced by bacterial fermentation (e.g., in the rumen of cattle); therefore animal products and fermented foods (e.g., nutritional yeast) provide the only dietary sources.
Form and Absorption Adequate absorption of Vitamin B12 depends on the presence of stomach acid and pepsin, pancreatic proteases, intrinsic factor (IF), and IF receptors on the terminal ileum. Because there is a low (∼1 percent) rate of absorption even in the total absence of IF, individuals with B12 malabsorption (pernicious anemia) may be maintained with large oral doses of vitamin B12 (250 to 1000 µg/day) after initial parenteral loading.
Functions Vitamin B12 is a prosthetic group required for two important enzymes – methionine synthase and methylmalonyl-CoA mutase – which are essential for cell replication and neurological function. Methionine synthase is present in the cell’s cytoplasm and catalyzes the transfer of a methyl group from N-methyl-tetrahydrofolate to homocysteine to yield methionine and to liberate tetrahydrofolate. Thus it is required for folic acid metabolism and methyl group transfer reactions. Methylmalonyl-CoA mutase resides in the mitochondria and transforms methylmalonyl-CoA (from uneven numbered fatty acids) into succinyl-CoA, for further metabolic use.
Deficiency Vitamin B12 deficiency is a specific concern of those following a vegetarian dietary pattern (particularly vegans). While tempeh, miso, and sea vegetables have been shown to contain B12, absorption from these sources may not be sufficient to prevent deficiency. Individuals lacking IF fail to absorb sufficient B12 and develop pernicious anemia. Some people develop pernicious anemia as a consequence of autoimmune inactivation of IF. Others at risk include patients who have had their terminal ileum surgically removed as therapy for inflammatory bowel disease, cancer, or trauma. Patients taking proton pump inhibitors on a long-term basis may develop B12 deficiency secondary to inadequate stomach acid to release B12 from food resulting in malabsorption. Many older people develop achlorhydria and lose their ability to release B12 from protein, so they absorb less vitamin B12. Alcohol abuse also reduces absorption and is a risk factor for dietary B12 deficiency. According to the Merck Manual, less common causes of inadequate vitamin B12 absorption include chronic pancreatitis, gastric surgery, malabsorption syndromes, AIDS, and the use of certain drugs (e.g., antacids, metformin, or repeated exposure to nitrous oxide).
Symptoms of vitamin B12 deficiency include megaloblastic anemia, nerve damage (tingling in the hands and feet), and a swollen, painful red tongue. Long-term vitamin B12 deficiency, if not treated, can cause severe, irreversible damage to both peripheral nerves, such as paresthesias and numbness in the limbs, and to spinal cord tracts, causing ataxia and loss of vibration sense, and dementia. Lowered levels of vitamin B12 have been observed in those with Parkinson’s disease and recent research has demonstrated the effectiveness of B12 in reversing the sensory neuropathy associated with chronic cough.
Toxicity No toxic or adverse effects have been associated with large intake or parenteral administration of vitamin B12. When high doses of vitamin B12 are given orally, only a small percentage is absorbed, which may explain its low toxicity. There is no TUL.
Vitamin B12 is a product of bacterial fermentation. The only dietary sources of vitamin B12 are foods of animal origin such as meat, chicken, fish, eggs, and dairy products. Fortified foods, such as brewers yeast and soy milk, contain added vitamin B12. Seaweed, algae, spirulina, and fermented plant foods, such as tempeh and miso, are touted as vegetarian sources of vitamin B12 but contain only trace amounts.
Relationship to Disease Prevention When taken as a supplement along with folate, vitamin B12 resulted in improved cognitive function and memory as well as a decrease in depressive symptoms in older adults with psychological distress. Given the widespread use of medications that interfere with B12 absorption (metformin and gastric acid inhibitors), clinicians should be alert to potential symptoms of B12 deficiency in their older patients.
Folate (Folic Acid)
Folate is a water-soluble B vitamin also known as folacin or folic acid. Folate is found in both plant and animal food sources. Dietary folate in the form of the polyglutamates is digested to the monoglutamate form and actively absorbed in the jejunum.
Functions Folate plays an essential role in transferring single carbon units to acceptor molecules and thus is important for:
- synthesis of DNA and RNA, cell division, and growth and development,
- synthesis of heme for the formation of blood cells,
- serving as a methyl donor for the enzyme involved in the conversion of homocysteine to methionine.
Deficiency Folate deficiency in humans is attributed to sub-optimal dietary intake of folate, inadequate absorption (e.g., as a consequence of gluten enteropathy), inadequate utilization (e.g., from drug antagonists such as methotrexate or enzyme deficiencies), increased demands (e.g., pregnancy), or increased losses (e.g., liver disease or dialysis). Although folate deficiency is rare in the United States, it may occur in alcoholics, or individuals who are unable to absorb folate, such as those with Crohn’s disease, ulcerative colitis, or short bowel syndrome. Unlike other vitamins, the recommended amounts of folate are the same for men and women but recent evidence suggests that larger amounts might be needed in men.
Folate deficiency in the elderly may be the result of a poor diet or the use of drugs that impede the absorption of folate. Antacids hinder the absorption of folate by raising the pH levels of the upper intestine. Cimetidine, sulfasalazine, and phenytoin also impede the absorption of folate. Folate supplementation can reverse the macrocytic anemia seen in pernicious anemia; however, it will not reverse the neurologic damage caused (see vitamin B12).
A lack of folate affects cell division, resulting in abnormalities in red blood cell formation in the bone marrow. Symptoms of folate deficiency commence with macrocytosis and progress to macrocytic anemia. As the oxygen-carrying capacity of the blood gradually diminishes, symptoms such as weakness, fatigue, irritability, headache, palpitations, and shortness of breath may occur. Folate deficiency also results in elevated blood homocysteine levels. It is estimated that two-thirds of individuals with high homocysteine levels have poor folate intake.
Toxicity The TUL for folate has been set at 1 mg/day. Although folate seems to have little or no toxicity per se, the TUL was established because excessive consumption of folic acid may mask vitamin B12 deficiency, allowing neurologic sequelae to progress even though the anemia associated with this deficiency resolves.
Relationship to Disease Prevention Since folate is involved in the synthesis of DNA and proteins, adequate levels are particularly important at times of rapid cell growth, such as during fetal development. It has been demonstrated that neural tube defects occur from a dietary deficiency of folate combined with a genetic defect in enzymes involved in folate metabolism. Folate administration during the very early stages of pregnancy has been convincingly demonstrated as important in preventing many neural tube defects. Fortification of certain foods with folate has been credited with substantially reducing the incidence of neural tube defects and perhaps some other birth defects (Chapter 4: Case 2).
People with high blood levels of the amino acid homocysteine (HCys) have been shown to have an increased risk of developing heart disease. The “salvage” of HCys (a product of methylation reactions) by conversion to methionine requires methyl tetrahydrofolate; thus, a block in this reaction from inadequate folate or B12, results in elevations of HCys in the body. As vitamin B6 is required for the lone alternative pathway for HCys utilization, a lack of any of these B vitamins causes especially high levels of HCys. Therefore, researchers have suggested that increasing folate, either through the diet or supplements, will reduce HCys levels in the blood and lower the risk of heart disease as well. This beneficial effect of folate is decreased by antiplatelet medications. However, recent findings report no beneficial vascular effects in high-risk populations, suggesting that elevated HCys may be a marker of increased risk of CVD rather than a causative agent.
Folic acid has recently been shown to decrease the risk of some types of strokes in smokers. Folate has been used effectively as an adjunct in depressed patients who fail to respond to selective serotonin reuptake inhibitor (SSRI) treatment. Lower folate levels have been associated with an increased risk of depression and dementia in the elderly, and folate supplementation increased cognitive functioning in older adults. Lower folate levels have also been correlated with an increased risk of prostate cancer in men and pancreatic cancer in women.
Folate Food Sources See Appendix F.
Minerals
Mineral elements are inorganic substances that occur as salts, such as sodium chloride (NaCl), or as a component of organic compounds, such as the iron in the tetrapyrrole ring of heme (e.g., hemoglobin) or the sulfur found in certain amino acids. Minerals are classified as macrominerals or microminerals, based on their percentages of total body weight. Macrominerals constitute more than 0.005 percent of the body’s weight, or 50 parts per million (ppm). Examples include calcium, chloride, phosphorus, potassium, magnesium, sodium, and sulfur. Microminerals fall into two categories:
- Minerals with identified roles in health maintenance, including chromium, cobalt, copper, fluoride, iodide, iron, manganese, molybdenum, selenium, and zinc.
- Minerals found in body tissues with no currently established roles in health maintenance, such as arsenic, boron, cadmium, nickel, silicon, tin, and vanadium.
In foods, minerals commonly occur as salts, such as sodium chloride or as enzyme cofactors. Because salts are usually water soluble, some loss occurs during cooking, such as when vegetables are boiled. The body is capable of storing some minerals (e.g., iron in ferritin, calcium in bone) so that deficiencies may require a prolonged period of poor intake before symptoms develop.
Calcium
Calcium is an abundant mineral in the body, with 99 percent of body calcium stored in the bones and teeth. The remaining 1 percent is active in enzyme activation, blood clotting, and muscle contraction. Most calcium absorption occurs in the duodenum, but the jejunum and ileum contribute substantially to overall calcium absorption.
Vitamin D levels in the body regulate calcium absorption. The parathyroid gland responds to low serum calcium levels by releasing PTH, which stimulates many tissues to convert vitamin D to its active form (calcitriol). Activated vitamin D, in turn, increases the absorption of calcium from the intestine and regulates calcium excretion via the kidneys.
When calcium levels in the blood are elevated, the hormone calcitonin, released from the parafollicular cells (or “C cells”) in the thyroid gland, prevents bone from releasing calcium and promotes calcium excretion. Individuals who have poor vitamin D intake and low sun exposure have poor calcium absorption. Lactose, the sugar in dairy products, improves calcium absorption in infants, whereas oxalate (which is present in spinach and rhubarb) and, to a lesser extent phytate, can inhibit calcium absorption. Calcium excretion is related to dietary protein intake – high protein diets increase urinary excretion of calcium; however, protein intake accompanied by adequate calcium intake increases bone mass.
Functions Calcium plays an essential role in:
- bone mineralization; calcium levels are maintained in equilibrium by the movement of 250 to 1000 mg of calcium in and out of bone tissue every day,
- maintenance of cell membrane permeability,
- muscle contraction,
- blood clotting,
- nerve impulse conduction.
Calcium Deficiency Calcium deficiency usually remains undiagnosed for years because the bones serve as an effective reservoir and continue to release calcium into the blood. Symptoms of calcium deficiency (hypocalcemia) include irritability, “pins and needles” sensation in hands and feet (paresthesia), muscle cramps and twitching (tetany), and possible seizures (convulsions). Over time, persistent low calcium intake can manifest as osteoporosis, with accompanying bone fractures and loss of height. Calcium deficiency in children is characterized by paresthesia of the mouth or extremities, stunted growth, tetany, and seizures.
Problems related to poor calcium intake include:
- Rickets is caused most commonly by vitamin D deficiency, but lack of calcium and phosphorus can also be a basis for this disease. Rickets is characterized by abnormal bone formation, bending and distortion of the bones, nodular enlargements of the boney epiphyses, delayed closure of the fontanels, and bone pain.
- Osteoporosis is defined as a reduction in bone density, rendering bones brittle and susceptible to fractures. Symptoms of osteoporosis may include altered posture caused by deformity of the spine, postural slumping due to acute pain, waddling gait, loss of height, muscle weakness, and kyphosis. The bones most commonly affected include the hip, spine, wrist, and upper arm. A low calcium diet and lack of adequate physical activity are primary factors believed to contribute to the development of osteoporosis. Excessive alcohol intake, family history of osteoporosis, race, early menopause, short stature, and cigarette smoking are major contributors as well.
Calcium Toxicity Hypercalcemia may be seen in people with a hyperactive parathyroid gland, excessive intake of vitamin D, or certain cancers, including breast and lung cancer. Hypercalcemia may result in dehydration, lethargy, nausea, vomiting, anorexia, and possibly death. The tolerable upper limit for calcium intake has been established at 2500 mg/day. Adults with a history of calcium oxalate kidney stones should be advised to limit their protein intake to the RDA level of 0.8 g/kg bodyweight per day, avoid oxalate-rich foods, and limit salt intake.
Supplement Issues The lifetime risk for osteoporotic fractures in women is estimated to be as high as 50 percent, and costs associated with hip fracture alone are estimated at $13 to $18 billion/year in the United States. These facts combined with the exponential increases expected as the population ages, make prevention key. While osteoporosis is a multifactorial disorder, calcium intake during adolescence and throughout life and adequate vitamin D is critical to achieving optimal peak bone mass and may play a significant role in preventing degenerative bone diseases in later years. Adolescents need to be educated about the importance of calcium for health, recommended intake, and good food sources of calcium, particularly lower-fat dairy products. Calcium supplements may be helpful for populations of:
- post-menopausal women,
- amenorrheic women,
- patients who avoid dairy foods, including strict vegetarians, vegans, and lactose-intolerant persons.
Relationship to Disease Prevention Calcium supplementation to pregnant women with low calcium intakes reduces the severity of preeclampsia, maternal morbidity, and neonatal mortality. After birth, however, calcium supplementation may result in lower bone densities in the mother. In a recent research study, calcium and vitamin D supplementation did not lower blood pressure or decrease the risk of breast cancer in older women. A meta-analysis of cohort studies and clinical trials failed to show any reduction in fractures with increased calcium intake, therefore more focus on the contribution of vitamin D and phosphate in combination with calcium supplementation is required. The role of milk has also been called into question as the results of the Nurse’s Health Study failed to show that women who drank more than one serving of dairy daily (three are currently recommended to meet calcium intake requirements), had lower risk of osteoporosis. Supplementation with calcium and vitamin D has also not been shown to produce a change in lipids in the body or cause weight loss but long-term use has been associated with an increase in urinary track stones and may decrease iron absorption.
Calcium Food Sources (including fortified sources) See Appendices G, H.
Magnesium
Forms and Absorption Magnesium is absorbed primarily in the distal jejunum and ileum and is more efficiently absorbed when intake is low. Magnesium competes with calcium for absorption, and its absorption is also slightly enhanced by vitamin D. Magnesium is found in bone, muscle, and intracellular and extracellular fluid. The kidney is the principal modulator of magnesium homeostasis through filtration and reabsorption.
Only 1 percent of the body’s magnesium pool is found in the blood and magnesium is a co-factor in more than 300 enzymatic reactions.
Functions Magnesium plays a role:
- in hundreds of ATP-requiring reactions in metabolism and active transport by acting as a necessary chelator for the highly negatively charged ATP and ADP molecules,
- in transmitting neural impulses and thereby eliciting muscle contractions in conjunction with calcium, sodium, and potassium,
- as a component of bones and teeth,
- in protein synthesis and cell replication,
- in suppressing PTH secretion, although it is only about one-half as effective as calcium.
Magnesium Deficiency Although overt magnesium deficiency is rare due to its presence in a wide variety of foods, the average intake of magnesium is below what it should be for disease prevention. A study evaluating data from the NHANES study 1999–2000 found that the median daily intake of magnesium in Caucasian males was about 100 mg less than the RDA. For women the deficit was 80 mg and among ethnic minority respondents, the deficits were even greater. Deficiency can occur in individuals who have absorption or excretion problems. These conditions include intestinal malabsorption, surgical removal of the lower part of the intestine, diuretic medications, severe vomiting, and kidney disease. Individuals with protein-calorie malnutrition, chronic alcohol abuse, hyperparathyroidism, and liver cirrhosis may have low serum magnesium levels. Recent studies have documented the relationship of low serum magnesium with insulin resistance and increased risk of metabolic syndrome. Since magnesium is required for normal PTH functioning, low magnesium levels may alter calcium and phosphorous homeostasis. Magnesium is also diminished by food processing (e.g., refining grains or boiling greens).
Indications of magnesium deficiency include low levels of calcium and potassium in the blood, as well as changes in the gastrointestinal, neuromuscular, and cardiovascular systems. In patients with low serum potassium levels that seem not to rise with supplementation, a magnesium infusion allows potassium levels to be restored to normal. Magnesium deficient individuals may have fatigue, lethargy, weakness, poor appetite, impaired speech, anemia, irregular heartbeat, tremors, and failure to thrive. Clinical signs of advanced magnesium deficiency include rapid heart rate, cardiac fibrillation, and convulsions.
Hypomagnesemia was found to be common in children during to cardiac bypass surgery and was ameliorated with magnesium supplements, thus lowering post-op arrhythmias. Following either the Atkins or LEARN diet was associated with inadequate dietary intake of magnesium, so supplementation during dietary restriction for weight loss may be indicated.
Magnesium Toxicity Elevated blood magnesium levels may be seen in people with renal failure or those receiving high doses of magnesium supplements. High blood levels typically cause diarrhea and may result in changes in mental status, muscle weakness, nausea, extremely low blood pressure, difficulty breathing, and an irregular heartbeat. The tolerable upper limit for magnesium has been established at 350 mg/day for adults and adolescents.
Supplement Issues
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree